Systemic sclerosis (SSc) is a rare chronic multi-system autoimmune disease of unknown cause and a complex pathogenesis. The hallmark of the disease is microvascular vasculopathy which results in tissue ischemia with recurrent episodes of reperfusion. Diffusion-weighted (DW) Magnetic Resonance imaging (MRI) is an excellent tool for the detection of activity of any vascular or inflammatory lesions.
ObjectivesDetect brain changes in systemic sclerosis patients with asymptomatic CNS manifestations using fluid attenuation inversion recovery (FLAIR) weighted sequence and diffusion-weighted (DW) sequence MRI.
MethodsFifteen systemic sclerosis female patients aged 27–60 years old with disease duration of 1–20 years with no CNS clinical manifestations were included. A controlled group of 14 clinically normal persons, age and sex matched. Both groups were subjected to brain MR examination at 1.5T; a FLAIR weighted sequence and a DW sequence. SPSS (version 20) was used for statistical analysis.
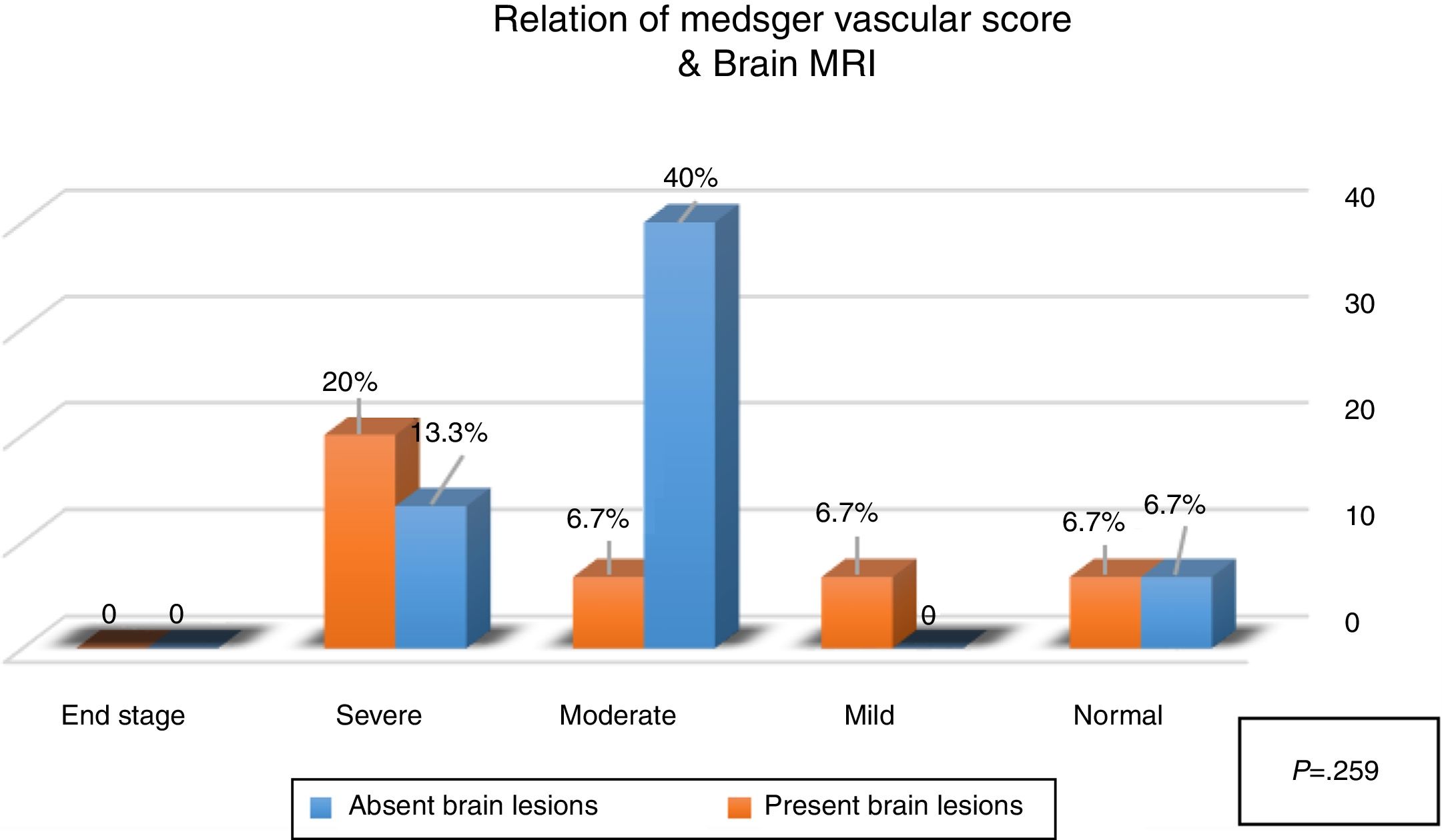
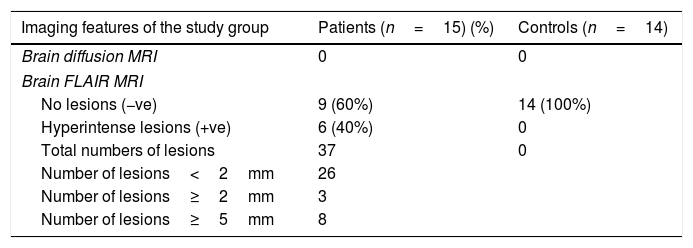
Results37 white matter hyperintense lesions (≤2 to ≥ 5mm in diameter) were detected in patient group using FLAIR weighted MRI while diffusion-weighted MRI failed to detect the same lesions. A non-significant relation (P=.259) between the presence of white matter hyperintense lesions and the severity of peripheral vascular affection of the disease was observed.
ConclusionsAsymptomatic central nervous system vasculopathy is detected in systemic sclerosis using FLAIR MRI, while diffusion MRI failed to detect such lesions. These findings suggest a non-inflammatory form of central nervous system microvasculopathy in SSc patients.
La esclerosis sistémica (SSc) es una rara enfermedad crónica autoinmune multisistémica de causa desconocida y una patogénesis compleja. El sello distintivo de la enfermedad es la vasculopatía microvascular que se traduce en isquemia tisular con episodios recurrentes de reperfusión. La resonancia magnética (RM) ponderada por difusión (DW) es una excelente herramienta para la detección de la actividad de cualquier lesión vascular o inflamatoria.
ObjetivosDetectar cambios cerebrales en pacientes con SSc con manifestaciones del sistema nervioso central (SNC) asintomáticas utilizando FLAIR y DW-RM.
MétodosQuince pacientes con SSc sin manifestaciones del SNC incluidos. Un grupo de 14 personas sanas estandarizadas por edad y sexo en el grupo de pacientes como grupo de control. La RM cerebral se hizo para obtener ambos grupos (pacientes y control) en 1,5T. La prueba de Chi-cuadrado y la prueba de correlación de Spearman SPSS® (versión 20) se utilizaron para el análisis estadístico.
ResultadosSe detectaron 37 lesiones hiperintensas de materia blanca (≤2-≥5mm de diámetro) en el grupo de pacientes que utilizaron RM ponderada con FLAIR, mientras que la DW-RM no detectó las mismas lesiones. Se observó una relación no significativa (p=0,259) entre la presencia de lesiones hiperintensas de la materia blanca y la severidad del afecto vascular periférico de la enfermedad.
ConclusionesLa vasculopatía del SNC asintomática se detecta en la SSc mediante la RM de FLAIR, mientras que la RM de difusión no detectó tales lesiones. Estos hallazgos sugieren una forma no inflamatoria de la microvasculopatía del SNC en pacientes con SSc.
Systemic sclerosis (SSc) is a rare chronic autoimmune disease, with multi-organ affection, of unknown cause and a complex pathogenesis. This multi-system affection exhibits evidence of inflammation, vasculopathy, autoimmunity, and fibrosis.
The major pathologic components of SSc are vascular disease and progressive fibrosis. The vasculopathy is either microvascular (which is the hallmark of the disease) or macrovascular, resulting in tissue ischemia with recurrent episodes of reperfusion.1–4
Diffusion-weighted Magnetic Resonance (MR) imaging (DWI) is an advanced MR imaging technique, which allows non-invasive evaluation of water diffusibility in brain tissue, as first described by Stejskal and Tanner in 1965.5–8 DWI is sensitive to the random translational motion of water molecules due to Brownian motion. Diffusion weighted images (DW-images) are generated by adding an opposing pair of diffusion gradients to spin-echo or echo planar imaging sequences. For stationary molecules, the effects of the first (tagging) and the second (un-tagging) gradient pulses cancel each other out. For mobile, diffusible molecules there is incomplete rephrasing resulting in a net phase shift, which leads to a signal loss. In practice, tissue with restricted diffusion will appear hyperintense to normal tissue on DW-images.5,6
During the last few years, DWI has been shown to be an excellent tool for the detection of acute stroke (gives us an idea about the ischemic and salvageable area to guide the management). As well as activity of any vascular or inflammatory lesions (e.g. vasculitis or vasculopathy) where DWI can detect small and active changes and differentiate ischemic disease process from others. Furthermore, old brain lesions (3–6 months old), where tissues were deprived from blood supply, appear as hypointense lesions (different shades of gray to black) in a radiologic terminology called encephalomalacia.9–14
Material and methodsFifteen patients, diagnosed according to the American College of Rheumatology (ACR) criteria for the diagnosis of systemic sclerosis,15 attending the Rheumatology, Rehabilitation & Physical medicine outpatient clinic in Assiut University Hospitals were studied.
The study protocol was approved by the Ethics Review Board of Faculty of Medicine, Assiut University, and informed consent was obtained from all participants according to the Declaration of Helsinki.
Their ages ranged between 27 and 60 years (42±10.18), with disease duration between 1 and 20 years (7.8±6.8). All patients were subjected to full history taking, clinical and basic laboratory evaluation (CBC, ESR, liver function tests, kidney function tests, fasting blood sugar, and lipid profile) in addition to pulmonary function tests, and echocardiography. Radiological evaluation and imaging using plain chest radiographs, high-resolution CT chest, and abdominal ultrasound were also done. The Medsger scale of disease severity was used.16 None of the patients had any history of cerebrovascular accidents, head trauma, or clinical evidences of neuropsychiatric disease.
Patients who suffered severe or uncontrolled arterial hypertension, uncontrolled diabetes mellitus, renal, hepatic, or respiratory failure were excluded from the study.
Fourteen healthy volunteers, sex and age matched with the studied group, were enrolled in the study serving as a control group.
Both groups were subjected to brain MR examination at 1.5T (Achieva, Philips, Netherlands). After centering with a three-step scout (axial, coronal, and sagittal), an axial spin echo, FLAIR weighted sequence was acquired with the following technical parameters: time of repetition/time of echo=11,000/140, matrix 232/512; field of view 230mm with thickness of 5mm (1mm gap), for a total of 23 images with NSA 2. The FLAIR images were used for counting focal brain abnormalities in both patients with SSc and the CG. The FLAIR is higher sensitive sequence for periventricular lesions in white matter than other weighted images. Diffusion weighted sequence performed as echo-planar sequence in following parameters; time of repetition/time of echo=3773/117, matrix 152/256; field of view 230mm with thickness of 5mm (1mm gap), for a total of 23 images with NSA 1 and EPI factor 55. The DW images were acquired in 0 and 1000s/mm2 and the diffusion gradients applied simultaneously in three orthogonal spatial directions.
These images were evaluated by the radiologist. He counted the white matter hyperintensities in all brain regions. All the abnormalities were electronically measured (along the longest diameter) to distinguish the lesions ≥2mm or less.
For statistical analysis, data was analyzed by using the advanced Statistical Package for Social Sciences (SPSS) program version 20. Chi-square test and Spearman's correlation test was used to examine the relation and correlation between continuous variables. P-Value was considered statistically significant when it was ≤.05.
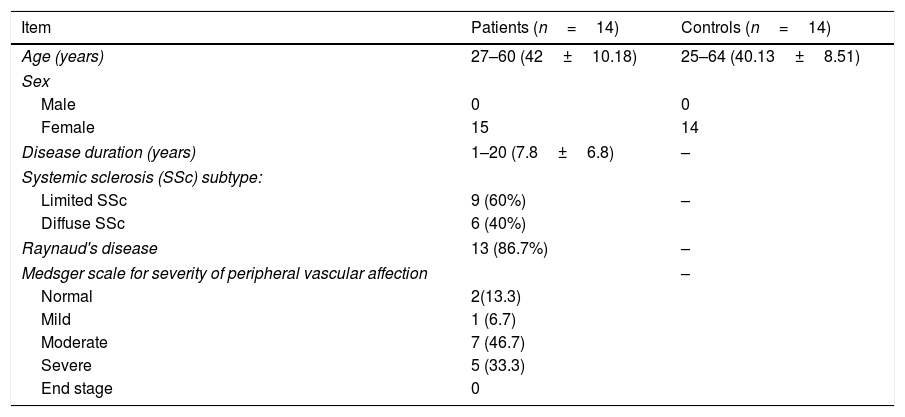
ResultsAll patients were females. Nine of them had limited SSc (60%), while the rest of them had diffuse type (40%).
Thirteen patients (86.7%) suffered peripheral vascular affection (Raynaud's disease) as 7 of them (46.7%) had moderate vascular affection, while 5 patients (33.3%) suffered severe vascular affection and one patient (6.7%) had mild peripheral vascular affection according to Medsger SSc severity scale (Table 1).
Demographic and clinical data in study and control groups.
| Item | Patients (n=14) | Controls (n=14) |
|---|---|---|
| Age (years) | 27–60 (42±10.18) | 25–64 (40.13±8.51) |
| Sex | ||
| Male | 0 | 0 |
| Female | 15 | 14 |
| Disease duration (years) | 1–20 (7.8±6.8) | – |
| Systemic sclerosis (SSc) subtype: | ||
| Limited SSc | 9 (60%) | – |
| Diffuse SSc | 6 (40%) | |
| Raynaud's disease | 13 (86.7%) | – |
| Medsger scale for severity of peripheral vascular affection | – | |
| Normal | 2(13.3) | |
| Mild | 1 (6.7) | |
| Moderate | 7 (46.7) | |
| Severe | 5 (33.3) | |
| End stage | 0 | |
A total of 37 of white matter hyperintense (WMH) lesions were detected in the patients group; 26 lesions <2mm and 11 lesions ≥2mm (8 of them were ≥5mm in diameter), using the FLAIR MRI. The number of lesions in one patient ranged between one solitary lesion to 18 WMH lesions.
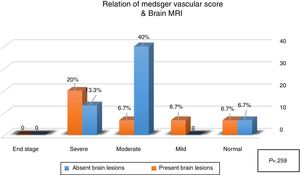
Six patients (40%) showed brain lesions using FLAIR MRI (in different supratentorial deep and subcortical brain regions (Table 2, Figs. 1 and 2). Three (20%) of them had severe peripheral vascular affection, while each of the remaining patients had mild, moderate or no peripheral vascular affection. Diffusion weighted MRI failed to detect any hypo- nor hyper-intense lesions (Table 2). A non-significant relation (P=.259) between the presence of WMH lesions and the severity of peripheral vascular affection of the disease (Medsgar Vascular Score) (Fig. 3), as well as non-significant strong correlation was found (r=0.085, P=.764) was also observed.
Imaging features of the study groups, comparing both MRI techniques (FLAIR/DWI) among patinets and controls.
| Imaging features of the study group | Patients (n=15) (%) | Controls (n=14) |
|---|---|---|
| Brain diffusion MRI | 0 | 0 |
| Brain FLAIR MRI | ||
| No lesions (−ve) | 9 (60%) | 14 (100%) |
| Hyperintense lesions (+ve) | 6 (40%) | 0 |
| Total numbers of lesions | 37 | 0 |
| Number of lesions<2mm | 26 | |
| Number of lesions≥2mm | 3 | |
| Number of lesions≥5mm | 8 | |
−ve: absence of lesions; +ve: presence of lesions.
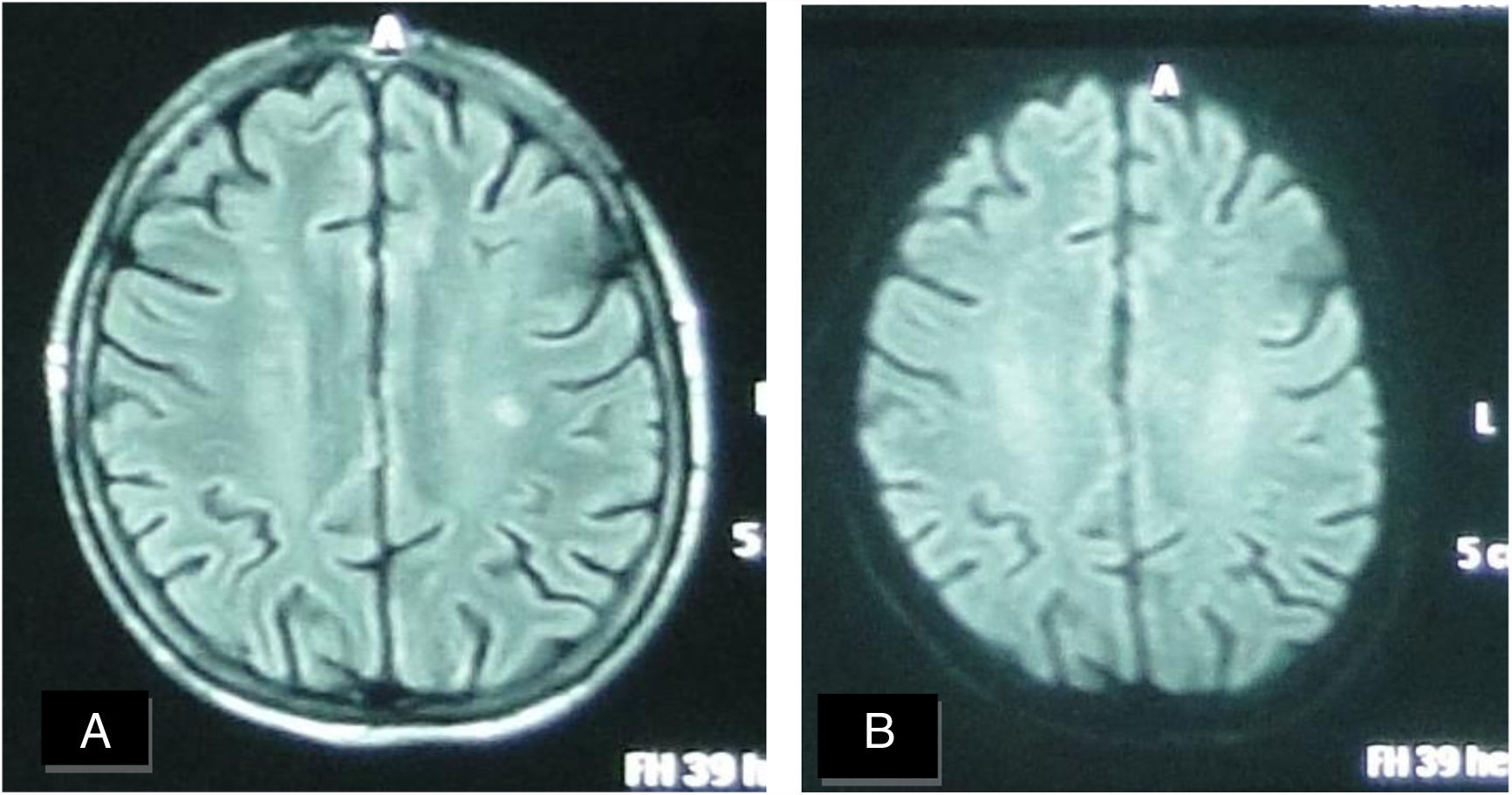
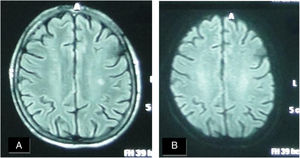
A female patient aged (27 years) and suffered from SS since (3 years). (A) FLAIR MRI shows a rather-defined single hyperintense signal lesion seen at deep periventricular white matter of the parietal regions with no comparable signal abnormality on DWI (B) suggesting late subacute to chronic ischemic lesions.
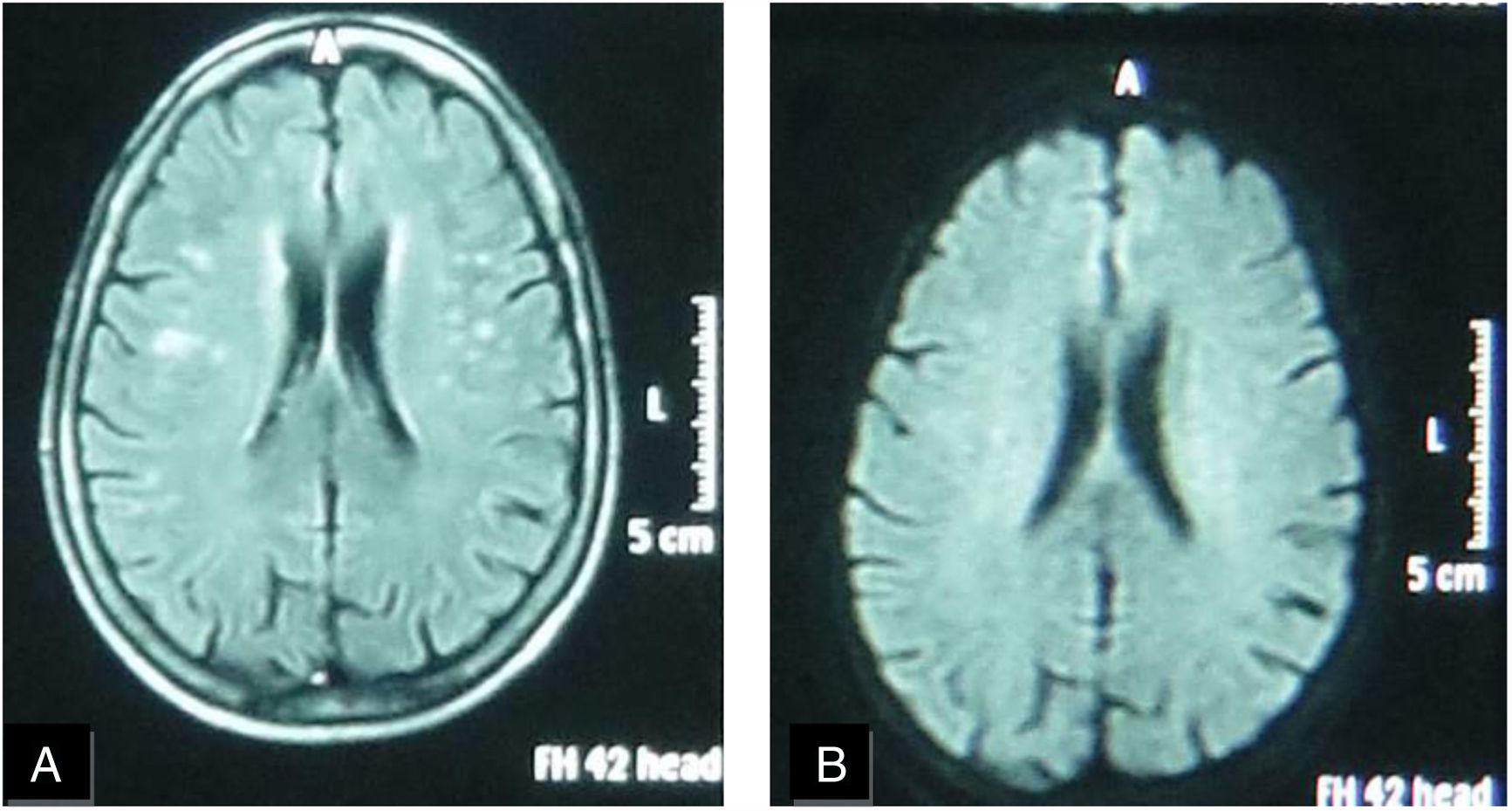
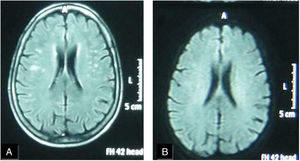
A female patient aged (60 years) and suffered from SS since (4 years). (A) FLAIR MRI shows multiple rather-defined hyperintense signal foci seen at deep periventricular white matter of both parietal regions with no comparable signal abnormality on DWI (B) suggesting late subacute to chronic ischemic lesions.
None of the control group showed any visible white matter lesion in either MRI techniques.
DiscussionSystemic sclerosis represents a complex autoimmune collagen disease that is characterized by multisystem affection. Central nervous system (CNS) involvement is known to be rare and unusual in such disease and is claimed to be related to the disease complications.17–19 This rarity was attributed to the limited presence of extracellular matrix collagens in cerebral tissue with the following sparing of media and adventitia of cerebral arteries and so, the limited progression of vascular obliteration.20–22
On the base of the high sensitivity of MRI to detect different vascular insults in the brain, we aimed to evaluate silent brain affection in SSc patients using two different MRI techniques (FLAIR and DW). The current study detected brain changes in SSc patients with asymptomatic CNS manifestations using FLAIR sequence, while diffusion MRI failed to detect the same lesions. The FLAIR technique results (in the matter of site and size of the lesions), were found to be consistent with the results of different studies.22–25 These white matter hyperintenisty (WMH) lesions where considered by the radiologist to be a definite sign of previous microvascular insults (ischemic demyelination), which additionally supports the ischemic non-inflammatory microvasculopathy theory of brain injury in these patients.23,24
Unfortunately, the completely negative DW images could not support the previous theory, as it was expected to find evidences of brain vascular insults in form of hypointense lesions that correspond to hyperintense lesions seen in FLAIR films. In year 2000, Oppenheim and her team, also found false negative DW MRI results in patients suffering acute ischemic stroke, especially transient ischemic attacks which remained negative even in their follow up DW Images.12,13 These findings can support ours in the light of the resemblance between transient ischemic attacks and the reperfusion that happen in microangiopathy in SSc, besides the limited presence of extracellular matrix collagens in the cerebral tissue, sparing of cerebral arteries media & adventitia.20,21
Furthermore, these negative DW images may be due to technique issue where the lesions are too small to be detected by DWI (of 1.5T magnet) not by the FLAIR images, based on the fact the FLAIR with high spatial resolution displayed a signal abnormality in half the lesions that were not visible on DWI.12,13
Although the results showed non-significant very weak correlation (r=0.085) between presence of brain MRI findings and presence of peripheral microvascular involvement, but we could not exclude the cerebral ischemic microvasculopathy, as multiple WMH were greater in SSc patients with cerebral hypoperfusion.24–26
This study had some limitations, such as small number of examined patients, the absence of detailed psychologic and intellectual evaluation which might give us an idea about their relationship with small infarcts detected by conventional MRI. In addition to some limitations of DWI technique used, as it is susceptible to false-negative images especially when small punctate infarcts are present in proximity to skull base. Also, the imaging plane (axial or coronal) which comes on the expense of decreased signal-to-noise ratio and increased imaging time and a clear diagnostic benefit that still to be proven, as well as the Magnet power (3T DWI is better than 1.5T DWI).13,27–29
It is concluded that asymptomatic CNS vasculopathy is detected in systemic sclerosis using FLAIR MRI, while diffusion MRI will not be cost effective to detect such lesions. Furthermore, these findings suggest a non-inflammatory form of CNS microvasculopathy in SSc patients and we recommend further research work associating intellectual and psychological affection of such CNS asymptomatic patients with imaging finding.
FundingNo funding was received.
Conflicts of interestThe authors declare no conflicts of interest.
We acknowledge all the subjects who participated in this work and made it possible.