We present the first reported case of juvenile Systemic Lupus Erythematosus with Klinefelter's syndrome in a 14-year-old Iranian boy who had leg ulcers and arthritis. He had low level of testosterone accompanied with hypergonadotropic hypogonadism. This case emphasizes the importance of two X chromosomes as a risk factor for Systemic Lupus Erythematosus in women and men with Klinefelter's syndrome (47, XXY).
Presentamos el primer caso notificado de lupus eritematoso sistémico de inicio juvenil junto con un síndrome de Klinefelter en un niño iraní de 14 años de edad que presentaba úlceras en piernas y artritis. Presentaba valores reducidos de testosterona acompañados con hipogonadismo hipergonadotrópico. Este caso resalta la importancia de dos cromosomas X como factor de riesgo de lupus eritematoso sistémico en mujeres y hombres con el síndrome de Klinelfelter (47, XXY).
Klinefelter's syndrome is the most frequent major abnormality of sexual differentiation in men and affects one in every 500–1000 born males.1 Men with Klinefelter's syndrome have more than one X chromosomes, usually two X chromosomes (47-XXY). The phenotype is characterized by eunuchoid appearance, increased length of legs and arms, scanty facial and body hair, gynecomastia, small and firm testes, and hyperpigmentation of the lower extremities.2 Hormonally, the syndrome is characterized by hypergonadotropic hypogonadism in which testosterone level is usually half of normal.2,3 Patients with Klinefelter's syndrome show a higher percent of Systemic Lupus Erythematosus (SLE) and other skin-related autoimmune diseases than the normal population. SLE may be a presenting symptom of Klinefelter's syndrome and may lead to diagnosis of the disease.4 Here we present a case of juvenile Systemic Lupus Erythematosus with Klinefelter's syndrome and most probably the first report from Middle East.
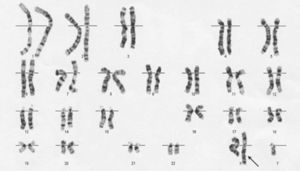
Case reportA 14-year-old Iranian boy presented to our department with a 3-week history of arthritis on both of his wrists and ankles, accompanied by myalgia and photosensitivity. His physical examination revealed butterfly rash, palmar and plantar erythema, and some small ulcers on his legs. He had low head hair implantment, and hyperpigmentation on face. Other physical findings were gynecomastia, pectus excavatum, small and firm testicles, and long extremities. The results of his laboratory investigations were as follows: white blood cell count 4.2×103/mm3 (neutrophils 72%, lymphocytes 24%, monocytes 4%), red blood cells count 424×104/mm3, platelets count 140×103/mm3, hemoglobin 11.3g/dL, hematocrit 34.1%, erythrocyte sedimation rate 84mm/h, aspartate amino transferase 37U/L, alanine aminotransferase 31U/L, lactate dehydrogenase 232U/L, creatine kinase 67U/L, aldolase 5.6U/L, blood urea nitrogen 27mg/dL, creatinine 0.9mg/dL, total protein 7.4g/dL, antinuclear antibody (positive > 1:160 homogeneous pattern), rheumatoid factors (positive +2), C-reactive protein (positive 17mg/L), C3 54mg/dL, C4 11mg/dL, IgG 2210mg/dL, IgM 220mg/dL, IgA 191mg/dL, and IgE 500mg/dL. His urine analysis revealed proteinuria 750mg/1000ml of urine collection. Results of other blood tests were within normal limits or negative, including lupus anticoagulant, β2-glycoprotein, anticardiolipin IgG and IgM Abs, anti-RO, anti-LA, anti-SM Ab, P & C-ANCA, VDRL, TSH, FT4, anti-T microsomal, antithyroglobulin, cryoglobulins, hepatitis C antibodies, hepatitis B antigen, protein C activity, and protein S free. According to American College of Rheumatology criteria for SLE, he was diagnosed as having juvenile Systemic Lupus Erythematosus.5 His renal biopsy showed mesangial glomerulitis (World Health Organization Class II).6 On admission, his endocrinological work-up discovered luteinizing hormone (6.9mIU/mL [normal range for men 1–6mIU/mL]), follicle stimulating hormone (22mIU/mL [normal range for men 1.4–15.4mIU/mL]), and testosterone (0.2ng/ mL [normal range for men 2.5–9ng/mL]), which indicate hypergonadotropic hypogonadism. His Karyotyping revealed 47 XXY karyotype, which is diagnostic of Klinefelter's syndrome (Fig. 1). He was treated with oral prednisone, Azathioprine, and hydroxychloroquine sulfate. At the same time, the patient was given intra-muscular testosterone once monthly for 1 year. Blood tests were performed for follow-up of the immune state, which were all within normal limits.
DiscussionKlinefelter's syndrome can present at any age. In adult men, the diagnosis may be made during investigation for sterility, but, at puberty, eunuch body might be the hallmark. Children with Klinefelter's syndrome might be diagnosed because of learning difficulties or social problems. Klinefelter's syndrome and SLE occur together more often than would be expected by chance alone.7 Studies have shown a clear relationship between low levels of testosterone and high prevalence of ulceration in patients with Klinefelter's syndrome. Treatment with testosterone leads to improvement of leg ulcers in these patients.8 Our patient showed both leg ulcers and low level of testosterone, whose leg ulcers were also reduced during subsequent therapy that included testosterone.
Males with untreated hypogonadism, associated with significant gonadal failure and very low levels of testosterone, have an increased risk of developing rheumatoid/autoimmune diseases. In fact, testicular dysfunction predisposes to the development of rheumatoid/autoimmune diseases. These patients have an increased frequency of antinuclear antibody and anticardiolipin antibodies compared with other hypogonadotropic hypogonadic patients.9 Although, our patient's sera were not positive for anticardiolipin antibodies, it was positive for antinuclear antibody (positive > 1:160 homogeneous pattern). SLE may be a presenting symptom of Klinefelter's syndrome and may lead to diagnosis of the disease. The first presentation of our patient was arthritis, myalgia, and photosensitivity. However, his follow-up revealed hypergonadotropic hypogonadism and his karyotype confirmed the diagnosis of Kelienfelter's syndrome.
Humoral and cellular immunities are enhanced in Klinefelter's syndrome, as a result of testosterone deficiency and increased levels of estradiol, which enhance autoantibody production. Treatment with testosterone has also proved to suppress both cellular and humoral immunities in these patients.9,10
ConclusionThe frequency of Klinefelter's syndrome is increased in men with SLE compared with its prevalence in men without SLE. Therefore Klinefelter's syndrome and SLE might be associated. Whereas Klinefelter's syndrome in children is often subclinical, the pediatric rheumatologists treating male children with lupus should be aware of Klinefelter's syndrome and provide them access to imperative medical management.