A 67-year-old female with a history of ovarian cancer presented with progressive dysphagia and muscle fatigue. Dermatomyositis (DM) was diagnosed three months earlier based on characteristic cutaneous lesions (Fig. 1) and elevated creatine kinase (3058U/L) and C-reactive protein (93mg/L) levels. Initial treatment with corticosteroids and intravenous immunoglobulin provided transient improvement in cutaneous symptoms, but dysphagia persisted.
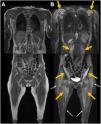
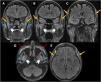
Whole-body magnetic resonance imaging (MRI, Fig. 2) revealed diffuse muscle edema consistent with active DM. Brain MRI (Fig. 3) ruled out central causes and demonstrated an unusual finding of bilateral edema of the masticatory muscles.
Diagnosis and developmentWhole-body MRI revealed diffuse muscle edema consistent with active DM and an unusual finding of bilateral masticatory muscle edema, correlating with chewing and swallowing difficulties. Brain MRI ruled out central causes, confirming that masticatory muscle involvement was the likely cause of symptoms. Despite immunosuppressive therapy, the patient required nasogastric nutritional support.
DiscussionDM primarily affects proximal limb muscles, and MRI findings such as diffuse edema and the “honeycomb” pattern are associated with severe disease, especially in paraneoplastic cases.1,2 However, masticatory muscle edema has not been previously described.3 One hypothesis suggests a selective autoimmune phenomenon affecting highly active muscle groups, while another considers an atypical inflammatory infiltration in paraneoplastic DM.4 The correlation with dysphagia suggests MRI could aid in evaluating refractory symptoms.5 Recognizing this atypical manifestation may influence therapeutic decisions and highlights the importance of detailed imaging in persistent cases. Further studies are needed to determine the prevalence and clinical significance of masticatory muscle involvement in DM. This case expands the spectrum of DM-related muscle involvement and reinforces the role of MRI in detecting atypical patterns (Figs. 1–3).
Patient's skin lesions. Erythematous cutaneous eruptions on the chest, shoulders, posterior neck, and dorsal region (A and B, white arrows), consistent with the “shawl sign.” Gottron's papules (C) with elevated lesions on extensor surfaces, including the interphalangeal (dashed dark blue arrows) and metacarpophalangeal (dashed dark blue circles) joints of the hands.
Whole-body MRI in coronal T1-weighted (A) and STIR-weighted (B) images. Relatively symmetrical, bilateral edema of the proximal musculature (orange arrows), primarily in the scapular and pelvic regions, as well as in the paraspinal muscles. No significant atrophy was identified. Minimal subcutaneous stranding was also noted (white arrows).
Brain MRI in fluid-attenuated inversion recovery (FLAIR sequence) – coronal (A–C) and axial (D, E) images. Notable bilateral and symmetrical edema of the masticatory muscles, involving the superficial temporalis (orange arrows), masseters (blue asterisks), and pterygoids (white head arrows). Cosmetic filling material was present in the anterolateral facial subcutaneous (red dashed arrows).
Full consent was obtained from the patient for the case report publication.
Funding informationNone.
Conflict of interestThe authors declare no conflicts of interest related to this publication.
The authors have no acknowledgments to declare.