A 57-year-old man with longstanding ankylosing spondylitis (AS) was treated successfully with etanercept since January 2006, except for persistent left elbow swelling. Three local corticosteroid injections and radiosynovectomy with 3mCi 186-Rhenium proved to be useless. Elbow involvement is sporadically seen in AS,1 and the persistence despite the intra-articular treatment made us consider the possibility of a coexistent arthropathy, such as an opportunistic infections (mycobacteria, fungi), synovial sarcoma, joint metastasis or lipoma arborescens. A first magnetic resonance imaging (MRI) was ordered, showing an unspecific synovial hypertrophy. Joint aspiration revealed an inflammatory non-hemorrhagic fluid with repeatedly negative cultures, and an open biopsy resulted in non-specific synovitis, ruling out infections and malignancies. In June 2010, an X-ray highlighted the development of bone erosions. A new MRI (Fig. 1) demonstrated at this time an enhancing soft-tissue mass with magnetic susceptibility effect of hemosiderin on T2*-weighted imaging, associated with subchondral bone cysts and extrinsic erosions. Surgical synovectomy was requested, and histopathologic examination noted villonodular hyperplasia and multiple multinucleated macrophages laden with hemosiderin, characteristic features of pigmented villonodular synovitis (PVNS).
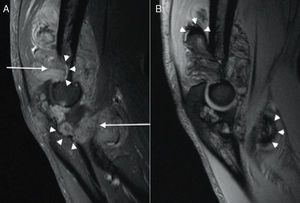
(A) Sagital T1 Fat-saturated image of the left elbow after intravenous gadolinium administration, showing an enhancing soft-tissue mass (arrows) associated to bone erosions (arrowheads). (B) Sagital T2* weighted image, showing areas of marked low signal intensity (arrowheads) suggestive of hemosiderin deposits.
PVNS is a rare neoplastic-like pathological entity of unknown etiology affecting the synovium of the joint, tendon or bursa.2 It is usually a monoarticular process carrying with pain, swelling – often mild and intermittent – and progressive decreased range of motion. It affects in decreasing order of frequency the knee, hip, ankle, and shoulder, while elbows are rarely involved.3 MRI findings are highly suggestive of the diagnosis, as the characteristic low signal intensity on T2*-weighted sequences relates to the hemosiderin-laden macrophagic infiltrate seen on histological specimens,4 which is an important aid to the clinician to make differential diagnosis with other entities showing identical clinical picture, such as synovial or fibrous tumors, amyloid deposits and proliferative processes. Nonetheless, similar MRI features could be found in other hemorrhagic and chronic hyperplastic synovial disorders (as in rheumatoid arthritis, arthropathy secondary to hemorrhagic diathesis, chronic articular traumatism, haemangioma, synovial sarcoma), making the histological confirmation unavoidable.5
In our case, the coexistence with a known cause of inflammatory arthritis, as well as the negative results of the previous techniques, delayed the final diagnosis. Although it has been published improvement of PVNS with TNFa blockade,6 our patient did not experience any benefit during etanercept treatment prescribed for his ankylosing spondylitis.
For the realization of this work has not received any funding.