Rheumatoid arthritis (RA) is the most frequent chronic polyarthritis. The current goal of RA treatment is to achieve clinical remission.
ObjectiveThe goal of this study was to determine the prevalence of remission in a cohort of patients from clinical practice, and to identify potentially modifiable factors associated with remission.
MethodsA retrospective study was performed on a cohort of RA patients seen at the first consultation at the HUGC Rheumatology Service Dr. Negrín (HUGCDN) between first of January 2000 and thirtieth of April 2014. Sustained remission was defined as DAS28 less than 2.6 in the last two available visits in the medical history.
ResultsA total of 463 patients were consecutively included, most (75%) women, with a mean age at the onset of RA of 50 years and a mean duration of the disease at follow-up of 8 years. 46% of the patients achieved sustained remission. Multiple logistic regression analyses found male sex (P=.031, OR 1.7, 95% CI 1.05–2.82), diagnosis in the first year of symptoms (P=.023, OR 1.7, 95% CI 1.07–2.69) and the initial DAS28 (P=.035) to be independent predictors for sustained remission.
ConclusionsThe 46% of the patients with RA followed in the HUGC Dr. Negrín are in persistent remission, being the early diagnosis a modifiable factor predictor of remission. Thus, an objective of the Rheumatology Service should be to improve the diagnostic delay of RA in the health area.
Introducción La artritis reumatoide (AR) es la poliartritis crónica más frecuente. El objetivo actual del tratamiento de la AR es lograr la remisión clínica.
ObjetivoEl objetivo de este estudio fue determinar la prevalencia de la remisión en una cohorte de pacientes de la práctica clínica, e identificar factores potencialmente modificables asociados con la remisión.
MétodosSe realizó un estudio retrospectivo en una cohorte de pacientes con AR observada en la primera consulta del Servicio de Reumatología del Hospital Universitario de Gran Canaria Dr. Negrín (HUGCDN) entre el primero de enero de 2000 y el 30 de abril de 2014. La remisión mantenida se definió como DAS28 menor de 2,6 en las 2 últimas visitas recogidas en la historia clínica.
ResultadosSe incluyeron consecutivamente 463 pacientes, la mayoría (75%) mujeres, con una edad media al inicio de la AR de 50 años y la duración media de la enfermedad en el seguimiento de 8 años. El 46% de los pacientes alcanzaron la remisión sostenida. Los análisis de regresión logística múltiple encontraron que el sexo masculino (p=0,031; OR: 1,7; IC del 95%: 1,05-2,82), el diagnóstico en el primer año de síntomas (p=0,023; OR: 1,7; IC del 95%: 1,07-2,69) y el DAS28 inicial (p=0,035) fueron factores predictores independientes de remisión sostenida.
ConclusionesEl 46% de los pacientes con AR seguidos en el HUGCDN están en remisión persistente, siendo el diagnóstico precoz un factor predictor modificable de la remisión. Así, un objetivo del servicio de reumatología debe ser mejorar el retraso diagnóstico de la AR en el área de salud.
Rheumatoid arthritis (RA) is the most frequent chronic inflammatory disease, affecting 0.5%–1% of the European and North American population. Its prevalence in Spain and in the Canary Islands is 0.5%.1 RA is characterized by persistent joint inflammation associated with further joint damage and disability. Not only the development of new drugs, but also the early diagnosis and treatment, provides better control of the disease and better long-term prognosis. The goal of RA treatment of the lowest disease activity possible has improved the results compared to the classic management. The treat to target strategy has a goal defined as clinical remission or low disease activity. The evaluation scales and their remission criteria have been in continuous revision, because depending on the index that is being used, patients with the same activity may obtain different punctuations. The purpose of this study was to determine the prevalence of clinical remission in a “real life” cohort of RA patients and identify factors associated with clinical remission, since knowing modifiable factors associated with remission could help achieve clinical outcomes.
PatientsData was collected from 463 patients. It was an observational, retrospective, realworld cohort of patients with RA recruited at the Rheumatology division of the HUGCDN since the first of January 2000 until the thirteenth of April 2014. Inclusion criteria were patients older than 18 years, diagnosed RA according to 2010 ACR/EULAR classification criteria and with available follow-up data of a minimum of two years after the basal visit.
Measures and Data CollectionThere were patients referred by the primary care doctor to the Hospital, patients from the emergency department or referred by other hospital units. Data was collected between January 2013 and April 2014. The baseline characteristics, included sex, age, history of smoking and alcohol intake and medical comorbidities (osteoporosis, hypertension, ischemic heart disease, heart failure, infarct, chronic obstructive pulmonary disease, asthma, depression and diabetes). Clinical data of RA: 28 and 44 joint counts, general health and pain in visual analog scale (VAS) and morning stiffness. Patients completed the health assessment questionnaire disability index (HAQ-DI). Blood tests that included erythrocyte sedimentation rate (ESR), C reactive protein (CRP), hemoglobin levels and serology including rheumatoid factor (RF) and anti cyclic citrullinated peptide antibody (ACPA) level. 28 count disease activity scores (DAS28) index was calculated. Baseline hand and foot radiographic findings and previous and current treatments were also collected. All data was collected from outpatient medical records. Serum RF was measured by a quantitative immunoturbidimetric assay, and the positive results were defined as a value of more than 14YIU/ml. Laboratory test for ACPA level measurement has been introduced into HUGCDN since 2007, so some patients diagnosed RA before that time never took this blood test. The significant changes of radiographic findings included narrowing of joint space or erosions compatible with RA, which were reported in medical records by the rheumatologists or reported by radiologists. In the follow-up visits, 28 and 44 joint counts, VAS GH, VAS pain and morning stiffness, blood tests that included hemoglobin, ESR, CRP and annual hand and foot X-rays were parameters also collected. Incidental comorbidities, and current and new treatments were noted. Disease activity was assessed from DAS28 which was calculated using the original formula with 28 swollen joint count, 28 tender joint count, ESR and VAS GH. Clinical sustained remission was defined as DAS28<2.6 in the last two consecutive visits. Low, moderate, and high disease activity states were defined as DAS28≤3.2, >3.2 but ≤5.1 and >5.1, respectively. The improvement criteria used in this study was the EULAR response criteria. The good responders were patients who had a decline of DAS28 at least 1.2 units from baseline and low disease activity. Moderate responders were patients with a change ≥1.2 and moderate/high disease activity or patients with a change ≤1.2 and >0.6 and low/moderate disease activity, others were nonresponders.
Statistical AnalysisStatistical analyses were performed using SPSS V.16.0 statistical software. Baseline characteristics with continuous data were reported as means±standard deviation (SD), and the categorical data was shown as frequencies and percentages. To test the differences between groups, the Mann–Whitney U test or the independent samples t test was used for continuous variables, and the X2 test for proportions. A stepwise multiple logistic regression model was used to find relevant independent prognostic variables. The variables included in the multivariate model were selected using univariate analysis (P<.05). The results were presented as the odds ratio (OR) with corresponding 95% confidence interval (95% CIs).
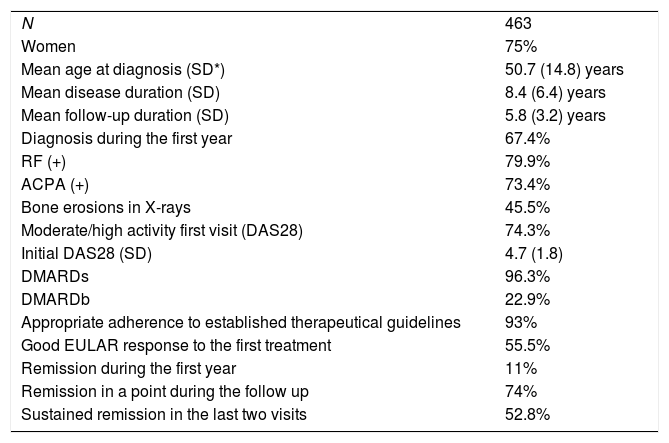
ResultsFour hundred and sixty-three RA patients were included. Baseline characteristics of the whole cohort of patients (n=463) are shown in Table 1. 75% of patients were female and mean age at diagnosis was 51 years. Mean disease duration was 8 years and mean follow-up time was 5.8 years. Most of the patients were positive RF and ACPA. Almost half of the patients had erosions in X-rays. The most frequent comorbidities were HTA (31%), dislypidemia (25%) and osteoporosis (14%). History of smoking was recorded in 49 patients and there were 77 current smokers. Regarding to extraarticular manifestations, 38 patients had rheumatoid nodules and 14 secondary Sjögren Syndrome. More than 70% of the patients were in moderate/high disease activity in the first visit. Mean DAS28 value was 4.7. At first visit, 5% of the patients were in clinical remission using DAS28. 96% of the patients received synthetic disease modifying antirheumatic drugs (DMARDs) and 23% received biologic synthetic disease modifying antirheumatic drugs (DMARDb). 72% of the patients achieved remission in unless one visit and 214 patients achieved sustained remission (Table 1).
Baseline Cohort Characteristics.
| N | 463 |
| Women | 75% |
| Mean age at diagnosis (SD*) | 50.7 (14.8) years |
| Mean disease duration (SD) | 8.4 (6.4) years |
| Mean follow-up duration (SD) | 5.8 (3.2) years |
| Diagnosis during the first year | 67.4% |
| RF (+) | 79.9% |
| ACPA (+) | 73.4% |
| Bone erosions in X-rays | 45.5% |
| Moderate/high activity first visit (DAS28) | 74.3% |
| Initial DAS28 (SD) | 4.7 (1.8) |
| DMARDs | 96.3% |
| DMARDb | 22.9% |
| Appropriate adherence to established therapeutical guidelines | 93% |
| Good EULAR response to the first treatment | 55.5% |
| Remission during the first year | 11% |
| Remission in a point during the follow up | 74% |
| Sustained remission in the last two visits | 52.8% |
RF: rheumatoid factor; ACPA: anti-cyclic citrullinated peptide antibody; DAS28: disease activity score in 28 joints; DMARDs: synthetic disease modifying antirheumatic drugs, DMARDb: biologic synthetic disease modifying antirheumatic drugs.
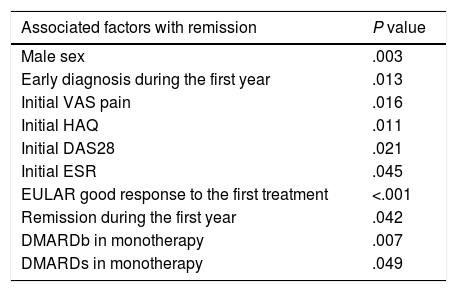
The univariate analysis showed an association between being in sustained remission and the following baseline variables: male sex, early diagnosis (during the first year of the disease), pain VAS, HAQ, DAS28 score, ESR, good EULAR response to the first treatment, remission during the first year and either DMARDb or DMARDs in monotherapy (Table 2).
Univariate Analysis.
| Associated factors with remission | P value |
|---|---|
| Male sex | .003 |
| Early diagnosis during the first year | .013 |
| Initial VAS pain | .016 |
| Initial HAQ | .011 |
| Initial DAS28 | .021 |
| Initial ESR | .045 |
| EULAR good response to the first treatment | <.001 |
| Remission during the first year | .042 |
| DMARDb in monotherapy | .007 |
| DMARDs in monotherapy | .049 |
VAS: visual analog scale; HAQ: health assessment questionnaire disability index; DAS28: disease activity score in 28 joints; ESR: erythrocyte sedimentation rate; DMARDb: biologic synthetic disease modifying antirheumatic drugs; DMARDs: synthetic disease modifying antirheumatic drugs.
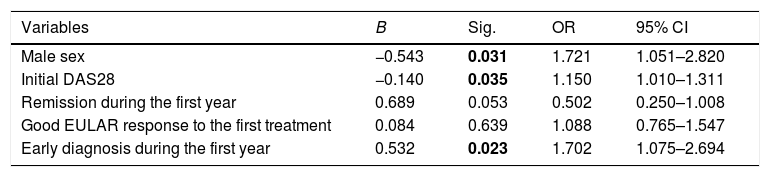
Multiple logistic regression analyses found male sex (P=.031, OR 1.7, 95% CI 1.05–2.82), diagnosis in the first year of symptoms (P=.023, OR 1.7, 95% CI 1.07–2.69) and the initial DAS28 (P=.035) to be independent predictors for sustained remission (Table 3).
Multivariate Analysis.
| Variables | B | Sig. | OR | 95% CI |
|---|---|---|---|---|
| Male sex | −0.543 | 0.031 | 1.721 | 1.051–2.820 |
| Initial DAS28 | −0.140 | 0.035 | 1.150 | 1.010–1.311 |
| Remission during the first year | 0.689 | 0.053 | 0.502 | 0.250–1.008 |
| Good EULAR response to the first treatment | 0.084 | 0.639 | 1.088 | 0.765–1.547 |
| Early diagnosis during the first year | 0.532 | 0.023 | 1.702 | 1.075–2.694 |
The values expressed in bold are the values with statistical significance.
RA is a chronic inflammatory disease that may cause joint destruction, functional disability and a reduction of the patient's quality of life. Unfortunately, there is no curative treatment for the disease, that is why the real goal is to release inflammation to achieve remission.
Cohort Characteristics75% of our patients were women and the mean age at the analysis was 58 years. Almost 80% were RF (+) and 73% ACPA (+), these are similar characteristics to other large cohorts of RA like QEST-RA2 with more than 5000 patients, 79% female and a mean age of 57 years or CORRONA7 cohort with more than 10,000 patients, 76% women with a mean age of 53 years and 78% RF (+).
Regarding disease activity, there is a big variability depending on the research consulted because of the use of different criteria to define the activity of the disease. In our study, the medium value of DAS28 at basal visit was 4.7 and the VAS pain 63 points. In the database BARFOT that included 698 patients, the average of VAS pain was 46 points and the medium value of DAS28 was 5.2.3 In our research, 84% of the patients had DMARDs treatment and 22% DMARDb therapy; comparable data with other seria of patients like the French cohort ESPOIR with 532 patients, 90% with DMARDs therapy and 23% with biological therapy4; or TARACT cohort with 335 patients, where 89% had DMARDs and 10% DMARDb.
Talking about remission, in this study the prevalence of remission using DAS28 in the first visit was 5%, 11% achieve remission during the first year of treatment and 72% had remission at some point during the follow-up. A considerable number of research about prognostic factors of remission in RA show different results due to the heterogenicity of the patients studied, the different definitions of remission and the treatments used. It has been observed prevalences of remission from less than 10% to up to 40%,2,5 although the studies that find higher percentages of remission are those that include early RA. The remission criteria in RA are in continuous discussion because, depending on the tool we use, patients with the same activity have different scores. In fact, in a study of the QUEST-RA cohort,2 where they evaluated the prevalence of remission using different criteria, they found a great variability (8.6% using ACR and 19.6% using DAS28), concluding that using different criteria results in obtaining different percentages of remission in patients with the same disease activity.
Prognostic Factors of Sustained RemissionRegarding sustained remission, the prevalence of sustained remission in our study was 46%. We did not find any relation between age and disease duration and clinical remission in RA; which has been published in other studies.6
1st suggestion → In the univariate analysis we did not find a relation between the age and the sustained remission. There were more patients achieving remission in the group of younger than 50 years old (58%) than in those patients older than 50 years old (49%) but this finding was not statistically significant. The duration of the disease was shorter in those patients that were in remission than in those who were not in remission but there were no statistically significant association. There were no statistically significant relation between sustained remission and disease duration categorized in less than 5 years, 5–10 years or more than 10 years.
Male sex was identified as an independent prognostic factor of remission in the multivariate analysis; association that has been communicated before.6 Men had approximately twice the probability of achieving remission than women. Male sex has been related to remission in previous studies like the one with CORRONA cohort with more than 10,000 patients where they used as remission criteria CDAI<2.8.7 Also, in the study with the French cohort BARFOT, male sex has been identified as independent prognostic factor of remission (OR 1.5) using DAS28 in the last two consecutives visits as sustained remission definition.3 Finally, in the GISEA study with 1257 patients treated with DMARDb, it was found male sex as predictor factor of remission.8
Early DiagnosisHalf of the patients in the Rheumatology Division HUGCDN were attended in the first six months after the onset of symptoms which had a relation with the probability of achieving remission either at any point during the follow-up or sustained remission. Early diagnosis in the first year was identified as an independent prognostic factor of maintained remission. So, this is one of the modifiable predictor factors to take into account in the management of a Rheumatology Service in order to achieve the therapeutic goals in RA. The evaluation of a specialist and the early diagnosis since the onset of symptoms will speed up the implementation of adequate treatment and will increase the patient's chances of remission. In this study, the data were variable because there were patients who were on follow up since 2000 up until 2013. Due to the improvement of derivation of patients from primary care and from other Hospital divisions, the delay has been shortened optimizing early diagnosis, although the results could be better. Early diagnosis has been related to remission in other studies such us TARACT,9 a retrospective research in which the definition of sustained remission was remission using DAS28 in two consecutive visits within three months.
RA Activity in the First VisitIn this study, it has been observed that the RA activity in the first visit will predict the prognosis of the disease. The medium DAS28 punctuation of our cohort of patients was 4.7 and more than 75% of the patients presented moderate to high RA activity at the beginning. DAS28 score was identify as an independent predictive factor of sustained remission in the multivariable analysis, and that has been observed in previous studies.6,10 Low baseline DAS28 was strongly predictive of the achievement of remission, which has been reported in other researches.3,11
A lower VAS pain score in the first visit was associated with remission during the first year of treatment, with remission in any point during the follow up and with maintained remission. Vázquez et al.11 also found a relation between low VAS pain at the beginning and sustained remission.
Functional CapacityFunctional disability will also predict the course of the disease. As seen in previous studies,6,8 the more disability at the beginning, the worse treatment response and the lower the probability of achieving remission. In our research, we found a correlation between a lower HAQ score and remission, correlation also observed in a French cohort of 191 AR patients10 and in the BARFOT cohort.3 Although, neither in our or in previous studies, HAQ score has been identified as an independent predictor factor.
Acute Phase Reactants (APR)In our study, we found an association between ESR<30 and sustained remission, that has been previously observed in other studies,11 but this association was not seen after the multivariate analysis. Regarding CRP or anemia, although patients in clinical remission had lower levels of CRP and less anemia, this data was not related to remission. Vázquez et al.11 found a relation between low levels of hemoglobin and a lower probability of remission and in a French cohort,10 they found a higher probability of remission in patients with levels of CRP<14.5mg/l. In two adalimumab studies,6,12 they found CRP<20mg/l as an independent factor of remission.
Serological MarkersSerum levels of RF and ACPA have been identified as poor prognostic factors in RA, although, being ACPA or RF negative, is not clearly related to a better outcome. In our study we did not find a relation between RF or ACPA and remission. In previous researches, RF negativity has been associated with remission3,9–11 but not as an independent factor. Regarding ACPA, only one study has found association between its negativity and remission.3
ComorbiditiesComorbidities in RA patients were not associated with remission in our study. The comorbidities profile on patients with RA is similar to the profile seen in other studies, where hypertension is the most prevalent comorbidity and the percentages of diabetes, depression and infarct are similar. We did not find a relation between Charlson comorbidity index and remission, association that has not been evaluated previously.
Toxic HabitsAlthough smoking is a poor prognostic factor in RA,13 in this study there was no relation found between tobacco and remission.
TreatmentsRegarding treatments, an adequate adherence to treatments was related to the probability of achieving remission at some point during the follow up. We also found a relation between the use of DMARDs in monotherapy and sustained remission. That is a fact that could be explained because, normally, patients with better response to treatments, have a less aggressive disease so they require less intensification of therapies. Therefore, a patient with a good response to methotrexate in monotherapy, with a good symptom follow up and low disease activity, probably will not need to add another DMARD. So, this patient profile will achieve remission in monotherapy.
2nd suggestion → The use of biologic DMARD in monotherapy was associated with persistent remission in the last year. But regarding this concept, we have to say that it was a small number of patients (15), and half of them were treated with tocilizumab, biologic agent that, as it is known, reduces in a significant way ESR levels and therefore leads to lower DAS28 scores.14 In general terms, biologic therapy was not associated with remission, probably due to a bias in prescription: patients receiving biologic DMARD are those patients that have not responded to conventional therapy with DMARDs and therefore have a more severe RA.
Another variable associated with remission in our patients was the good EULAR response to the first treatment. The good clinical response after the initial treatment has been identified as a remission predictor factor in some studies.9,12,15 In a study of the TARACT cohort with 366 patients, the good EULAR response during the first year (OR 3.1) was found as an independent predictor factor of sustained remission in the last two visits.9 In the RAPID1 study with Certolizumab pegol, with 703 patients with a disease duration of 6 years and a medium value of DAS28 of 7 (high activity), they observed that patients with a good response to treatment at weeks 4, 6 and 8, had a higher probability of achieving reduced disease activity during the first year. Achieving reduced disease activity or a decrease in the DAS28 score with the first treatment was associated with remission at some point during the follow up and with sustained remission in the last year.16 Not only the good EULAR response to the first treatment, but also achieving remission during the first year of treatment, was associated with sustained remission in our patients. This association has been observed in the ESPOIR study.4 In the study of the cohort CORRONA17 they observed that patients that were in remission during the first year, have a higher probability to continue in remission.
ConclusionWe concluded that the initial presentation and situation of the patient and the delay in the first visit to the Rheumatologist will determine the future of the disease. The RA activity at the basal visit will be the key for the achievement of the therapeutic goals. The modifiable factors consist in improving the derivation of patients from the primary care to the specialist to make an early diagnosis and initiate an intensive treatment as soon as possible.
The present research presents various strengths. The relevance of this research is that we have studied real live patients of the Rheumatology Department. Its importance lies with its observation of real clinical practise, with an important number of patients with a medium follow up of almost 10 years. All the rheumatologists in the department have a systematic way of work, either in the first visit or subsequent visits.
On the other hand, our study presents limitations. It is a retrospective study with patients with a follow up of almost 10 years, so that, not all data was available for revision and some data was collected after the fact, such as calculation of activity index scores.
Clinical remission is the goal of the treatment of RA patients. A non modifiable factor of poor prognosis is female gender; but an early diagnosis and a good EULAR response to the first treatment will improve the achievement of therapeutic goals. Moreover, a lower disease activity using DAS28 in the first visit is a predictor factor of remission in RA patients.
Ethics ApprovalEthical Committee of the University Hospital of Gran Canaria Dr Negrín.
FundingThis study has not been supported by any public nor private entity.
Conflict of InterestThe authors declare no conflict of interests.
The authors would like to thank all members of the Rheumatology Department of Hospital Universitario Gran Canaria Dr Negrín.