Rice body formation is an uncommon inflammatory process occurring in joints and tendon sheaths in systemic disorders.1 Since their first description in 1895 in a patient with tuberculosis, these have been described in various rheumatic diseases including rheumatoid arthritis, juvenile idiopathic arthritis, and seronegative inflammatory arthritis, in infections with atypical mycobacteria, and in subacromial bursitis.2–5 Generally involving shoulder and knee joints, we describe here a rare case report of a patient with isolated wrist tenosynovitis with rice bodies on magnetic resonance imaging (MRI) who was diagnosed as tuberculosis based on results of microbiologic investigations.
A 50-year-old lady came with progressive pain and isolated swelling of the right wrist of 9 months duration. Physical examination revealed an oblong swelling on the volar aspect of wrist extending into the forearm. Attempted active flexion at the wrist was painful though passive range of movement was normal. Laboratory investigations showed raised erythrocyte sedimentation rate of 50mm/h. Radiograph of the wrist was normal. MRI revealed well-defined fluid intensity collection along the flexor tendon sheath with presence of hypointense-layered lucencies within suggestive of tenosynovitis with rice bodies (Fig. 1A and B). The adjacent bone and soft tissues were normal. Fluid obtained by ultrasound-guided aspiration from the tenosynovial swelling was positive for Acid Fast Bacilli. Culture grew Mycobacterium Tuberculosis and hence, diagnosis of tuberculosis was reached. The patient did not have diabetes and was not on any immunosuppressive drugs. Serology for Human Immunodeficiency Virus (HIV) was non-reactive. The patient responded to six months of anti-tuberculous therapy with complete resolution of pain and swelling.
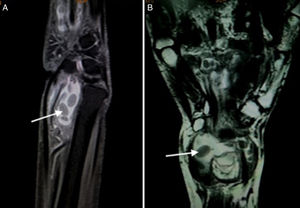
(A) T2W FAT SAT sagittal image show a well defined fluid intensity collection seen along the flexor tendon sheath with presence of hypointense layered rice grain (white arrow) shaped within it suggestive of tenosynovitis with multiple loose bodies. (B) T2W Coronal images show well defined fluid intensity collection anterior to the wrist joint along the flexor tendon sheath suggestive of tenosynovitis. Multiple layered hypointense loose bodies like rice grain are seen within it (arrow).
Rice bodies are called so due to their resemblance to grains of polished white rice on gross examination. The pathogenesis of rice body formation is unclear, but is likely related to shedding of the infarcted synovial tissue into the joint.2 These are formed by fibrin deposits on a nidus of sloughed synovium or inflamed tissue, as evidenced by rim of fibroblasts and inflammatory cells on a nidus of collagen. Types 1, 2 as well as small amounts of type 5 collagen have been demonstrated on histopathological sections.2,6,7 Rice bodies can be detected on both ultrasonography and MR imaging. Ultrasonography of tendon sheath may show low-level internal echoes or an apparent soft tissue mass, however, may fail to delineate individual rice bodies, particularly if these are too small.8 Therefore, MRI is considered the imaging modality of choice for rice bodies which appear iso- or hypointense to skeletal muscle on T1- and T2-weighted images.1
Rice bodies are known to occur commonly in rheumatic conditions such as rheumatoid arthritis (RA), juvenile idiopathic arthritis, seronegative inflammatory arthritis, and also osteoarthritis.2–4,9 Pigmented villonodular synovitis (PVNS) and synovial osteochondromatosis form the primary differential diagnoses. In a patient with isolated tenosynovitis, infection is highly likely, and mycobacteria are most often implicated. Rice body formation has been seen with tenosynovitis due to Mycobacterium tuberculosis, and nontuberculous mycobacteria (NTM), including Mycobacterium marinum, Mycobacterium kansasii, rapid growing mycobacterium, Mycobacterium avium and Mycobacterium intracellulare.5 The laboratory should always be informed of the possibility of NTM, as these can be differentiated on culture. Treatment includes mycobacterial therapy and tenosynovectomy to avoid complications such as tendon rupture.10 However, rarely, as in our case, resolution has been reported with antitubercular therapy without any surgical treatment.11
In a patient with early polyarthritis yet negative autoantibodies, rice body formation could be a salient marker to underlying RA. In established RA, it is important to know that these solid masses are treatable; as resolution has been described with intraarticular steroids and/or disease modifying anti-rheumatic drugs in most cases without sequelae. This can obviate a surgical procedure, which although initially successful, is associated with recurrence in one-third of patients. Half of those with recurrence require re-operation.12 Lastly, rice bodies are rare in the wrist. If not identified and treated they can progress to compressive neuropathy and tendon ruptures.13