Sarcoidosis is a chronic granulomatous disease that develops with non-caseified granuloma formation. Galectin-3 is a multifunctional protein operating in biological processes such as fibrosis, angiogenesis, and immune activation.
PurposeThis study evaluates the levels of serum galectin-3 and TGF-beta in sarcoidosis patients to determine a possible correlation with clinical findings.
Material and methodForty-four biopsy-proven sarcoidosis patients followed in a single centre and 41 age and sex-matched healthy volunteers were included in the study. The levels of serum galectin-3 and TGF-beta were evaluated by ELISA method.
ResultsAmong the 44 sarcoidosis patients, 13(29.5%) were male and 31(70.5%) were female. The average patient age was 47.4 and the average disease duration was 3.2 years. The level of serum galectin-3 was found to be the same as in the control group and had no significance statistically (p=.977). No correlation was determined between the level of serum galectin-3 and clinical and laboratory findings of sarcoidosis (p>.05). The level of serum TGF-beta was found to be higher in the sarcoidosis patients when compared to that of the control group (p=.005). While a correlation was found between serum TGF-beta and enthesitis, sacroiliitis, and arthralgia (p=.006, p=.034, p=.02), no correlation was determined on the other clinical and laboratory findings (p>.05).
ConclusionWhile the level of serum galectin-3 was determined to be normal in sarcoidosis patients, a high level of serum TGF-beta was found. These findings show that TGF-beta may play an important role in sarcoidosis pathogenesis and the formation of granuloma.
La sarcoidosis es una enfermedad granulomatosa crónica que se desarrolla con una formación de granuloma no caseificado. Galectina-3 es una proteína multifuncional que opera en procesos biológicos como la fibrosis, la angiogénesis y la activación inmune.
PropósitoEste estudio evalúa los niveles séricos de galectina-3 y TGF-beta en pacientes con sarcoidosis para determinar una posible correlación con los hallazgos clínicos.
Material y métodoFueron seguidos en un solo centro 44 pacientes con sarcoidosis probados por biopsia y se incluyeron en el estudio 41 voluntarios sanos de la misma edad y sexo. Los niveles séricos de galectina-3 y TGF-beta fueron evaluados por el método ELISA.
ResultadosEntre los 44 pacientes con sarcoidosis, 13 (29,5%) eran hombres y 31 (70,5%) eran mujeres. La edad promedio de los pacientes fue de 47,4 y la duración promedio de la enfermedad fue de 3,2 años. Se encontró que el nivel de galectina-3 en suero era el mismo que en el grupo control y no tenía significancia estadística (p = 0,977). No se determinó correlación entre el nivel sérico de galectina-3 y los hallazgos clínicos y de laboratorio de sarcoidosis (p > 0,05). El nivel de TGF-beta en suero se encontró más alto en los pacientes con sarcoidosis, en comparación con el del grupo control (p = 0,005). Si bien se encontró una correlación entre el TGF-beta sérico y la entesitis, sacroileítis y artralgia (p = 0,006, p = 0,034, p = 0,02), no se determinó correlación en los otros hallazgos clínicos y de laboratorio (p > 0,05).
ConclusiónSi bien se determinó que el nivel sérico de galectina-3 era normal en pacientes con sarcoidosis, se encontró un alto nivel de TGF-beta en suero. Estos hallazgos muestran que el TGF-beta puede desempeñar un papel importante en la patogénesis de la sarcoidosis y la formación de granuloma.
Sarcoidosis is a systemic disease of unknown causation that affects many different types of tissue and organs characterized by non-caseified granuloma reactions.1 The disease is presented most frequently with hilar lymphadenopathy, lung infiltration, and skin and eye lesions. Although its pathogenesis has not been clarified exactly, cellular immune system activation and non-specific inflammatory response occur with the effects of some genetic and environmental factors.2 Th1-cells and macrophage-based pro-inflammatory cytokines trigger the inflammatory cascade and granuloma formation is developed as a result of tissue permeability, cell influx, and local cell proliferation.3 Non-caseified epithelioid cell granulomas are the pathological findings of sarcoidosis.4 Some biological reagents used in the diagnosis and monitoring of sarcoidosis (serum ACE, serum calcium, and D3) are not specific to the disease and they also are determined in various pathologies. Therefore, the existence of some molecules specific to sarcoidosis is being sought. Galectin (Gal) is a lectin based on beta-galactoside that occurred in the carboxyl-terminal and amino-terminal domains.5 Recently, 15 members of the Gal family have been defined. This family can be divided into three main groups as per the structure of galectin. Only Gal-3 has a chimeric structure and is defined in many types of tissue and cells including monocyte, macrophage, dendritic, mast, eosinophils, and B and T lymphocytes. Gal-3 has various effects on biological and pathological processes such as inflammatory, autoimmune, fibrosis, cell adhesion, proliferation, differentiation, and tumor invasion.6,7 Gal-3 plays a significant role in the development of inflammation with the interaction of various cytokines and chemokines. It is a pleiotropic cytokine with biological and regulatory effects on TGF-β cells8 and plays a critical role in cellular growth, development, differentiation, and proliferation. Furthermore, it takes part in many events such as extracellular matrix synthesis and lysis, control of mesenchymal-epithelial interactions during embryogenesis, immune modulation, apoptosis, angiogenesis, adhesion and migration, and leucocyte chemotaxis.9 Gal-3 and TGF-beta have been studied as inflammatory mediators in chronic diseases such as systemic sclerosis (SSc), RA, and SLE. The expression of serum Gal-3 increases has been observed in many rheumatic diseases and a correlation with some clinical findings established.10–12 It has been considered that Gal-3 might have a role in erosive and destructive arthritis in RA patients. While it is believed that TGF-beta is responsible for tissue repair or pathological fibrosis in the late stage of sarcoid inflammation, it also can play an important immunomodulatory role in the early stage of sarcoid inflammation.13 As the roles of Gal-3 and TGF-beta in sarcoidosis pathogenesis have not yet been clarified, it is hard to utilize them as disease markers.
This study aims to determine the serum Gal-3 and TGF-beta levels of patients with sarcoidosis and to reveal their possible relationship with disease features.
Materials and methodForty-four patients diagnosed with sarcoidosis as a result of the conducted tests were consecutively taken into the study. Forty-one healthy volunteers compatible in age and gender were included in the study as the control group. The sarcoidosis diagnosis was made with biopsy and histopathological examinations taken from different organs and tissues, and the demonstration of the non-caseified granuloma. Other reasons likely to cause granulomatous illnesses (bacterial, fungal infections) were eliminated. The following laboratory tests were conducted on all patients with sarcoidosis: routine biochemistry, acute phase reactants (ESR, CRP), serum ACE, calcium and D3 levels were all checked. Lung X-ray and thorax CT imaging were conducted for staging the sarcoidosis. All events were questioned in detail and their systemic and rheumatologic examinations performed. Informed consent was taken from each of the individuals in the patient and control groups and entry forms were filled out. All of the demographic, clinical, serologic and radiological data of the patient group individuals were registered. Blood samples from patients and healthy volunteers taken in tubes and procured by centrifuge for 10min at 4000rpm were preserved in a refrigerator at −80°C until the study. During the study, the serums were transferred into the +4°C part of the refrigerator a day before and kept there to defrost. Before pipetting, the homogeneity of the serums was ensured by vortexing. The eBioscience brand (Vienna, Austria) micro ELISA kit (catalog number: BMS279/2 BMS279/2 TEN) was used for the quantitative analysis of the serum Gal-3 level. The study purpose ELISA kit (Catalog number: BMS249/4 BMS249/4 TEN) of the same brand was used for the Serum TGF-β1 designation. A BioTek ELX 50 washer was used during the washing process performed according to the kit prospectus, and BioTek ELX 800 for the microplate absorbance readings.
Statistical methodR Studio V.0.98.501 was used in the analysis of the obtained data. The normality of the distribution of the variables was researched through visual analyses such as histogram, probability plot, and analytical methods (Kolmogorov–Simirnov/Shapiro–Wilk test). Definitive analyses were submitted using the average and standard deviation for the normally distributed variables. The comparison between the independent groups (control vs. patients) was made by independent t-test. The comparison of whether there was any connection between the clinical findings (erythema nodosum, uveitis, etc.) and the analyzed parameters within the patient group was made using the Mann–Whitney U test with p<0.05 values accepted as statistically significant.
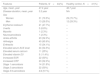
ResultsThirteen (29.5%) of the patients with sarcoidosis were men and 31 (70.5%) were women. The average age of patients was 47.4 years with an average illness duration of 3.2 years. When the system and organ involvement were assessed, erythema nodosum in 21 (47.7%), uveitis in 3 (6.8%), arthralgia in 40 (90.9%), ankle arthritis in 23 (52.3%) and enthesitis in 15 (34.1%) of the patients were seen. No patients with cardiac involvement were detected. As a result of the thorax CT, 14 (31.8%) of the patients were seen to have stage 1, 22 (50%) patients stage 2, four (9.1%) patients stage 3, and four (9.1%) patients stage 4 sarcoidosis. The histopathological verification of the sarcoidosis was done with skin and axillary LAP biopsy and demonstration of the non-caseified granuloma. The laboratory evaluation showed high serum levels of ACE in 24 patients (54.5%), calcium in 11 patients (25%), D3 in 5 patients (11,4%), ESR in 22 patients (50%), and CRP in 23 patients (52.3%) (Table 1). Serum Gal-3 levels were found to be similar in both the sarcoidosis patients and the control group (p=0.977) (Table 2). No correlation was detected between the serum Gal-3 levels and some clinical and laboratory findings (p>0.05). The serum TGF-beta levels were higher in patients with sarcoidosis when compared to the control group (p=0.005). While a connection between the serum TGF-beta and enthesitis sacroiliitis, and arthralgia was present (p=0.006, p=0.034, p=0.02 respectively), other clinical and laboratory findings showed no correlation (Table 3).
Demographic, clinical and laboratory features of patients with sarcoidosis and healthy control group.
| Features | Patients, N=44(%) | Healthy control, N=41(%) |
|---|---|---|
| Age, mean, year | 47.4 year | 46.7 year |
| Disease duration, mean, year | 3.2 year | NA |
| Sex | ||
| Women | 31 (70.5%) | 29 (70.7%) |
| Men | 13 (29.5%) | 12 (29.3%) |
| Erythema nodosum | 21 (47.7%) | – |
| Uveitis | 3 (6.8%) | – |
| Myositis | 1 (2.3%) | – |
| Neurosarcoidosis | 1 (2.3%) | – |
| Ankle arthritis | 23 (52.3%) | – |
| Arthralgia | 40 (90.9%) | – |
| Enthesitis | 15 (34.1%) | – |
| Elevated serum ACE level | 24 (54.5%) | – |
| Elevated serum calcium | 11 (25%) | – |
| Elevated vitamin D3 | 5 (11.4%) | – |
| Increased ESR | 22 (50%) | – |
| Increased CRP | 23 (52.3%) | – |
| Stage 1 sarcoidosis | 14 (31.8%) | – |
| Stage 2 sarcoidosis | 22 (50%) | – |
| Stage 3/4 sarcoidosis | 4/4 (9.1%) | – |
Abbreviations: ACE: angiotensin converting enzyme; ESR: erythrocyte sedimentation rate; CRP: C-reactive protein.
Correlation between serum Gal-3 and TGF-beta with clinical findings in patients with sarcoidosis.
| Findings | Galectin-3p-Value | TGF-B1p-Value |
|---|---|---|
| E. nodosum | 0.081 | 0.102 |
| Uveitis | 0.072 | 0.065 |
| Arthralgia | 0.081 | 0.02 |
| Ankle arthritis | 0.652 | 0.415 |
| Sacroiliitis | 0.513 | 0.034 |
| Enthesitis | 0.404 | 0.006 |
| Elevated serum D3 | 0.542 | 0.076 |
| Elevated CRP | 0.161 | 0.873 |
| Elevated ESR | 0.602 | 0.713 |
| Elevated serum ACE | 0.193 | 0.652 |
* p<0.05 statistically significant.
In this study, we found higher TGF-beta levels in sarcoidosis patients, while those of Gal-3 were similar to those of the healthy controls. While no association between the clinical findings of sarcoidosis and Gal-3 was found, a statistically significant connection was detected between the TGF-beta, enthesitis, and arthralgia. While some previous studies have shown that serum Gal-3 level is higher in some rheumatic diseases with inflammatory arthritis (scleroderma, rheumatoid arthritis, Behçet's disease, SLE), this is the first study on the relationship between sarcoidosis and Gal-3 in the literature. Koca et al. established that when compared to the control group, patients with scleroderma and SLE have high levels of Gal-3, and postulated that this might be associated with disease activity.14 In another study, a high level of serum Gal-3 was detected in patients with Behçet's disease and was found to be associated with disease activity.15 Ezatt et al. reported a correlation between serum Gal-3 levels and the activation and progression of the disease.16 Forsman et al. detected a correlation between serum Gal-3 and the erosive and destructive course of arthritis in the antigens-induced arthritis model.17 Filer et al. on the other hand, showed that serum Gal-3 triggers different cytokine profile and signal transduction pathways in the RA joint synovium. The overexpression of the Gal-3 in the synovium was shown to trigger the release of pro-inflammatory cytokines synthesized from the tissue fibroblasts over the MAPK signal transduction pathways and PI-3.7 Ohshima et al. have shown the overexpression of Gal-3 in patients with RA and that it could be an important biomarker of the activation of the disease.18 In their study, Guevremont et al. showed that Gal-3 is expressed on the chondrocytes and is a possible substrate for some destructive enzymes such as the collagenase-3.19 These studies revealed a relationship between Gal-3 and erosive and destructive arthritis. It also is known that the levels of Gal-3 and TNF-alfa have significant correlation and subsequent to treatment of anti-TNF-alfa, the serum and synovial Gal-3 levels return to normal.20 Clearly, the synergistic effects of these two molecules contribute to destructive changes in the joints. Non-destructive arthritis seen in sarcoidosis, contrary to the above, may be explained with low Gal-3 levels, as shown in our study. The mild form of arthritis and low levels of advanced disease in sarcoidosis may be explained by low levels of Gal-3. To confirm this hypothesis, molecular studies that show Gal-3 expression in not only the serum but also the synovial fluid and tissue are required. Our study is the first regarding this subject. The role of TGF-beta in the formation of granuloma seen in sarcoidosis is well known. However, the role of this molecule in the sarcoid arthritis model is not yet certain. Our study reveals a correlation between clinical disease findings as well as the TGF-beta level in patients with sarcoidosis. This points to the important role of the molecule in the sarcoidosis pathogenesis.
The study has its limitations. First, the low number of patients prevents us from generalizing based on these results. Second, we considered only the serum Gal-3 level. To illuminate the pathogenesis of sarcoid arthritis, it is necessary to check the Gal-3 expression in the synovial fluid and tissue as well. Again, another primary rheumatic disease (like RA) could have been used as the control group.
In conclusion, we detected low levels of serum Gal-3, while serum TGF-beta was higher in patients with sarcoidosis. While there was a detected association between TGF-beta and some clinical features of the disease, there was no correlation found between serum Gal-3 and the clinical disease finding. Further studies are required to illuminate the pathogenesis of sarcoidosis and reveal new biomarkers to be used in the diagnosis and activation of the disease.
Conflict of interestThe authors declared no conflict of interest.