Nailfold capillaroscopy has been used as a non-invasive diagnostic method for microvasculature evaluation in various rheumatological disorders. The present study aimed to determine the utility of nailfold capillaroscopy in the diagnosis of Kawasaki Disease (KD).
MethodIn this case–control study nailfold capillaroscopy was performed in 31 patients with KD and 30 healthy controls. All nailfold images were evaluated for capillary distribution and capillary morphology such as enlargement, tortuosity, and dilatation of the capillaries.
ResultAbnormal capillaroscopic diameter was identified in 21 patients from the KD group and 4 patients in the control group. The most common abnormality in capillary diameter was irregular dilatation in 11 (35.4%) KD patients and in 4 people (13.3%) in the control group. Distortions of the normal capillary architecture was commonly seen in the KD group (n=8). A positive correlation was observed between coronary involvement and abnormal capillaroscopic results (r=.65, P<.03). The sensitivity and specificity of capillaroscopy for the diagnosis of KD were 84.0% (95%CI: 63.9–95.5%) and 72.2% (95%CI: 54.8–85.8%), respectively. The PPV and NPV of capillaroscopy for KD were 67.7% (95%CI: 48.6–83.3) and 86.7% (95% CI: 69.3–96.2), respectively.
ConclusionCapillary alterations are more common in KD patients compared to control group. Thus, nailfold capillaroscopy can be useful in detecting these alterations. Capillaroscopy is a sensitive test for detecting capillary alternations in KD patients. It could be used as a feasible diagnostic modality for evaluating microvascular damage in KD.
La capilaroscopia periungueal se ha utilizado como un método diagnóstico no-invasivo para evaluación de la microvasculatura en varios trastornos reumatológicos. El presente estudio pretendió determinar la utilidad de la capilaroscopia periungueal en el diagnóstico de la enfermedad de Kawasaki (KD).
MétodoEn este estudio de casos y controles se realizó la capilaroscopia periungueal para 31 pacientes con KD y 30 controles sanos. Todas las imágenes de la ungueal se evaluaron para la distribución capilar y la morfología capilar, como la ampliación, la tortuosidad y la dilatación de los capilares.
ResultadoSe identificó un diámetro capilaroscópico anormal en 21 pacientes del grupo KD y en 4 pacientes del grupo control. La anomalía más común en el diámetro de los capilares fue la dilatación irregular en 11 (35,4%) pacientes con KD y 4 personas (13,3%) en el grupo control. Las distorsiones de la arquitectura capilar normal se observaron comúnmente en el grupo KD (n=8). Se observó una correlación positiva entre la afectación coronaria y los resultados capilares anormales (r=0,65, p <0,03). La sensibilidad y la especificidad de una capilaroscopia para el diagnóstico de KD fueron del 84,0% (IC del 95%: 63,9-95,5%) y del 72,2% (IC del 95%: 54,8-85,8%), respectivamente. El VPP y el VAN de la capilaroscopia para KD fueron del 67,7% (IC del 95%: 48,6-83,3) y del 86,7% (IC del 95%: 69,3-96,2), respectivamente.
ConclusiónLas alteraciones capilares son más frecuentes en los pacientes con KD en comparación con el grupo control. Así, la capilaroscopia periungueal puede ser útil en la detección de estas alteraciones. La capilaroscopia es una prueba sensible para detectar las alteraciones capilares en pacientes con KD. Podría utilizarse como modalidad diagnóstica factible para evaluación el daño microvascular en la KD.
Kawasaki disease (KD) is an acute inflammatory process mainly affecting children and characterized by multi-system vascular involvement.1 These patients experience a broad spectrum of clinical manifestations, including skin lesions, eyes, and neurological systems.2 Besides, numerous studies have shown that KD patients suffer from cardiovascular complications as the major causes of morbidity and mortality among these groups of patients.3,4 The major concerns lie in determining coronary artery abnormalities. However, other vascular abnormalities involved in systemic vascular physiology are gaining great clinical interest, including increased carotid artery intima-media thickness, reduced distensibility of arteries, and increased stiffness of central and peripheral arteries.5,6 Histopathological studies demonstrated the presence of aneurysm sites at other locations, predominantly affecting small to medium-sized vascular territories such as brachial, renal, femoral, and iliac arteries.7 The arterial function was investigated in several studies by various methods, including evaluation of coronary flow reserve with angiography, intracoronary flow velocity by transthoracic echocardiography, magnetic resonance imaging, and positron emission tomography.8,9
Nailfold capillaroscopy was a non-invasive diagnostic method for microvasculature evaluation in various rheumatologic disorders.10,11 Distinct morphologic patterns on nailfold capillary changes reveal specific capillaroscopic patterns, possibly reflecting an underlying autoimmune inflammatory disease. This technique is helpful for microvascular analysis in several diseases such as Juvenile systemic sclerosis, systemic lupus erythematosus, Sjogren's syndrome, Behçet's disease, and familial Mediterranean fever.11,12 Although capillaroscopy is considered a safe and feasible diagnostic tool, little information exists regarding the application of this technique to assess microvascular function among the pediatric population diagnosed with KD. Therefore, the present study aimed to determine the utility of nailfold capillaroscopy in KD patients.
Materials and methodsPatient populationIn this case–control study, all consecutive KD patients diagnosed with KD at the Pediatric Rheumatology Department (Pediatrics Center of Excellence affiliated to Tehran University of Medical Sciences, Tehran, Iran) were included from September 2017 to November 2018. According to American Heart Association guideline, 31 patients were identified with KD. After diagnosing KD, all patients received 2g/kg of IVIG as a single dose and a high dose of aspirin (80–100mg). Patients were excluded if they had a previous history of coronary artery abnormality, hypertension, diabetes mellitus, pre-existed cardiovascular disease, taking vasoactive drugs, and caffeinated beverages.
The control group was selected from children under six who were referred to a growth and development clinic for routine examination and had normal growth and development without any background disorder.
The ethics committee of Tehran University of Medical Sciences approved this study. All parents were asked to fill out an informed consent before all procedures. The study was conducted under the Declaration of Helsinki and other applicable laws and regulations.
Study protocolA careful history and physical examination were performed for all subjects. All patients underwent an electrocardiogram and an echocardiogram. Medical records of KD patients were retrieved and assessed for details of their acute illness. The Nailfold capillary changes were analyzed by the digital nailfold videocapillaroscopy (NVC) (optipix-optilia OP 120 021, Sweden) and OptiPix capillaroscopy software equipped with a ×200 fiber optic illumination in the sub-acute phases of Kawasaki disease after IVIG treatment. The physician performing the procedure was unaware of the clinical information about the examinees. Capillaroscopy was performed on eight fingers with an optical microscope (at 10- and 16-time magnifications) by the same observer. Patients were asked to rest at a standard temperature of approximately 24°C for at least 15min before the procedure. According to modified Maricq's criteria, capillary distribution and capillary morphology were evaluated by NVC.13 The increased diameter is divided into two subgroups: regular dilation consists of the complete capillary dilation, whereas a segment dilation of the capillary is involved in irregular dilation.
Moreover, the definition of architectural capillary abnormality consisted of any disarray in the regular arrangement of capillaries. The capillary density was compared with the control group according to age. Morphology variations define as tortuosity, branching, and the other exclusive alternations of capillary loops.
Results were considered abnormal if there was a sign of local or global loss of capillaries (>20%), presence of hemorrhages in two or more areas (at least two fingers), or two or more dilated loops in at least two fingers. The evaluation process was repeated one month after baseline data to assess the reproducibility of the findings.
Statistical analysisNormality of the distributions of the continuous variables was examined with the Kolmogorov–Smirnov test. Continuous variables are expressed as mean±standard deviation if normally distributed. Categorical variables are reported as percentages and analyzed using the chi-squared test. The correlations between the variables were used by Pearson and Spearman test, as indicated. The sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of nailfold capiloroscopy for the corresponding KD were calculated. Two-tailed P values<0.05 were used for significance testing. All data were analyzed using Stata 12.0 (StataCorp, College Station, TX, USA).
ResultsThirty-one KD patients were identified, including 21 males (67.7%) and nine females (32.3%). The mean age of the patients and control group were not significantly different (3.39±1.59 vs. 4.58±2.91, respectively) (P=0.09). The male to female ratio was 2.1–1 in KD group. Most KD patients (71%) presented with typical clinical features of Kawasaki. Coronary involvement was identified in 13 KD patients (41.9%). The frequency of different coronary artery abnormalities as evaluated by a transthoracic echocardiogram is summarized in Table 1.
The frequency of various coronary artery involvement among KD patients.
| Coronary artery involvement features | N (%) |
|---|---|
| Patients without involvement | 18 (58.1%) |
| Coronary artery ectasia | 1 (3.2%) |
| Abnormal tapering LAD | 1 (3.2%) |
| Abnormal tapering LCA | 1 (3.2%) |
| LAD and LMCA ectasia | 2 (6.4%) |
| LCA aneurysm and abnormal tapering RCA | 1 (3.2%) |
| LCA ectasia | 2 (6.4%) |
| Mild LAD ectasia | 3 (9.7%) |
| RCA ectasia | 1 (3.2%) |
| Small aneurysmal dilation in LMCA | 1 (3.2%) |
| Total | 31 (100%) |
Abbreviation: LAD, left anterior descending; LCA, left coronary artery; LMCA, left main coronary artery; RCA, right coronary artery.
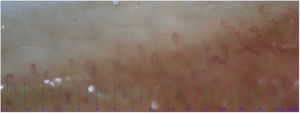
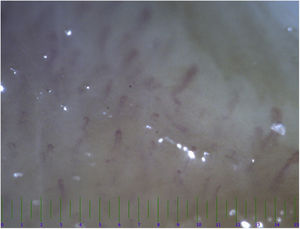
The nailfold capillaroscopy was conducted on both the KD and control groups. The abnormal capillaroscopic diameter was identified in 21 patients from KD group and four patients in the control group (Table 2). The most common abnormality in the evaluation of capillaries diameter was irregular dilatation (Fig. 1) seen in 11 (35.4%) KD patients and 4 (13.3%) in the control group. The normal capillary architecture distortions were commonly seen in KD group (n=8). On the other hand, there were no findings of architectural capillary abnormality in the control group (P=0.003). About half of KD patients had a reduction in capillary density (Fig. 2), while no similar abnormality was observed in the control group (P<0.001). There was no significant difference between KD patients and the control group in terms of morphology variations (P=0.4). Moreover, a positive correlation was observed between coronary involvement and abnormal capillaroscopic results (r=0.65, P<0.03).
The comparison of nailfold capillaroscopy findings between patients with Kawasaki disease (KD) and controls.
| Capillaroscopic features | KD(n=31) | Control(n=30) | P-value |
|---|---|---|---|
| Diameter | 0.015 | ||
| Normal | 10 (32.2) | 26 (86.7) | |
| Narrowing | 8 (25.8) | 0 (0) | |
| Regular dilatation | 1 (3.2) | 0 (0) | |
| Irregular dilatation | 11 (35.4) | 4 (13.3) | |
| Increased end of the microvascular bed | 1 (3.2) | 0 (0) | |
| Capillary architecture | 0.003 | ||
| Regular | 23 (74.2) | 30 (100) | |
| Irregular | 8 (25.8) | 0 (0) | |
| Capillary density | <0.001 | ||
| Normal | 17 (54.8) | 30 (100) | |
| Decreased | 14 (45.2) | 0 (0) | |
| Morphology | 0.41 | ||
| Loop | 26 (83.9) | 28 (93.3) | |
| Dilatation | 1 (3.2) | 0 (0) | |
| Ramified, tortuous capillaries | 4 (12.9) | 2 (6.7) | |
The sensitivity, specificity, PPV, and NPV of abnormal capillaroscopy patterns for KD were calculated. The results indicate that the sensitivity and specificity of a capillaroscopy for diagnosis of KD were 84.0% (95%CI: 63.9–95.5%) and 72.2% (95%CI: 54.8–85.8%), respectively. The PPV and NPV of capillaroscopy for KD were 67.7% (95%CI: 48.6–83.3) and 86.7% (95%CI: 69.3–96.2), respectively. The positive and negative likelihood ratios were 3.02 (95%CI: 1.74–5.26) and 0.22 (95%CI: 0.09–0.56), respectively.
DiscussionMicrocirculation is highly important to normal physiological processes, including tissue oxygenation, hemostasis, tissue repair, and nutritional exchange. Microcirculation assessment is vital in analyzing microvascular abnormalities in many rheumatologic disorders. Recently, nailfold capillaroscopy has been widely used to identify microcirculation damage since it gives precise information about capillaries’ conditions.11,14–16 However, limited data exist regarding the utility of this technique among pediatric patients with KD. The evaluations were done after IVIG treatment because Kawasaki disease is the acute vasculitis with the hypothesis of unstable alternations in the vasculature, especially the microvascular in the acute phase. The stabilization of capillaroscopy changes might be more in the sub-acute phase after IVIG treatment. In the present study, our findings suggest that nailfold capillaroscopy could detect morphological alterations in the microcirculation compared with the control group.
Our findings indicated that various morphological changes could be identified by using capillaroscopy among patients with KD, including irregular dilatation of capillaries, reduction in capillary density, and architectural capillary abnormality. Among our KD patients, the most frequent capillaroscopic findings were decreased capillary density (45.2%) and irregular dilatation of capillaries (35.4%). In patients with systemic sclerosis, the capillaroscopic patterns are characterized by a progressive capillary loss microvasculature function and have been associated with higher disease activity.17 Ingegnoli et al.18 evaluated microvascular damage among 123 cases diagnosed with systemic lupus erythematosus using nailfold capillaroscopy, and their findings indicated that about 35.8% of cases were found to have capillary abnormalities (including elongated loops, dilatation of the efferent side, increased tortuosity, and branching), while, 28.5% of the patients had shown normal pattern. The bed nails’ capillary abnormalities (including elongated loops, dilatation of the efferent side, increased tortuosity, branching, and loss of density) are determined in connective tissue disorders such as systemic lupus erythematosus,18,19 Dermatomyositis,20 scleroderma,17 and the others cause of vasculitis and vasculopathy as a chronic process of vascular inflammation.
On the contrary, Kawasaki disease is an acute vasculitis accompanied by an acute inflammation process with similar abnormalities, regardless of probable different mechanisms. Oxidative stress has a major role in endothelial dysfunction in Kawasaki disease's acute and sub-acute phases. In addition, the CRP level, fever duration, and cytokines of inflammations lead to endothelial injuries accompanied by oxidative stress directly or indirectly.21,22 So, the mechanisms of acute alternations in bed nail capillaries may differ from the chronic capillaroscopy in the other connective tissue disorders. Although, further evaluations should be involved.
This study observed a significant positive correlation between abnormal capillary changes and coronary artery involvement in sub-acute phases of Kawasaki disease after IVIG treatments. Similarly, Huang et al.23 reported that coronary artery involvement significantly correlates with changes in peripheral microcirculation, especially in the sub-acute phase. In IVIG-resistance Kawasaki disease, the IL6 and IL10 cytokines mildly decrease, and IL4 and TNFα cytokines increase with more coronary involvement.24 On the other hand, cytokine elevations and more inflammations accompanied by more oxidative stress lead to endothelial dysfunctions.25 Indeed, oxidative stress lead to RBC hemostasis dysfunctions, platelet activation, apoptosis inhibition, and ultimately thrombocytosis causes clot formations in microvascular.26 Microvascular involvements in KD such as conjunctival injections, extremities edema, and erythema in the acute phase of KD may be prodromal to medium-sized vascular involvement such as coronary vasculitis in the sub-acute phase.27 Similarly, the microvascular involvements prodromal to coronary involvements may occur in the heart muscle.28 Thus, early evaluations of microvascular involvements may change the treatment strategies to aggressive treatment in the early phase other than IVIG, such as corticosteroids and anti-TNF.29,30 Capillaroscopy may predict the early microvascular involvements, consequently improving the outcome with aggressive and urgent treatments. However, further research should be involved.
The present study had several limitations. Our study's relatively small sample size may have reduced the power to detect a significant correlation between capillaroscopic findings and other disease manifestations. Moreover, this study lacks a prospective follow-up to determine factors associated with alteration in capillaroscopic features. Therefore, the results of the present study should be interpreted in the context of its limitations.
In conclusion, the findings of this study indicate that capillary alterations can be seen in KD, although it is not specific to this disease. So, nail fold capillaroscopy can be helpful in detecting the capillary alternations in KD patients. Accurate coronary artery involvement diagnosis in KD patients is the most important component in evaluating and managing this disorder. Currently, echocardiography is the initial step in evaluating coronary complications in KD. Nailfold capillaroscopy is a feasible noninvasive diagnostic method to evaluate peripheral endothelial dysfunction that could indirectly help predict coronary arterial anomalies in KD patients, along with echocardiography. Nevertheless, Capillaroscopy cannot replace echocardiography, but it might be a complementary part of the diagnostic approach. Further studies are warranted to validate this finding and provide enough evidence on using capillaroscopy to detect coronary involvement among KD patients.
Authors’ contributionsB.S. and N.R. performed data gathering and drafting of the manuscript.
S.R., and F.T. contributed to the conception and design of the study, and clinical expertise.
R.A., and S.N. analyzed and interpreted the clinical data, and clinical expertise.
E.A. performed echocardiography and contributed to interpretation of the clinical data.
V.Z. provided the concept the survey, interpretation of the clinical data, oversaw the project and critical revision of the final draft of manuscript, primary responsibility for the paper.
All authors read and approved the final version of the manuscript.
Conflicts of interestThe authors have no conflicts of interest to declare.
This study was part of a fellowship thesis (of Dr. B. Sedaghat) supported and approved by Tehran University of Medical Sciences. We thank all the healthy participants as control group for helping us in doing this study. We would like to thank patients and their parents for giving permission to publish their data.