A Caucasian 72-year-old man with chronic obstructive pulmonary disease and paraparesis caused by thoracic spinal cord injury due to traffic accident twenty-five years ago. He presented to the emergency room with one week of cough with purulent sputum, dyspnea with 88 percent of blood oxygen saturation, intermittent fever up to 38°C and worsening of bilateral lower limbs weakness.
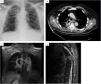
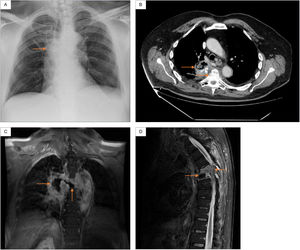
Physical examination was notable for crackles on auscultation in the upper and middle fields of the right lung, as well as spastic paraparesis with normal rectal tone. Blood test showed increased C-reactive protein 15mg/dL (reference range 0.5–1). Chest X-ray showed right paratracheal infiltrates (Fig. 1A). Chest CT showed cavitating right lung consolidation and crush located at T5-T6 (Fig. 1B). Thoracic spine MRI showed lung-spinal fistula and signs suggestive of spondylodiscitis (Fig. 1C and D).
(A) Chest X-ray: right paratracheal infiltrates. (B) Chest CT: right lung consolidation occupying the azygo-esophageal recess, with aire-fluid level and calcium deposits, as well as a marked crush and destructuring located at the T5-T6. (C) Thoracic spine MRI (coronal): central necrotic-cystic zone occupyping the disc space of the T5-T6 and fistulous communication with the adjacent right lung injury. (D) Thoracic spine MRI (sagittal): diffuse gadolinium enhancement and kyphotic deformity with canal stenosis located at the T5-T6.
An empirical antibiotic treatment was initiated with intravenous piperacillin–tazobactam for a presumed bacterial thoracic spondylodiscitis related to contiguous right-side cavitating pneumonia.1,2 Microbiological investigations were all negative.
To pursue definitive diagnosis, the patient underwent evaluation for percutaneous CT-guided spinal needle biopsy.3 However, he died on the seventh-day hospital stay due to massive hemoptysis and irrecoverable cardiac arrest. The family of the patient refused autopsy.
Conflict of interestsThe authors declare they have no conflict of interest.