Nailfold capillaroscopy (NC) is useful in the evaluation of Raynaud's phenomenon, associated with some connective tissue diseases and in the follow-up of patients with systemic sclerosis. Our study evaluates the impact of NC in the diagnosis, according to the reason for the request and profile of autoantibodies in daily clinical practice.
Material and methodsAll patients that undergone at least one NC between June 2012 and December 2017 were included. Clinical records were reviewed and analysed in a dichotomous way (yes/no), to see whether the NC contributed to a change of diagnosis in subsequent consultations. In addition, demographic, clinical and laboratory data were collected, and the relationship with NC patterns evaluated.
ResultsOf the 530 patients who had undergone at least one NC, 266 had Raynaud's phenomenon as primary indication for the technique. Of those, 20 patients (3.8%) had a diagnostic change in the post-NC consultation; 15 were diagnosed with systemic sclerosis, 4 with undifferentiated connective tissue disease and one with mixed connective tissue disease. All patients had, except for one patient diagnosed with undifferentiated connective tissue disease, positive antinuclear antibodies titres, 11 of them had disease specific antibodies (9 anti-centromere, one anti-Scl70 and other anti-RNPC). The positivity of antinuclear antibodies titres was associated with a higher probability of presenting a scleroderma pattern in the NC, and all patients with a specific rheumatological diagnosis had an abnormal NC.
ConclusionNC is a useful technique, but with limited impact in the diagnosis of connective tissue diseases. Autoantibody positivity is associated with a greater likelihood of presenting pathological NC patterns.
La capilaroscopia periungueal (CP) es útil en la evaluación del fenómeno de Raynaud tanto primario como secundario, y en el seguimiento de los pacientes con esclerosis sistémica. Nuestro estudio evalúa el impacto de la CP en el diagnóstico, en función del motivo de solicitud y el perfil de autoanticuerpos en la práctica clínica diaria.
Material y métodosSe incluyeron todos los pacientes con al menos una CP entre junio de 2012 y diciembre de 2017. Se revisaron las historias clínicas y se determinó de forma dicotómica (sí/no) si la CP contribuyó al diagnóstico realizado en la consulta posterior a la realización de la CP. Se recogieron datos demográficos, clínicos y de laboratorio, motivo de solicitud de la CP y su relación con los patrones CP.
ResultadosDe 530 pacientes con una primera CP, 266 se realizaron como estudio de un fenómeno de Raynaud. De estos, en 20 pacientes (3,8%) se realizó un diagnóstico de enfermedad del tejido conectivo en la consulta posterior a la CP; 15 fueron diagnosticados de esclerosis sistémica, 4 de conectivopatía indiferenciada y uno de enfermedad mixta. Salvo un paciente diagnosticado de conectivopatía indiferenciada, el resto tenía anticuerpos antinucleares positivos y 11 de ellos, además, anticuerpos específicos (9 anticentrómero, uno anti-Scl70 y otro, anti-RNPC). La positividad de anticuerpos antinucleares se asoció con una mayor probabilidad de presentar una CP de esclerodermia, y ningún paciente diagnosticado de una enfermedad reumática tras la CP tenía un patrón normal.
ConclusiónLa CP es una técnica útil, pero con impacto limitado en el diagnóstico de enfermedades del tejido conectivo. La positividad de los anticuerpos se relaciona con una mayor probabilidad de presentar patrones patológicos en la CP.
Nailfold capillaroscopy (NC) is a non-invasive imaging technique for observation of microcirculation at nail cuticle level.1 It is a simple, safe, rapid and reproducible method and its interpretation is reliable.2 As a result of all of the above this imaging technique is highly useful and greatly requested in clinical practice, particularly for the diagnosis and follow-up of connective tissue diseases.
The main indication of NC is for the presence of a Raynaud phenomenon (RP).3 RP is the clinical manifestation of an overemphasised vasoconstriction to cold or stress.4 The presence of RP is also frequent in systemic diseases of connective tissue, particularly in systemic sclerosis (SS),5 inflammatory myopathies6 and mixed connective tissue disease (MCTD). NC is useful in distinguishing a primary RP, without any disease association and a secondary RP which is connective tissue disease associated.
Several studies have revealed that a high percentage of patients with RP and a capilaroscopic pattern of scleroderma will develop SS after several months or years, whilst in patients with RP but with no capilaroscopic alterations only 12.6% will subsequently develop sclerodermia.7
It is not possible in any cases for us to establish a diagnosis of progressive systemic scleroderma or any other disease on the basis of RP and a certain scleroderma pattern, however apparent this may be.8
The changes observed in the capillaries include changes to capillary density; size and shape of capillaries; neoangiogenesis phenomena and the presence of hemosiderin deposit by capillary micro-haemorrhages. The exclusive differentiated patterns are associated with SS but similar changes may be visible in other diseases (for example inflammatory myopathies or MCTD).
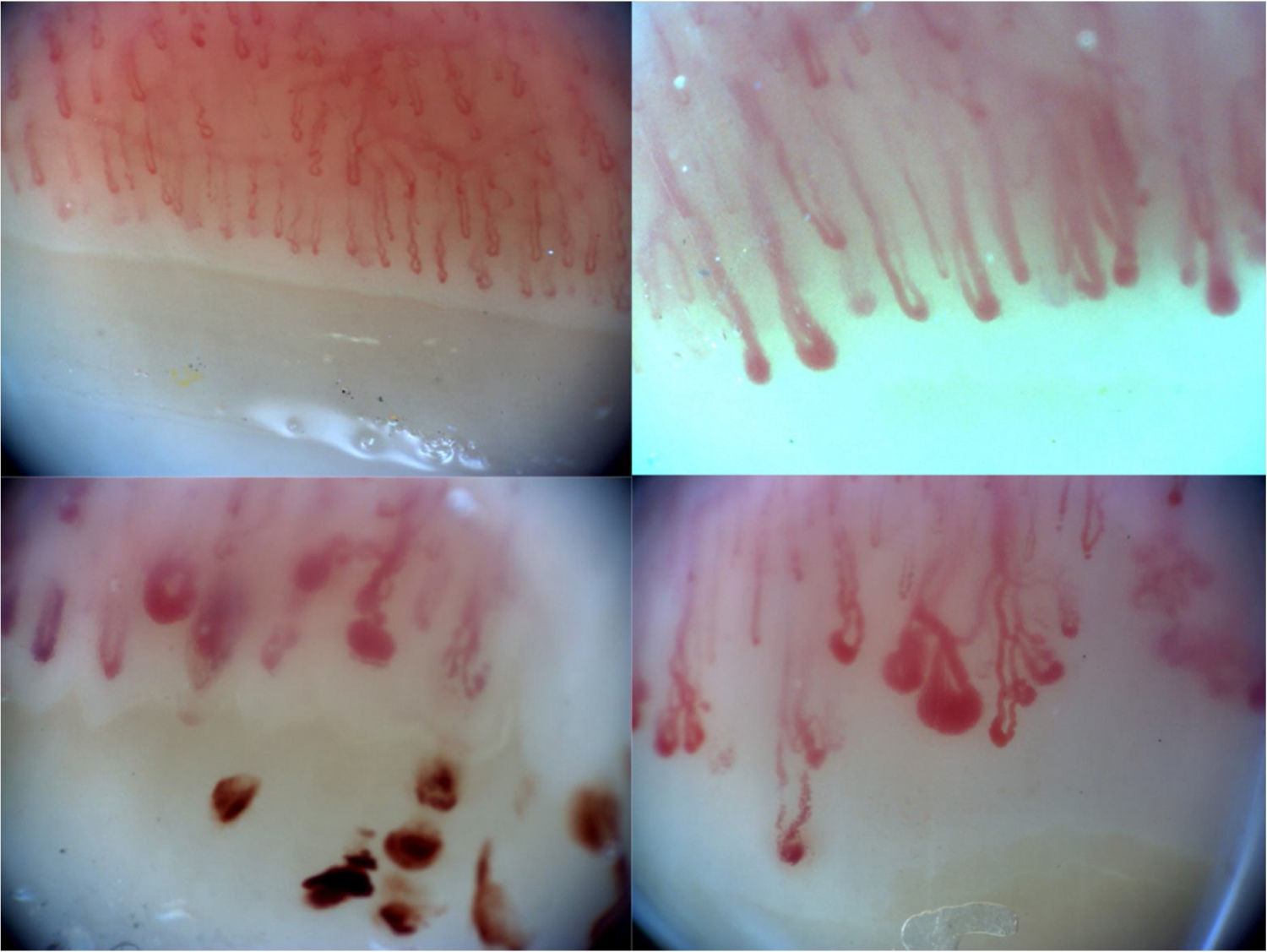
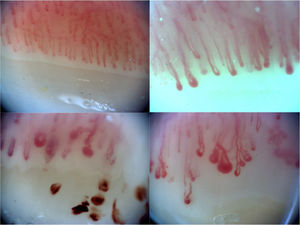
The normal appearance of the nailbed has non dilated capillaries which are parallel to one another and perpendicular to the nailbed, with 1–2 capillaries per papilla and in total 9–13 capillaries per millimetre. A normal NC does not present with neoangiogenesis, micro-haemorrhages or mega-capillaries. The early scleroderma pattern is characterised by the presence of capillary afferent and efferent loop dilatations, in addition to mega-capillaries (>50μm), with the maintenance of a normal capillary density and without any micro-haemorrages.6 The active scleroderma pattern is characterised by the presence of capillary dilatations, neoangiogenesis or avascular areas accompanied by capillary micro-haemorrhages. The delayed scleroderma pattern is characterised by the presence of mega-capillaries, reduction of capillary density, vascular areas and neoangiogenesis.7 The 4 previously described patterns are shown in Fig. 1.
The capilaroscopic patterns of scleroderma have been related to a higher risk of digital ulcers, pulmonary hypertension, interstitial pneumopathy, and calcinosis in patients with SS.9–11 Since 2013, the ACR/EULAR classification criteria include NC as an important criteria in the detection of very early sclerosis, for its capacity to show very early changes in the disease progression.12,13 However, its use in other connective tissue diseases remains controversial, as occurs with systemic erythematosus lupus, dermatomyositis, polymyositis, Sjögren's syndrome, rheumatoid arthritis and ankilosing spondylitis.6,14,15
Due to all of this, NC is commonly requested in clinical practice, but its use has scarcely been studied in this area.16 Our study assessed the impact of NC in diagnosis in daily clinical practice according to the reason for the request and the autoantibody profile.
Material and methodsThis was a clinical, observational, longitudinal and descriptive study. All patients with at least one NC between June 2012 and December 2017 were included. The NC were carried out by 2 rheumatologists who were experts in the technique (MMA and JCN) on a weekly basis with a video capillaroscopy of 220× magnification (from 2012 to 2015 with USB microscopy and from 2016 to 2017 with Optopix). After each examination an electronic report was issued with the description of findings and the conclusion with a capilaroscopic pattern.
The possible NC patterns were as follows: (1) normal pattern, with no changes; (2) pattern with slight non-specific changes, undulations or other occasional variants to normality; (3) pattern with moderate, non-specific changes, undulations in over 50% of capillaries and/or non pathological dilatations; (4) early scleroderma patterns, active and delayed, according to EULAR definitions.7
Clinical histories were reviewed and it was determined dichotomically (yes or no) whether the diagnosis or systemic treatment of the patient had changed in the later NC consultation. For those patients who demonstrated a change diagnoses and treatment changes were reported.
The reason for the request of the test was reported, together with the original referral, and the diagnosis of the patient if they had one, in addition to demographic data (age and sex), clinical data (presence of RP and digital ulcers) and laboratory data (autoantibodies). The study was approved by the ethical committee of our hospital.
Frequency data were expressed in percentages and the continuous variables in mean and intrerquartile range. The Student's t-test or the Chi-square test was applied depending on group comparisons. The Chi-square test was used to determine p, since the variables were qualitative.
ResultsThe number of examinations carried out on 535 patients was 734. Five patients were removed from the analysis because no demographic or laboratory data was available for them. The repetition of 2 or more NC occurred in 140 patients, 3 NC or more in 44 patients, 4 NC or more in 12 patients (all with SS) and 5 NC in 3 patients.
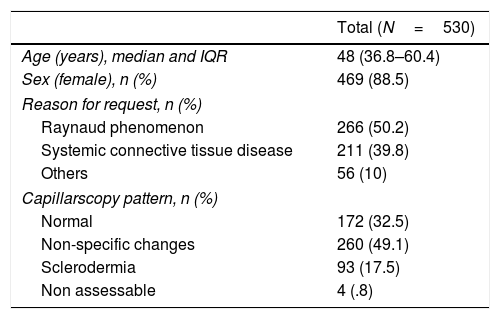
Table 1 shows the demographic data of the remaining 530 patients. Patients had been referred from rheumatology in 89.4% of cases (474 patients), and the remaining 10.6% (56 patients) from other specialties, mainly internal medicine (46 patients). The group of patients with a systemic connective tissue disease included people with systemic erythematous lupus, Sjögren's syndrome, inflammatory myopathies (dermatomyositis and polymyositis), MCTD and undifferentiated connective tissue diseases. Of the 530 patients, a change in diagnosis occurred in posterior consultation in 20 cases (3.8%) in those who requested the NC for RP.
Demographic patient data of patients who underwent at least one capillaroscopy.
| Total (N=530) | |
|---|---|
| Age (years), median and IQR | 48 (36.8–60.4) |
| Sex (female), n (%) | 469 (88.5) |
| Reason for request, n (%) | |
| Raynaud phenomenon | 266 (50.2) |
| Systemic connective tissue disease | 211 (39.8) |
| Others | 56 (10) |
| Capillarscopy pattern, n (%) | |
| Normal | 172 (32.5) |
| Non-specific changes | 260 (49.1) |
| Sclerodermia | 93 (17.5) |
| Non assessable | 4 (.8) |
IQR: interquartile range.
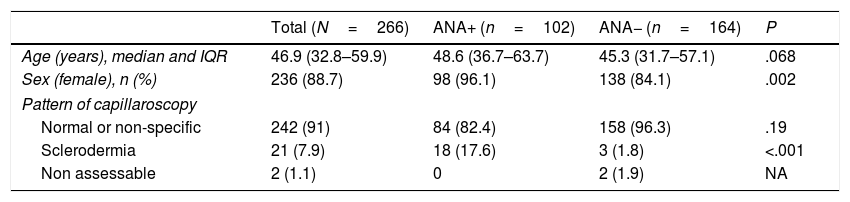
The most common reason for request was RP (266 patients), and the autoantibody profile (positive or negative antinuclear antibodies [ANA]) distinguishes 2 different groups in relation to the result of the NC and the changes in diagnosis. Table 2 contains the characteristics of both groups. Out of the 20 patients with RP and changes in diagnosis, 15 were diagnosed with SS, 4 with connective tissue diseases and one with MCTD. Of these, all except one patient had positive ANA and 11 of them had specific antibodies (9 anticentromere, one anti-Scl70 and another anti-RNPC). The capilaroscopic patterns of the patients with changes to diagnosis were: 12 patients (51.7%) with a scleroderma pattern, 8 patients (48.3%) with non-specific changes and no patients with normal NC. The positivity of ANA was associated with a higher probability of presenting with a capillaroscopy scleroderma pattern (P<.001). All the patients who had been diagnosed with sclerosis met with the ACR/EULAR 2013 classification criteria.12
Patients with capillaroscopy requested due to Raynaud phenomenon according to the positivity of antinuclear antibodies.
| Total (N=266) | ANA+ (n=102) | ANA− (n=164) | P | |
|---|---|---|---|---|
| Age (years), median and IQR | 46.9 (32.8–59.9) | 48.6 (36.7–63.7) | 45.3 (31.7–57.1) | .068 |
| Sex (female), n (%) | 236 (88.7) | 98 (96.1) | 138 (84.1) | .002 |
| Pattern of capillaroscopy | ||||
| Normal or non-specific | 242 (91) | 84 (82.4) | 158 (96.3) | .19 |
| Sclerodermia | 21 (7.9) | 18 (17.6) | 3 (1.8) | <.001 |
| Non assessable | 2 (1.1) | 0 | 2 (1.9) | NA |
ANA: antinuclear antibodies; NA: not applicable; IQR: interquartile range.
NC is a highly requested imaging technique in clinical practice for the study of RP and connective tissue diseases. Despite most of the results being normal or non-specific, the presence of pathological patterns may impact the decision-making of diagnosis and treatment. In our study, the negativity of the ANA was related to normal capillaroscopy or non-specific capillaroscopy in the great majority of patients and consequently with no changes to diagnosis of rheumatoid diseases.
NC is highly useful in the diagnosis and follow-up of SS but its use in other connective tissue diseases is controversial. However, there are many requests for capillarsocopy for patients with other rheumatoid diagnoses where a request is made to assess an RP. It has been proven that non pathological capillaroscopy together with negativity of autoantibodies has a high predictive negative value leading to the ruling out of a systemic disease and our results are consequently consistent with this.17
NC should be interpreted jointly with the results of autoimmunity and on occasions it is necessary to have a gradual follow-up to determine the capilaroscopic change over time, particularly in those patients with positive ANA.18,19 In our study, the positive ANA were more greatly associated with the presence of a scleroderma pattern, which helped in diagnosing SS in 3 out of every 4 patients with pathological NC (P<.001). Furthermore, patients for whom more than 3 NC were requested were those who had been diagnosed with sclerosis, with 3 normal NC or non-specific NC being sufficient to rule out rheumatoid disease. The basic RP study should therefore include autoimmunity analysis and a NC.13
Table 2 reflects those patients who underwent a NC with a previous diagnosis of RP, among whom there were 11 patients who did not have an ANA determination. This was due to the fact that most of the patients who undergo NC had the request for it made during their first visit, and this was performed prior to the determination of autoantibodies.
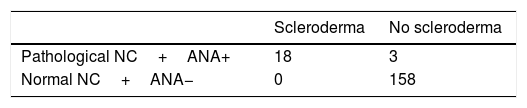
Changes in the NC have been shown to relate to greater involvement of organs and have a predictive value regarding disease progression.20–22 Early detection of changes in NC may help us to take different therapeutic decisions which in some cases may change the course of the disease. Table 3 calculates the positive and negative predictive value for the diagnosis of sclerosis in patients with RP and a pathological NC with positive ANA versus normal NC with negative ANA. These data are close to those published in the literature.23,24
Our study has certain limitations that need mentioning. The descriptive and observational nature of the study suffers from the usual limitations: unavailable data, patient selection bias, etc. However, this is a normal reality in clinical practice which may be comparable to that occurring in other centres of rheumatology with their own capillaroscopy scheduling. The lack of progressive data impedes capillaroscopic pattern developmental analysis in patients with an initial normal or non-specific NC and positive autoantibodies, which would be of great interest for capillaroscopic follow-up. However, this aspect has been described in other studies, with the involvement of autoantibodies leading to greater probability of progression in the NC pattern.18,19
Internationally accepted capilaroscopic patterns are the 3 scleroderma ones (early, active and delayed) and the normal pattern. It is however common for patients to present with non-specific changes which do not completely match any of the previous patterns. In an arbitrary way, in our centre we decided to classify this type of pattern with non-specific changes and to graduate them according to their severity into mild and moderate. We are aware that this is a subjective graduation and a limitation of our study.
ConclusionsTo conclude, NC is a highly requested technique in clinical practice, with a limited impact on diagnosis. It enables rheumatoid disease to be ruled out in the presence of negative ANA and normal NC, although further studies are required to sustain this statement.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Torrens Cid LA, Soleto K CY, Montoro-Álvarez M, Sáenz Tenorio C, Silva-Riveiro A, López-Cerón A, et al. Impacto clínico de la capilaroscopia periungueal en la práctica clínica diaria. Reumatol Clin. 2021;17:258–262.