The description of the controversy regarding the use of Doppler ultrasound or biopsy published by González Porto et al. is of very high quality. The authors conclude that ultrasound scan is of restricted usefulness in giant cell arteritis (GCA) and recognise that there is a need for prospective studies.1 We also consider the reply by de Miguel et al.2 to be highly relevant, with its description of technical and methodological data, and we would like to add a few remarks with the aim of improving the procedure for ultrasound scan in GCA.
According to the recent EULAR 20183 recommendations, it is important to use a multifrequency transponder, and it is recommended that one of less than 15 MHz be used, as de Miguel et al. remark. In our experience we too use frequencies of 15 MHz for a scale of greys and Doppler in colour (60% gain and PRF of 1,5–2 kHz), and all such tasks are performed by ultrasound technicians who have been trained in the said technique. One very important detail is that we must not restrict evaluation to the superficial temporal arteries. According to the data published by Schäffer et al.4 we should measure and evaluate the inner and middle layers of the common superficial temporal artery (cut point: 0.42 mm), the parietal branch (0.29 mm), the frontal branch (0.34 mm), the facial artery (0.37 mm) and the axillary artery (1.0 mm), as all of these have a sensitivity of from 87% for the lowest up to 100%.
It is here where, as was said, the procedure has gradually been improved, and training in the said technique may improve the sensitivity parameters (S) and the specificity parameters (E). When they reviewed their data, de Miguel et al. found that they had improved over the years, until they obtained S of 91.6% and E of 95.83%.5 In our case, in 2018 we obtained an S and E of 81.8 and 93.3%, respectively, with a positive predictive value of 90.1% and a negative predictive value of 87.5%, all without evaluating the axillary artery, although it is now regarded as essential to do this.6
Finally, respecting the open debate on the utility of ultrasound scan imaging in GCA, which was awarded a score of 5 points, and the recent EULAR3 recommendations document, it is considered to be a test with very diagnostic value when performed by an expert. Likewise, it must be said that there are other complementary imaging techniques which should be evaluated to detect wall or luminal inflammation in extracraneal arteries in the case of large vessel vasculitis such as GCA. It also has to be pointed out that ultrasound scan is of limited value in cases of aortitis.3
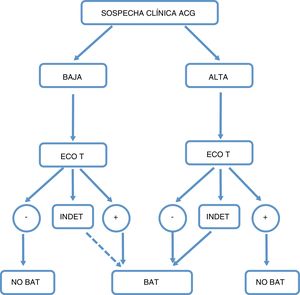
We understand that an algorithm should be used to decide whether a cohort has low or high clinical suspicion, deciding on the basis of the result whether or not to perform a superficial temporal artery biopsy. Nevertheless, this algorithm deserves its own particular debate (Fig. 1).
Proposed algorithm for action in case of suspicion of giant cell arteritis (GCA).
High level of clinical suspicion: age >50 years old and 1) with exclusively cephalic symptoms (cephalea that commenced recently, jaw claudication or visual alterations); 2) with rheumatic polymyalgia, according to EULAR/ACR 2017 criteria; 3) with toxic syndrome or non-specific fever syndrome, once infectious causes have been ruled out and screening for neoplasia has proved negative, and 4) with ictus in vertebrobasilar territory, with no relevant cardiovascular history or findings with an atherogenic or embolic etiology after a directed study.
GCA: giant cell arteritis; TAB: temporal artery biopsy; TAUS: temporal artery ultrasound scan; INDET: indeterminate result.
Please cite this article as: Corominas H, Estrada Alarcón P, Moya P, Sanz DR. Comparativa entre ecografía Doppler frente a la biopsia de arteria temporal en el diagnóstico de la arteritis de células gigantes. Debate abierto. Reumatol Clin. 2021;17:121–122.