Sarcoidosis is a systemic granulomatous disease with a wide range of clinical manifestations. Skin involvement is an early, frequent and accessible location for a histopathological study. Several risk factors have been described to determine the likelihood of systemic involvement of an apparent cutaneous condition. Early diagnosis and systemic treatment could prevent future complications.
A series of three cases is presented in which the initial diagnosis was cutaneous sarcoidosis, but it was actually the first manifestation of a systemic disease. A review of this topic is also presented.
La sarcoidosis es una enfermedad granulomatosa sistémica con un gran abanico de manifestaciones clínicas, siendo la afectación cutánea una de las más precoces, frecuentes y accesible de un estudio histopatológico. En la actualidad, se han descrito varios factores de riesgo que determinarán la probable afectación sistémica de una aparente afectación cutánea única. Esta correcta valoración establecerá el inicio de un tratamiento sistémico, previniendo de esta forma futuras complicaciones.
Se presenta a continuación una serie de 3 casos de sarcoidosis cutánea como primera manifestación de una enfermedad sistémica paucisintomática y se hace una revisión del tema.
Sarcoidosis is a systemic granulomatous disease of unknown etiology and with a wide range of clinical signs. It occurs throughout the entire world, affecting more women than men (2:1), and the distribution by age is bimodal (25–35 and 45–55 years). The histological hallmark is the presence of uniform noncaseating granulomas with few peripheral lymphocytes (naked granulomas).1
Pulmonary involvement is the most common clinical sign (90%), followed by cutaneous (35%), hepatosplenic, ocular and exocrine (parotid) gland involvement, whereas central nervous system, cardiac, upper respiratory tract and musculoskeletal involvement are less frequent, but more severe.1 Although cutaneous involvement in sarcoidosis can develop throughout the course of the disease, it is most frequently present at the onset (30%). Thus, biopsy and histopathological study of the lesion will enable an early diagnosis.2
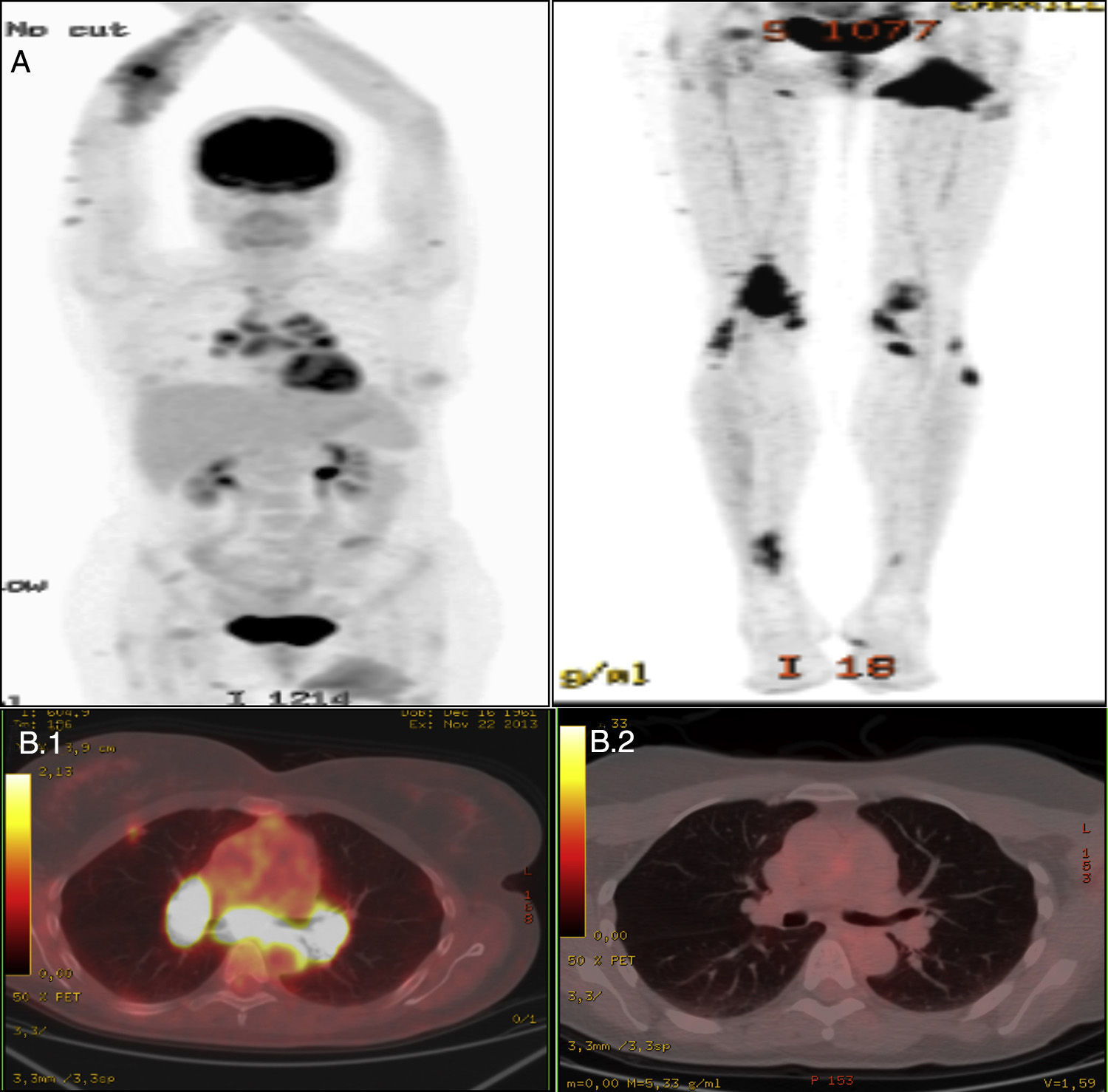
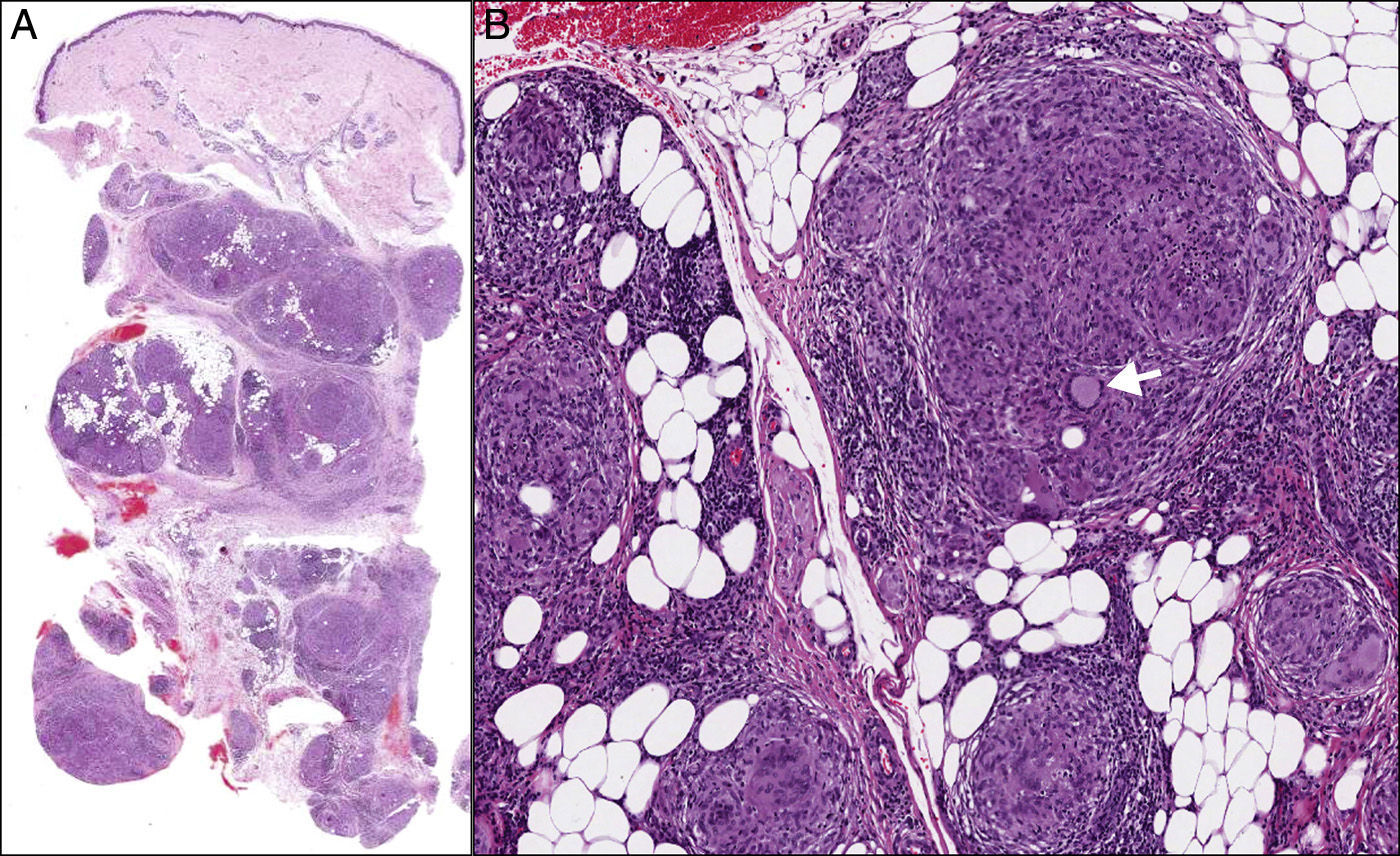
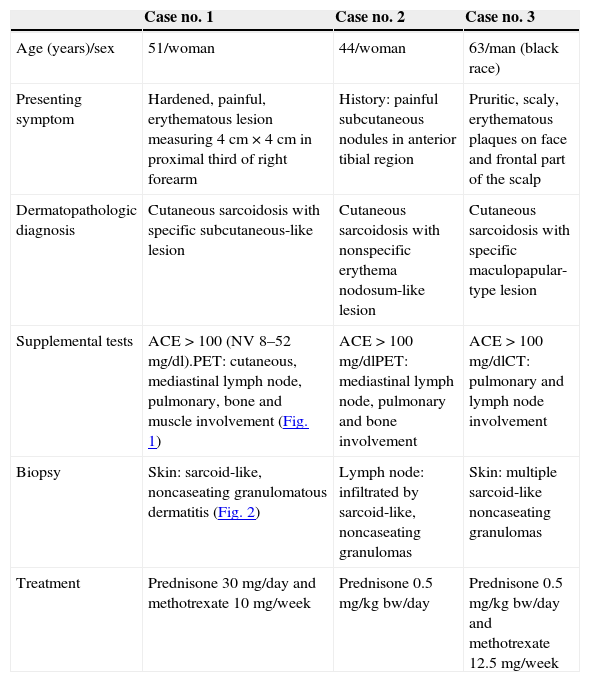
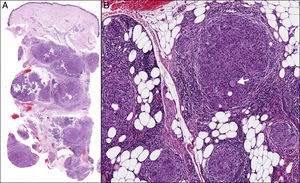
Case ReportsWe present a series of three patients in whom the first finding was an apparently isolated skin lesion. Given the characteristics of the lesion, the initial results of supplemental tests and a histopathological study compatible with cutaneous sarcoidosis, a more comprehensive study was carried out, which revealed asymptomatic/paucisymptomatic systemic involvement. Treatment was begun with systemic prednisone at 0.5mg/kg body weight/day in a tapering regimen, associated with 5–6 months of methotrexate administration in cases nos. 1 and 3, after which an improvement was observed in the clinical findings and supplemental test results (Table 1 and Figs. 1 and 2).
Clinical Characteristics and Results of Supplemental Tests.
| Case no. 1 | Case no. 2 | Case no. 3 | |
|---|---|---|---|
| Age (years)/sex | 51/woman | 44/woman | 63/man (black race) |
| Presenting symptom | Hardened, painful, erythematous lesion measuring 4cm×4cm in proximal third of right forearm | History: painful subcutaneous nodules in anterior tibial region | Pruritic, scaly, erythematous plaques on face and frontal part of the scalp |
| Dermatopathologic diagnosis | Cutaneous sarcoidosis with specific subcutaneous-like lesion | Cutaneous sarcoidosis with nonspecific erythema nodosum-like lesion | Cutaneous sarcoidosis with specific maculopapular-type lesion |
| Supplemental tests | ACE>100 (NV 8–52mg/dl).PET: cutaneous, mediastinal lymph node, pulmonary, bone and muscle involvement (Fig. 1) | ACE>100mg/dlPET: mediastinal lymph node, pulmonary and bone involvement | ACE>100mg/dlCT: pulmonary and lymph node involvement |
| Biopsy | Skin: sarcoid-like, noncaseating granulomatous dermatitis (Fig. 2) | Lymph node: infiltrated by sarcoid-like, noncaseating granulomas | Skin: multiple sarcoid-like noncaseating granulomas |
| Treatment | Prednisone 30mg/day and methotrexate 10mg/week | Prednisone 0.5mg/kgbw/day | Prednisone 0.5mg/kgbw/day and methotrexate 12.5mg/week |
ACE: angiotensin-converting enzyme; CT: computed tomography; NV: normal value; PET: positron emission tomography.
Nuclear medicine study of case no. 1. (A) Scintigraphic study showing an active inflammatory process affecting upper and lower limbs, mediastinal lymph nodes, lung parenchyma, bone and left gluteal muscle. (B.1) Positron emission tomography (PET) study showing mediastinal lymph node involvement prior to treatment. (B.2) PET study following treatment.
Cutaneous sarcoidosis is relatively common and constitutes a diagnostic challenge for medical specialists, as it may be an early symptom of probable asymptomatic systemic involvement (9%–37%), the extent of which will be proportional to the affected body surface area.3 Although, in the past, the cutaneous manifestations were not considered to be implicated in the prognosis of the disease,4 at the present time, there are increasing reports of this real and strong association, which, in fact, constitutes the only initial sign in over 50%–80% of the cases.5,6
The prognosis of sarcoidosis is generally good, with spontaneous resolution in nearly 60% of those affected. However, some patients progress to a chronic disease with a mortality of 1%–6%.7 The risk factors for progression are black race, age >40 years, lupus pernio, extensive cutaneous involvement, nasal mucosal involvement, chronic uveitis, chronic hypercalcemia, nephrocalcinosis, bone lesions, highly elevated angiotensin-converting enzyme levels, abnormal findings in the study of the bronchoalveolar lavage sample (CD4/CD8>3.5, lymphocytosis>28%), neurosarcoidosis and cardiac involvement.7,8
Positron emission tomography currently constitutes a useful tool in the diagnosis and follow-up of sarcoidosis, even in cases of occult or asymptomatic involvement. It is more sensitive and requires a 3-fold lower radiation dose than gallium scintigraphy.9
Treatment is based on the administration of high-dose systemic corticosteroids (oral prednisone at a dose of 0.5mg/kgbw/day) in a tapering regimen, associated in some cases with immunosuppressive drugs. The list of the latter is long and, to date, there are no studies with a high level of evidence and grade of recommendation that demonstrate the superiority of any given agent over the others. However, the available studies recommend the use of methotrexate (10–15mg/week) as the drug of choice.1,10
Thus, the presence of suggestive lesions should activate a protocol of supplemental tests aimed at confirming the lesion type and assessing the extent of the disease; on the basis of the results, and in view of the poor prognosis associated with the detected risk factors, the decision will be made to begin systemic therapy in order to prevent future complications.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of InterestThe authors declare that they have no conflicts of interest.
We thank the Departments of Pathology and Nuclear Medicine of Hospital General Universitario de Ciudad Real, Spain, for the facilities provided.
Please cite this article as: Ramírez Huaranga MA, Ramos Rodríguez CC, de la Rocha Vedia IV, García Arpa M, Murillo Lázaro C, Bellón Guardia M. Sarcoidosis cutánea: el preámbulo de una enfermedad sistémica paucisintomática. Reumatol Clin. 2015;11:395–397.