The association of dermatomyositis with myasthenia gravis (MG) is uncommon, having been reported so far in only 26 cases. We report the case of a 69 year-old man diagnosed with MG two years ago and currently treated with piridostigmyne. The patient developed acute proximal weakness, shoulder pain and elevated creatine-kinase (CK). He also developed generalized facial erythema and Gottron's papules. Laboratory tests showed positive antinuclear and anti-Mi2 antibodies. Further analysis confirmed CK levels above 1000U/l. The clinical management of the patient and the therapeutic implications derived from the coexistence of both entities are discussed.
La asociación de dermatomiositis y miastenia gravis (MG) es infrecuente, habiéndose comunicado hasta la actualidad únicamente 26 casos. Se presenta el caso de un varón de 69 años diagnosticado de MG 2 años atrás, en tratamiento con piridostigmina, que inicia cuadro agudo de debilidad muscular proximal, artralgias en hombros y elevación de creatincinasa (CK); así como aparición de eritema facial generalizado y pápulas de Gottron. En el estudio de laboratorio se evidenció positividad de anticuerpos antinucleares y anti-Mi2. Ulteriores determinaciones de CK mostraron niveles por encima de 1.000U/l. Se discute el manejo clínico de este paciente y las implicaciones terapéuticas que plantea la coexistencia de ambas entidades.
Idiopathic inflammatory myopathies (IIM), including dermatomyositis (DM), are a heterogeneous group of systemic autoimmune diseases whose main clinical feature is predominantly proximal muscle weakness.1 They are rare diseases, with an estimated annual incidence of 6 cases/105 individuals2 and may be associated with other autoimmune diseases such as lupus or Sjogren's syndrome.
Another autoimmune disease that causes muscle weakness, myasthenia gravis (MG), can also be associated with the IIM.3–9 MG is rare, with an estimated prevalence of 140 cases/106 inhabitants.10 Its pathogenesis derives from the compromise resulting from the binding of autoantibodies to proteins involved in the neuromuscular transmission signaling. Recognizing the association between the two entities is important due to its therapeutic implications. We present a case of DM in a patient previously diagnosed with MG.
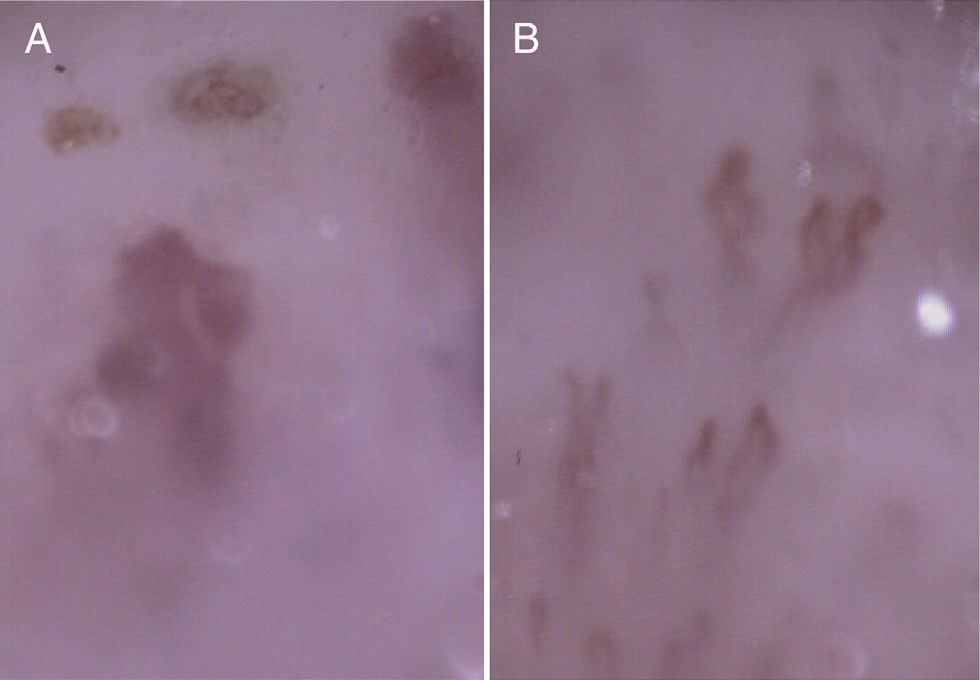
Clinical CaseThe patient was a 69 year-old-male Caucasian, diagnosed two years prior with MG, positive to anti-AChR antibodies and treated with pyridostigmine (60mg/8h). He was referred to our center due to the appearance of weakness which appeared a month before, manifested by difficulty dressing or getting out of bed, shoulder joint pain and elevated creatine kinase (CK). He had presented diffuse facial erythema for 6 months. The physical examination showed cuticular thickening and bleeding, Gottron's papules (Fig. 1) and facial erythema and on the neckline (Fig. 2) He had proximal muscle weakness in the upper and lower limbs (4/5). The rest of the examination was normal.
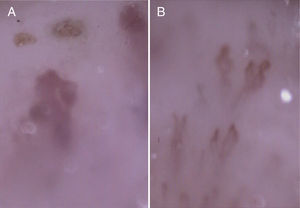
The laboratory exams highlighted CK 1254U/l. Antinuclear antibodies were positive (>1/160, with a granular pattern, and anti-ENA and anti-DNA were negative) as well as the anti-Mi2. Nailfold capillaroscopy showed a pattern suggestive of DM (Fig. 3).
Electromyography showed a myopathic pattern with proximal predominance in the upper limbs. A muscle biopsy was not considered necessary. Given the high sensitivity of the test for occult neoplasia, a PET-CT was performed and was normal.
With the diagnosis of DM, prednisone (1mg/kg/day) was started. After three weeks, significant improvement of skin lesions was observed, but muscle weakness persisted, with added dysphagia. CK levels increased to 3800μ/l. Weekly methotrexate (h 20mg/week SC) and a course of high-dose intravenous immunoglobulins was added to treatment. The patient showed improvement in muscle strength and swallowing, as well as disappearance of Gottron's papules, with gradual decrease in CK.
DiscussionThe association of MG to MII is very rare, with 26 cases3–9 having been communicated until the present. It is important to know of this association because it has therapeutic implications. Unlike patients with IIM, MG presents with fluctuating weakness that worsens with activity and during the course of the day. In addition, a real muscle fatigability in IIM is not characteristic, while it is a typical clinical characteristic of MG. In most patients with MG, the eye muscles are initially affected, causing intermittent diplopia and ptosis, symptoms that are not observed in the IIM. Proximal muscle weakness is a common symptom of MG and in DM, appearing with bulbar symptoms such as dysphagia or dysarthria.
Treatment of MG includes anticholinesterase although not all patients respond. As in IIM, glucocorticoids, immunosuppressants and immunomodulators–intravenous immunoglobulin–are frequently used in MG. The usual pattern of steroid use in DM is high prednisone doses (1mg/kg/day) with subsequent gradual tapering. However, in MG it is recommended to start with a low dose and gradually increase due to risk of exacerbation of weakness.10
In summary, MG may precede or complicate the course of IIM. Knowing this association is important because it requires different handling and treatment, with a gradual intensification of therapy with glucocorticoids.
Ethical ResponsibilitiesProtection of people and animalsThe authors declare this research did not perform experiments on humans or animals.
Data confidentialityThe authors declare that they have followed the protocols of their workplace regarding the publication of patient data.
Right to privacy and informed consentThe authors have obtained the informed consent of patients and/or subjects referred to in the article. This document is in the possession of the corresponding author.
Conflict of InterestThe authors have no conflict of interest to state.
Please cite this article as: Sangüesa Gómez C, Flores Robles BJ, Méndez Perles C, Barbadillo C, Godoy H, Andréu JL. Dermatomiositis y miastenia gravis: una asociación infrecuente con implicaciones terapéuticas. Reumatol Clin. 2015;11:244–246.