Sarcoidosis is a complex disease of unknown aetiology, with a variable course and highly different forms of presentation. Our objective was to characterize all our patients with sarcoidosis with emphasis on their clinical presentation and to establish differences between patients with sarcoidosis with and without joint involvement.
MethodsWe reviewed the medical records of all patients with a diagnosis of sarcoidosis who were treated at the outpatient or inpatient services of the Pablo Tobón Uribe Hospital in Medellín, Colombia, from January 2002 to April 2017.
ResultsWe identified 22 patients with sarcoidosis. There were joint symptoms in 13 of them. All but one of the patients with sarcoidosis affecting the joints had concomitant skin involvement (92%), which was much less frequent in patients without joint involvement (22%) (odds ratio=4.2; P<.001).
ConclusionsPatients with sarcoidosis who have joint involvement have a much higher frequency of concomitant skin involvement. The absence of cutaneous findings in a patient with joint symptoms decreases the likelihood of sarcoidosis.
La sarcoidosis es una enfermedad compleja, de etiología desconocida, de curso variable y con formas de presentación diversas. Nuestro objetivo fue caracterizar a todos nuestros pacientes con sarcoidosis con énfasis en su forma de presentación clínica y establecer diferencias entre los pacientes con sarcoidosis con y sin compromiso articular.
MétodosSe revisaron las historias clínicas de todos los pacientes con diagnóstico de sarcoidosis que fueron atendidos en el Hospital Pablo Tobón Uribe de Medellín, Colombia, desde enero de 2002 hasta abril de 2017.
ResultadosSe encontraron 22 pacientes con sarcoidosis. Hubo síntomas articulares en 13 de ellos. Todos los pacientes con sarcoidosis articular, excepto uno, tuvieron compromiso cutáneo concomitante (92%), lo cual fue mucho menos frecuente en los pacientes sin compromiso articular (22%) (OR=4,2; p<0,001).
ConclusionesLos pacientes con sarcoidosis que tienen compromiso articular presentan una frecuencia mucho mayor de compromiso cutáneo concomitante. La ausencia de hallazgos en piel en un paciente con síntomas articulares disminuye la probabilidad de que se trate de sarcoidosis.
Sarcoidosis is a multisystem granulomatous disease with heterogeneous clinical features. Many consider it to be a diagnostic challenge, not just for the complexity of its symptoms but also for its similarity to other multisystem diseases, such as autoimmune infections and diseases.1
As far as we are aware, in Colombia the only information available has been supplied by: a series of 51 patients from 9 hospital centres in Bogotá and published 40 years ago,2 a series of 34 patients presented in a summary format report in Cali, Colombia, which underlines a high frequency of bone and joint involvement (Cañas et al., face-to-face communication), a series of 7 paediatric cases in Bogotá3 and another of 8 adult patients in Santander.4 Apart from these series and reports of isolated cases,5–7 we have no available information on the disease and its symptoms in our environment, nor do any details exist of the characteristics of joint involvement.
The aim of this study was to describe the characteristics of a group of adult Colombian patients with sarcoidosis, which we consider would lead to a better understanding of the clinical behaviour of the disease in our region.
Patients and methodsA cross-sectional study was conducted to characterize our patients with sarcoidosis and try to establish whether there were differences between those with sarcoidosis with and without joint involvement. All consecutive patients with a clinical diagnosis of sarcoidosis treated in the Hospital Pablo Tobón Uribe de la ciudad de Medellín, in Colombia, assessed between January 2002 and April 2017 were included. The diagnoses were established by the treating physicians through a combination of clinical symptoms, laboratory tests, imaging studies or results from biopsies, depending on the application in each case and after ruling out infectious processes, neoplasms or other chronic inflammatory diseases. We defined the case study example to be the patient with sarcoidosis and any type of joint involvement and the control example as patients with sarcoidosis with no type of joint involvement. All the patients registered on the electronic medical record of the Hospital were included and demographic and medical information relating to how the disease began was collected, along with the medical events during follow-up, the result of the diagnostic aids, the treatments supplied and the patient evolution.
Qualitative variables are presented as frequencies and percentages and quantitative variables as medians and interquartile range. For qualitative variable analysis the exact Fisher test was used and for quantitative variables the Mann–Whitney U test was used. Analyses were performed using the Stata version 11 statistical programme.
Due to the fact that this study was exclusively based on clinical records, it was considered to be a research study without risk and no informed consent was necessary. This study was approved by the Ethics Committee of the Unite of Research and Teaching of the Hospital Pablo Tobón Uribe.
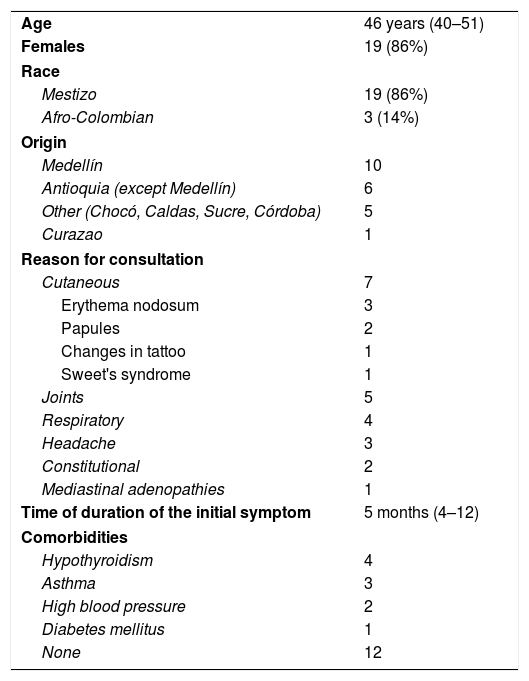
ResultsTwenty two patients who had been diagnosed with sarcoidosis were found, of whom 19 (86%) were women. The median age was 46 years (IQR: 40–51). There were 3 Afro-Colombian patients and 19 mestizo patients. The main reason for consultation were skin and joint symptoms. The median duration of symptoms until diagnosis was 5 months (IQR: 4–12) (Table 1).
Description of the population.
| Age | 46 years (40–51) |
| Females | 19 (86%) |
| Race | |
| Mestizo | 19 (86%) |
| Afro-Colombian | 3 (14%) |
| Origin | |
| Medellín | 10 |
| Antioquia (except Medellín) | 6 |
| Other (Chocó, Caldas, Sucre, Córdoba) | 5 |
| Curazao | 1 |
| Reason for consultation | |
| Cutaneous | 7 |
| Erythema nodosum | 3 |
| Papules | 2 |
| Changes in tattoo | 1 |
| Sweet's syndrome | 1 |
| Joints | 5 |
| Respiratory | 4 |
| Headache | 3 |
| Constitutional | 2 |
| Mediastinal adenopathies | 1 |
| Time of duration of the initial symptom | 5 months (4–12) |
| Comorbidities | |
| Hypothyroidism | 4 |
| Asthma | 3 |
| High blood pressure | 2 |
| Diabetes mellitus | 1 |
| None | 12 |
Fourteen patients had alterations to pulmonary functions and were distributed into: class I: 6; class II: 5, and class III: 3. None of our patients had any reported cardiac, muscular or neurological symptoms or alterations. Skin alterations were found in 14 of the 22 patients, mainly erythema nodosum, papules, changes to a tattoo in one patient and Sweet's syndrome in another. Joint symptoms were reported in 13 patients, with arthritis of the ankles in 8 (62%).
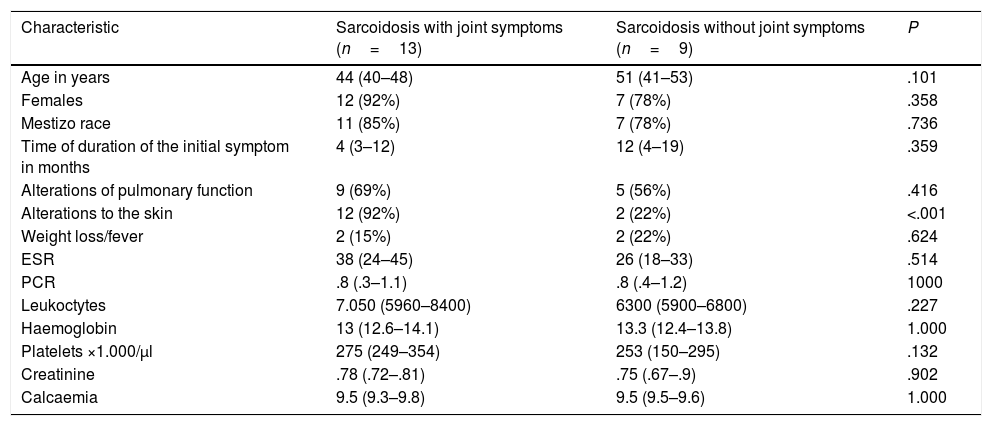
Table 2 compares the patients with sarcoidosis with and without joint involvement. No differences between these two groups were observed, except for a marked difference which was statistically significant with relation to the skin manifestations. All the patients with joint sarcoidosis, except one, had concomitant skin involvement (92%), which was much less frequent in the patients without joint involvement (22%) (OR=4.2; P<.001). In addition, the group with the joint involvement had a tendency for their symptoms to have a lower time of evolution prior to diagnosis (4 months [3–12] versus 12months [4–19], P=.359).
Comparison of the patients with sarcoidosis with and without joint involvement.
| Characteristic | Sarcoidosis with joint symptoms (n=13) | Sarcoidosis without joint symptoms (n=9) | P |
|---|---|---|---|
| Age in years | 44 (40–48) | 51 (41–53) | .101 |
| Females | 12 (92%) | 7 (78%) | .358 |
| Mestizo race | 11 (85%) | 7 (78%) | .736 |
| Time of duration of the initial symptom in months | 4 (3–12) | 12 (4–19) | .359 |
| Alterations of pulmonary function | 9 (69%) | 5 (56%) | .416 |
| Alterations to the skin | 12 (92%) | 2 (22%) | <.001 |
| Weight loss/fever | 2 (15%) | 2 (22%) | .624 |
| ESR | 38 (24–45) | 26 (18–33) | .514 |
| PCR | .8 (.3–1.1) | .8 (.4–1.2) | 1000 |
| Leukoctytes | 7.050 (5960–8400) | 6300 (5900–6800) | .227 |
| Haemoglobin | 13 (12.6–14.1) | 13.3 (12.4–13.8) | 1.000 |
| Platelets ×1.000/μl | 275 (249–354) | 253 (150–295) | .132 |
| Creatinine | .78 (.72–.81) | .75 (.67–.9) | .902 |
| Calcaemia | 9.5 (9.3–9.8) | 9.5 (9.5–9.6) | 1.000 |
For 15 years there were only 22 cases of sarcoidosis in our hospital, despite being a regional and national centre of reference with a permanent service for major specialties and where patients can come into the surgery for the first time. Unfortunately medical cover of the hospital is not universal, since the access of each patient depends, among other things, on geographic and administrative factors.
Our series included a predominance of women, great diversity of the clinical spectrum of the disease and a high rate of arthritis of the ankles. In contrast, in the recent series of 8 patients published by Santamaria-Alza and Fajardo4 half of the patients were men, and no mention was made of joint symptoms. In the series by Valovis2 51 cases were collected which came from 9 hospital centres in Bogotá. In this series there was also an equal distribution by sexes and it was mentioned that only 4 patients (8%) had joint symptoms. In the series of 34 patients presented as a summary by Cañas et al. (face-to-face communication), 14 had bone or joint symptoms (42%). In none of these series was any additional information reported to characterize the subgroup with joint symptoms.
Sarcoidosis may mimic acute or chronic arthropathies, spondyloarthritis, autoimmune granulomatous processes, vasculitis, myopathies, dry eye syndrome and systemic, cutaneous and ocular symptoms which form part of the everyday clinical practice of the rheumatologist.8 Sarcoidosis may compromise the musculoskeletal system in different ways, in muscles and in joints and bones.9 Up to 25% of patients with this disease present with arthritis,8 but it is not unusual that some publications completely fail to mention these clinical manifestations.4,10–12 Musculoskeletal symptoms in sarcoidosis are common and may be the first sign of the disease and therefore, the opportunity to make an early diagnosis.13
The standard classification for arthritis that may occur in sarcoidosis is acute or transitory and chronic or persistent arthritis, with the latter being much less frequent. Acute sarcoid arthritis often occurs in the context of a Löfgren's syndrome which is defined by the triad of erythema nodosum, bilateral hiliar lymphadenopathy and arthritis.8 It is widely known that bilateral arthritis of the ankle strongly suggests the diagnosis of sarcoidosis, with a 99% rate of sensitivity, and a 90% rate of specificity.8,14 Visser et al.15 studied 579 patients with arthritis of recent onset, among whom there were 55 with a final diagnosis of sarcoidosis, and they proposed several criteria to aid clinical diagnosis of sarcoid arthritis. In keeping with these criteria, a diagnosis of joint sarcoidosis may be established with a sensitivity of 99% and specificity of 93% in patients who present with at least 3 of the following 4 characteristics: erythema nodosum, less than 2 months since symptom onset, aged over 40 and bilateral arthritis of the ankles. After the ankles, the other most commonly affected joints are: knees, wrists, and metacarpophalangeal joints. What is striking is that in different reports of the literature the frequency of other clinical symptoms in patients with joint sarcoidosis is widely variable. For example, erythema nodosum may or may not be present, and an extensive range of between 25% and 87.8% has been reported.8,14
In this study we compared patients with and without joint symptoms, finding significant differences only in the frequency of concomitant skin involvement. Skin symptoms were the norm within the group with the joint involvement, but quite unusual within the group without this involvement. This major finding appears to have been little explored until now by other researchers.
Our study has several weak points, including the low number of patients finally included, the retrospective nature of the data collection, the absence of histological confirmation for all cases and the reference bias of our hospital.
The strong association between skin and joint symptoms in the patients with sarcoidosis could be a fairly useful piece of data for the initial focus of a patient with joint symptoms, in such a way that the absence of skin alterations would make it unlikely that this was sarcoidosis of the joints. Our study does however suggest that the absence of joint symptoms associated with a lower frequency of skin symptoms appears to delay patients seeking medical attention.1
ConclusionsGiven the clinical diversity of sarcoidosis, primary care physicians should be familiarized with its forms of presentation. This study suggests that in our medium where sarcoidosis is suspected in patients with joint symptoms, the absence of skin involvement decrease the likelihood of this diagnosis. This finding could be of use clinically and should be verified by other researchers.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Muñoz C, Restrepo-Escobar M, Martínez-Muñoz M, Echeverri A, Márquez J, Pinto LF. Diferencias entre los pacientes con sarcoidosis con y sin compromiso articular atendidos durante quince años en un hospital de tercer nivel de complejidad. Reumatol Clin. 2020;16:45–48.