To estimate the annual cost associated with obstetric events in women of reproductive age with immune-mediated inflammatory diseases, from the perspective of the National Healthcare System.
MethodsA cost-analysis was developed to estimate the impact associated with obstetric events in women of reproductive age with psoriasis (PSO), psoriatic arthritis (PsA), rheumatoid arthritis (RA) and axial spondyloarthritis (axSpA). The analysis considered complications during fertility and conception, in pregnancy and in the postpartum. All parameters were validated and agreed by a multidisciplinary expert panel. Unitary costs (€,2019) were obtained from national, local databases.
ResultsDuring fertility and conception, an annual cost per patient of €229 was estimated for a preconception consultation in a patient with PSO, of €3642 for a preconception consultation in patients with PsA, RA and axSpA and €4339 for assisted reproduction. Women with complications in pregnancy had an annual cost per patient of €1214 for a miscarriage in the first trimester, €4419 for a late miscarriage in the second trimester, €11,260 for preeclampsia €3188 for restricted intrauterine growth and €12,131 for threat of premature delivery. In the postpartum, an annual cost per patient of €120,364, €44,709, and €5507 were estimated associated with admissions to neonatology of premature infants of <28, 28−32 and 33−37 weeks, respectively.
ConclusionsThis analysis provides insight on the economic burden of complications associated with women of reproductive age for immune-mediated diseases (PSO, PsA, RA, axSpA). Individualization of treatment, additional and close monitoring may reduce the risk and burden of these complications.
Estimar el coste anual asociado a eventos obstétricos que pueden experimentar mujeres en edad fértil con enfermedades inflamatorias inmunomediadas, desde la perspectiva del Sistema Nacional de Salud.
MétodosSe desarrolló un análisis de costes para estimar el impacto anual por paciente asociado a eventos obstétricos en mujeres en edad reproductiva con artritis psoriásica (APs), artritis reumatoide (AR), espondiloartritis axial (EspAax) y psoriasis (PsO). Se consideraron eventos durante la fertilidad, la concepción, el embarazo y el posparto. Todos los parámetros fueron validados y consensuados por un panel multidisciplinar de expertos. Los costes unitarios (€,2019) se obtuvieron de bases de datos nacionales.
ResultadosDurante la fertilidad y concepción, se estimó un coste anual/paciente de 229€ para una consulta preconcepcional en pacientes con PsO, de 3.642€ en pacientes con APs, AR y EspAax y de 4.339€ para reproducción asistida. En el embarazo, el coste anual/paciente fue de 1.214€ para un aborto espontáneo en el 1er trimestre, 4.419€ para un aborto tardío en el 2º trimestre, 11.260€ para preeclampsia, 3.188€ para crecimiento intrauterino retardado y 12.131€ para amenaza de parto prematuro. En el postparto, se estimó un coste anual/paciente de 120.364€, 44.709€ y 5.507€ para prematuridad de <28, 28-32 y 33-37 semanas, respectivamente.
ConclusionesEste análisis facilita información sobre la carga económica de los eventos en mujeres en edad reproductiva con APs, AR, EspAax y PsO. Una adecuada planificación junto con la individualización del manejo, el tratamiento y la monitorización adicional pueden reducir el riesgo y la carga de estos eventos.
Immune-mediated inflammatory diseases (IMIDs) are a heterogeneous group of chronic diseases characterised by impairment of the immune system related to an imbalance of cytokines involved in the inflammation process, causing chronic damage to different organs and tissues.1,2
It is estimated that this group of diseases affects more than 2.5 million Spaniards, which represents a prevalence of 6.4%,3 with an overall higher prevalence in women (7.4%) than in men (5.4%).4 The most prevalent IMIDs include psoriatic arthritis (PsA), rheumatoid arthritis (RA), axial spondyloarthritis (axSpA) and psoriasis (PSO). It is estimated that 10%–20% of the population with these diseases are women of reproductive age (18–45 years).1,3,5
The initial therapeutic approach to the treatment of IMIDs is to control symptoms and inflammatory activity, and to prevent tissue damage. Currently, the target of the available therapeutic treatments is to achieve long-term complete remission or a state of low disease activity, thereby improving the patient's quality of life.2,6
Onset of these diseases may coincide with a woman's reproductive age; therefore, it is important to consider a potential pregnancy in the management of these diseases. Pregnancy can be a challenge for the healthcare professional and may be complicated with serious consequences and even death.7,8 These events primarily occur in women with active disease, with a higher risk of pre-eclampsia, caesarean section and preterm delivery than the general population.9–11 In this regard, adequate disease control is crucial to ensure the best foetal and maternal health as high disease activity is associated with an increased risk of adverse pregnancy outcomes and small-for-gestational-age foetuses.12–15
Therefore, pregnancy planning, the optimal treatment to achieve pre-pregnancy disease control and close follow-up of these patients are necessary to prevent or detect potential events early. It is also important to consider the management of women with IMIDs and their desire for pregnancy in multidisciplinary consultations, towards a more appropriate approach to both the disease and the pregnancy and, therefore, to the management of events.16 In recent years, specialist consultations for pregnancy management in women with IMIDs have been developed in some hospitals in Spain.
IMIDs are a significant economic and social burden for healthcare systems and patients.2,17 The annual cost of these diseases exceeded 12,000 million Euros in Spain, representing an average annual cost per patient of more than 3000€.18 In this context, to optimise available resources to ensure the sustainability of healthcare systems, economic evaluations are very important to obtain information on the cost of managing these patients.19
In the absence of economic data available in the literature, the aim of the present study is to estimate the cost associated with potential obstetric events in women of reproductive age with PSO, PsA, RA, axSpA, from the perspective of the National Health System (NHS) in Spain.
Material and methodsA cost analysis model was designed to estimate the economic impact associated with obstetric events in women of reproductive age with PsA, RA, axSpA, and PSO, in Spain, from the perspective of the Spanish national health system, within a time frame of one year. This analysis was developed in Microsoft Excel 2016, with input from a multidisciplinary panel of experts (rheumatology, dermatology, gynaecology/obstetrics, reproductive medicine, and neonatology), to validate and agree all the parameters included in the model.
The study population were women of reproductive age with IMIDs such as PsA, RA, axSpA, and PSO. These diseases were considered the most prevalent at national level and of the greatest social impact based on the data found in the literature.3,20
Events were evaluated in the women during fertility and conception (preconception consultation and assisted reproduction), during pregnancy (miscarriage in the 1 st trimester, late miscarriage in the 2nd trimester, preeclampsia, restricted intrauterine growth, and threat of premature delivery) and in the newborn in the postpartum (admission to the neonatal intensive care unit [NICU] due to prematurity of <28 weeks, 28−32 weeks, and 33−37 weeks). The data were obtained from publications reviewed in the literature.15,16,21–23
Health resources considered in the modelIn line with the perspective of the analysis, only direct health resources associated with the management of events in women of reproductive age with PsA, RA, axSpA, and PSO were considered in the model.
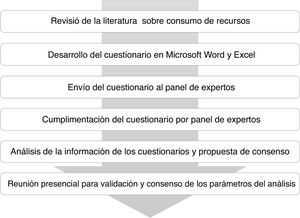
The multidisciplinary panel of experts identified and estimated the consumption of direct resources associated with the management of each obstetric complication according to the stage of the woman of reproductive age (during fertility and conception or in pregnancy) and of the newborn in the postpartum period. To this end, a structured questionnaire was developed in Microsoft Word and Excel and completed by the expert panel based on their experience in routine clinical practice. To facilitate completion of the questionnaire, the resources were grouped into the following categories: visits and consultations with physicians, hospital admissions (duration and hospital unit), surgeries performed (type and duration), procedures (laboratory and imaging), medications and other resources associated with the management of obstetric events considered in the analysis. A face-to-face meeting was then held with the members of the multidisciplinary expert panel to review and agree on the consumption of resources to be included in the analysis (Fig. 1).
Tables 1–3 detail the annual frequency as well as the percentage of patients estimated by the expert panel for each event in women of reproductive age with PsA, RA, axSpA, and PSO.
Healthcare resource consumption for the management of events during fertility and conception.
| Event | Preconception consultation | Assisted reproduction | |||||
|---|---|---|---|---|---|---|---|
| PSO | RA, PsA and axSpA | ||||||
| Description of resource | Resource used | Annual frequency | % of patients | Annual frequency | % of patients | Annual frequency | % of patients |
| Visits, consultations | Dermatology | 2 | 60% | – | – | – | – |
| 3 | 30% | ||||||
| 4 | 10% | ||||||
| Nursing | – | – | – | – | 5 | 25% | |
| Gynaecology/Obstetrics | – | – | 1 | 50% | 10 | 25% | |
| 3 | 25% | ||||||
| 2 | 50% | ||||||
| 5 | 50% | ||||||
| Rheumatology | 4 | 60% | 2 | 100% | |||
| – | – | 6 | 20% | ||||
| 3 | 20% | ||||||
| Hospital admissions | Day hospital | – | – | – | – | 1 day | 25% |
| 2 days | 25% | ||||||
| Rheumatology | – | – | 3 days | 1% | – | – | |
| Procedures | Laboratory tests | – | – | – | – | 8 | 25% |
| 1 | 50% | ||||||
| 4 | 25% | ||||||
| Complete autoimmunity | – | – | 1 | 70% | – | – | |
| Cervico-vaginal cytology | 1 | 30% | 1 | 40% | – | – | |
| Vaginal ultrasound | – | – | – | – | 1 | 20% | |
| 3 | 10% | ||||||
| 9 | 15% | ||||||
| 10 | 55% | ||||||
| High resolution ultrasound | – | – | – | – | 1 | 10% | |
| Diagnostic hysteroscopy | – | – | – | – | 1 | 10% | |
| Joint infiltration | – | – | 1 | 10% | – | – | |
| Artificial insemination | – | – | – | – | 2 | 30% | |
| Hip X-ray | – | – | 1 | 20% | – | – | |
| Chest X-ray | – | – | 1 | 20% | – | – | |
| Surgeries | Surgical hysteroscopy | – | – | – | – | 1 | 5% |
| Follicular puncture | – | – | – | – | 1 | 25% | |
| 2 | 25% | ||||||
| Embryo transfer | – | – | – | – | 2 | 50% | |
| Drugs | Folic acid | – | – | 5 mg/day, 6 months | 30% | – | – |
| 400 μg/day, 6 months | 70% | ||||||
| GnRH antagonists | – | – | – | – | .10 mg (single dose) | 50% | |
| .25 mg/day, 5 days | |||||||
| Contraceptives or oestrogens | – | – | – | – | 1 tab/day, 15 days | 25% | |
| Biological therapies | – | – | Induction and maintenance according to data sheet | 10%-30% | – | – | |
| Enoxaparin | – | – | – | – | 40IU/day, 30 days | 15% | |
| hCGr | – | – | – | – | 6500 IU (single dose) | 25% | |
| Hydroxychloroquine | – | – | 200 mg/12 h, 8 months | 20% | – | – | |
| Follicle stimulating hormones | – | – | – | – | 225IU/day, 10 days | 50% | |
| 50IU/day, 8 days | 30% | ||||||
| Potassium iodide | – | – | 200 μg/day, 6 months | 100% | – | – | |
| Naproxen | – | – | 500 mg/day, 2 months | 30% | – | – | |
| Ovitrel (HCG) | – | – | – | – | 6,500IU (sing dose) | 50% | |
| Prednisone | – | – | 5 mg/day, 4 months | 40% | – | – | |
| Progesterone | – | – | – | – | 200 mg/12 h, 30 days | 100% | |
| Sulfasalazine | – | – | 1 g/12 h, 6 months | 40% | – | – | |
| Other resources | General anaesthesia | – | – | – | – | 1 | 50% |
Healthcare resource consumption for the management of events in pregnancy.
| Event | Spontaneous miscarriage | Late miscarriage | Preeclampsia | Restricted intrauterine growth | Threatened premature delivery | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Description of resource | Resource used | Annual frequency | % patients | Annual frequency | % patients | Annual frequency | % patients | Annual frequency | % patients | Annual frequency | % patients |
| Visits, consultations | Gynaecology/obstetrics | 2 | 20% | 2 | 100% | 4 | 80% | 3 | 80% | – | – |
| 3 | 80% | 6 | 20% | 4 | 15% | – | – | ||||
| Haematology | – | – | 1 | 100% | – | – | – | – | – | – | |
| Rheumatology | – | – | 1 | 30% | – | – | – | – | – | – | |
| Hospital admissions | Gynaecology/obstetrics | – | – | 2 days | 100% | 4 days | 80% | 14 days | 5% | 3 days | 60% |
| 7 days | 20% | ||||||||||
| 35 days | 17% | 14 days | 10% | ||||||||
| 30 days | 10% | ||||||||||
| Day hospital | 1 day | 20% | – | – | – | – | – | – | – | – | |
| ICU | – | – | – | – | 5 days | 3% | – | – | – | – | |
| Procedures | Diagnostic amniocentesis | – | – | – | – | – | – | – | – | 1 | 5% |
| Laboratory tests | 1 | 100% | 2 | 100% | 2 | 80% | 1 | 80% | 2 | 100% | |
| 18 | 17% | ||||||||||
| 5 | 3% | 2 | 20% | ||||||||
| Vaginal ultrasound | 2 | 100% | 2 | 100% | 2 | 80% | 3 | 80% | 2 | 100% | |
| 4 | 15% | ||||||||||
| 12 | 20% | 14 | 5% | ||||||||
| High resolution ultrasound | – | – | 1 | 5% | – | – | – | – | – | – | |
| Chromosome studies | 1 | 5% | – | – | – | – | – | – | – | – | |
| Genetic study | – | – | 1 | 100% | – | – | – | – | |||
| Placenta study, autopsy | – | – | 1 | 100% | – | – | – | – | – | – | |
| Cardiac monitoring | – | – | – | – | – | – | – | – | 30 | 100% | |
| Surgeries | Caesarean | – | – | – | – | – | – | 1 | 40% | – | – |
| Dilatation and curettage | 1 | 20% | – | – | – | – | – | – | – | – | |
| Anatomopathological study | 1 | 20% | – | – | – | – | – | – | – | – | |
| Curettage | – | – | 1 | 50% | – | – | – | – | – | – | |
| Drugs | Methyldopa | – | – | – | – | 500 mg/8 h, 6 weeks | 20% | – | – | – | – |
| Betamethasone | – | – | – | – | 12 mg/day, 2 doses | 20% | 12 mg/day, 2 doses | 15% | 12 mg/day, 2 doses | 100% | |
| Doxycycline | – | – | 100 mg(single dose) | 50% | – | – | – | – | – | – | |
| 200 mg(single dose) | 50% | ||||||||||
| Labetalol | – | – | – | – | 100 mg/8 h, 6 weeks | 100% | – | – | – | – | |
| Misoprostol | 800 μg(single dose) | 60% | 800 μg(single dose) | 100% | – | – | – | – | – | – | |
| 800 μg, 2 doses | 20% | 400 μg/4 h, 1 day | 20% | ||||||||
| Prednisone | – | – | 10 mg/day, for 15 days | 30% | – | – | – | – | – | – | |
| Magnesium sulphate | – | – | – | – | 6 g (single dose) | 10% | 6 g (single dose) | 5% | 6 g (single dose) | 10% | |
| 1 g/4 h, 2 days | 1 g/4 h, 2 days | 1 g/4 h, 2 days | |||||||||
| Tractocile | – | – | – | – | – | – | – | – | 1 48 h cycle | 80% | |
| 2 48 h cycles | 10% | ||||||||||
| 4 48 h cycles | 10% | ||||||||||
| Other resources | General anaesthesia | 1 | 20% | 1 | 25% | – | – | – | – | – | – |
| Regional anaesthesia | – | – | 1 | 25% | – | – | – | – | – | – | |
| Vaginal-rectal discharge | – | – | – | – | 1 | 100% | – | – | – | – | |
| Induction of labour | – | – | – | – | 1 | 100% | – | – | – | – | |
| Cardiotocography recording | – | – | – | – | 2 | 80% | – | – | – | – | |
| 35 | 20% | – | – | – | – | ||||||
Healthcare resource consumption for the management of postpartum events.
| Event | Prematurity <28 weeks | Prematurity 28−32 weeks | Prematurity 33−37 weeks | ||||
|---|---|---|---|---|---|---|---|
| Resource description | Resource used | Annual frequency | % patients | Annual frequency | % patients | Annual frequency | % patients |
| Visits, consultations | Neonatology | 5 | 100% | 2 | 100% | 1 | 30% |
| Hospital admissions | Neonatology | 80 days | 50% | 20 days | 50% | 7 days | 60% |
| 60 days | 50% | 28 days | 30% | 14 days | 10% | ||
| 35 days | 20% | 20 days | 2% | ||||
| NICU | 30 days | 50% | 7 days | 50% | 5 days | 5% | |
| 15 days | 50% | 15 days | 30% | ||||
| 20 days | 20% | ||||||
| Procedures | Laboratory tests | 22 | 100% | 8 | 100% | 1 | 60% |
| 2 | 40% | ||||||
| Central line cannulation | 5 | 100% | 1 | 90% | 1 | 20% | |
| Hearing screening | 1 | 100% | 1 | 100% | – | – | |
| Echocardiography | 7 | 50% | 2 | 70% | 1 | 50% | |
| 5 | 30% | ||||||
| 3 | 20% | ||||||
| Abdominal ultrasound | 4 | 90% | 1 | 100% | 1 | 100% | |
| Brain ultrasound | 8 | 100% | 4 | 100% | 1 | 100% | |
| Fundoscopic examination | 2 | 60% | 2 | 80% | – | – | |
| 3 | 30% | ||||||
| 4 | 10% | ||||||
| Arterial/venous blood gases | 90 | 100% | 20 | 100% | 4 | 40% | |
| 3 | 30% | ||||||
| 2 | 30% | ||||||
| Chest/abdomen X-ray | 15 | 100% | 3 | 100% | 1 | 50% | |
| Intelligence test (Bayley) | 1 | 100% | 1 | 100% | – | – | |
| Mechanical ventilation | 1 | 50% | 1 | 20% | – | – | |
| Non-invasive ventilation | 1 | 90% | 1 | 60% | – | – | |
| Surgeries | PDA surgery | 1 | 15% | – | – | – | – |
| Surgery to treat NEC | 1 | 20% | – | – | – | – | |
| ROP surgery | 1 | 45% | – | – | – | – | |
| Intestinal perforation | 1 | 2% | – | – | – | – | |
| Drugs | Bevacizumab | .625 mg (single dose) | 40% | .625 mg (single dose) | 40% | – | – |
| Ranitidine | – | – | 2 mg/kg/8 h, 10 days | 50% | – | – | |
| Surfactant | 200 mg/kg (single dose) | 50% | – | – | – | – | |
| 100 mg/kg (single dose) | 25% | – | – | ||||
| Other resources | Parenteral nutrition | 20 days | 100% | – | – | – | – |
| Lumbar puncture | – | – | – | – | 1 | 5% | |
| Brain MRI | – | – | – | – | 1 | 5% | |
| Early-onset neonatal sepsis | 1 | 9% | – | – | – | – | |
| Late-onset neonatal sepsis | 1 | 50% | – | – | – | – | |
| Red blood cell transfusion | 2 | 40% | – | – | – | – | |
In line with the perspective of the analysis, only direct health care costs were considered. In this sense, the costs included in the total cost estimation were those associated with the management of obstetric events in women of childbearing age with IMIDs according to their stage (during fertility and conception, pregnancy and postpartum).
The pharmacological costs associated with the management of events were calculated based on laboratory sales price (LSP) obtained from the catalogue of medicines of the General Council of Pharmaceutical Associations of Spain,24 applying the deductions provided in Royal Decree-Law 8/201025 (Table 4).
Pharmacological costs associated with the management of events.
| PVL – RD 08/2010 | |
|---|---|
| Folic acid | .038€/mg |
| Methyldopa | .002€/mg |
| GnRH antagonists | .21€/mg |
| Betamethasone | .18€/mg |
| Bevacizumab | 3.05€/mg |
| Doxycycline | .003€/mg |
| Enoxaparin | .001€/IU |
| Oestrogens | .73€/tab |
| hCGR | .12€/μg |
| Hydroxychloroquine | .002€/mg |
| Recombinant follicle stimulating hormones | .195€/IU |
| Potassium iodide | .0002€/μg |
| Labetalol | .01€/mg |
| Misoprostol | .0007€/μg |
| Naproxen | .001€/mg |
| Prednisone | .0067€/mg |
| Progesterone | .0047€/mg |
| Ranitidine | .0018€/mg |
| Sulfasalazine | .0001€/mg |
| Magnesium sulphate | .005€/mg |
| Surfactant | 1.33€/mg |
| Biological therapies | 2.19−3.46€/mg |
| Tractocile | 170.00€/cycle |
In the case of medicines where the dose is calculated per kilogram of weight, average weight needs to be defined. For the analysis, an average weight of 750 g was established for preterm infants <28 weeks and 1200 g for preterm infants from 28 to 32 weeks, based on the data found in the literature.26
Unit costs for each of the resources were obtained from the national healthcare cost database27 and the literature.28 All costs were expressed in 2019 Euros (€, 2019).
Table 5 details the unit costs of the healthcare resources included in the analysis.
Unit costs (€, 2019).
| Item | Unit cost (€) | |
|---|---|---|
| Visits, consultations | Dermatology | 89.30 |
| Nursing | 31.76 | |
| Gynaecology/Obstetrics | 127.73 | |
| Haematology | 157.82 | |
| Neonatology | 87.12 | |
| Paediatrics | 174.16 | |
| Rheumatology | 153.36 | |
| Hospital admissions | Gynaecology/Obstetrics | 786.25 |
| Day hospital | 364.49 | |
| Neonatology | 725.05 | |
| Rheumatology | 945.13 | |
| Intensive care unit | 1.362.59 | |
| Neonatal intensive care unit | 1.868.24 | |
| Procedures | Diagnostic amniocentesis | 316.17 |
| Laboratory tests | 111.40 | |
| Full autoimmune | 149.61 | |
| Central line cannulation | 635.54 | |
| Cervico-vaginal cytology | 20.50 | |
| Hearing screening | 126.76 | |
| Echocardiography | 75.24 | |
| Abdominal ultrasound | 115.26 | |
| High resolution ultrasound, 3D | 56.13 | |
| Brain ultrasound | 83.53 | |
| Vaginal ultrasound | 102.48 | |
| Chromosome study | 260.79 | |
| Genetic study | 235.43 | |
| Placenta study, autopsy | 1.039.44 | |
| Fundoscopic examination | 39.00 | |
| Arterial/venous blood gases | 17.57 | |
| Diagnostic hysteroscopy | 317.18 | |
| Joint infiltration | 201.02 | |
| Artificial insemination | 1,224.38 | |
| Cardiac monitoring | 182.00 | |
| Hip/lumbar spine X-ray | 49.55 | |
| Chest X-ray | 127.12 | |
| Intelligence test (Bayley) | 555.00 | |
| Mechanical ventilation | 300.16 | |
| Non-invasive ventilation | 240.13 | |
| Surgeries | Caesarean | 4,339.59 |
| Patent ductus arteriosus surgery | 3,313.44 | |
| Dilatation and curettage | 1,453.34 | |
| Necrotizing enterocolitis | 28,883.98 | |
| Anatomopathological study | 111.76 | |
| Surgical hysteroscopy | 876.39 | |
| Curettage | 766.18 | |
| Perforated bowel | 13,613.31 | |
| Follicular puncture | 223.08 | |
| Retinopathy | 3,358.71 | |
| Embryo transfer | 120.92 | |
| Other resources | General anaesthesia | 704.49 |
| Regional anaesthesia | 478.87 | |
| Vaginal-rectal discharge | 150.00 | |
| Induction of labour | 799.39 | |
| Lumbar puncture | 243.37 | |
| Cardiotocography recording | 147.72 | |
| Brain MRI | 279.71 | |
| Early-onset neonatal sepsis | 6,866.85 | |
| Late-onset neonatal sepsis | 6,866.85 | |
| Red blood cell transfusion | 173.00 |
The total annual cost per patient for each event considered in the analysis was estimated from disaggregated information on resource consumption multiplied by the unit cost of each of the resources identified, validated, and agreed for the management of obstetric events in women of childbearing age with PsA, RA, axSpA, and PSO.
ResultsTaking into account the resource consumption estimated by the expert panel for each of the events, the total cost associated with the management of events in women of childbearing age with PsA, RA, axSpA, and PSO varies according to stage, ranging from 229€/patient in the case of preconception consultation in women with PSO to 120,364€/patient for admission to neonatology for a preterm infant <28 weeks.
During fertility and conception, the annual cost per patient was estimated for each potential event in women with PsA, RA, axSpA, and PSO. The annual cost per patient associated with the follow-up preconception consultation was 229€ (specialist visits 223€ and laboratory and imaging procedures 6€) and 3642€ (specialist visits 836€; hospital admissions 28€; laboratory and imaging procedures 168€; and medication 2610€) in a patient with PSO and in a patient with PsA, RA and axSpA, respectively. Assisted reproduction entailed an annual cost per patient of 4339€ derived from 1081€ for specialist visits, 273€ for hospital admissions, 1915€ for laboratory and imaging procedures, 332€ for surgical procedures, 386€ for medication and 352€ for other resources (Fig. 2).
Women with events in pregnancy presented an annual cost per patient of 1214€ for a 1 st trimester miscarriage (specialist visits 358€; hospital admissions 73€; laboratory and imaging procedures 329€; surgical procedures 313€; medication .60€ and other resources 141€), of 4419€ for a 2nd trimester late miscarriage (specialist visits 459€; hospital admissions 1573€; laboratory and imaging procedures 1705€; surgical procedures 383€; medication 3€; and other resources 296€), of 11,260€ for pre-eclampsia (specialist visits 562€; hospital admissions 7399€; laboratory and imaging procedures 946€; medication 133€; and other resources 2220€) of 3187€ for retarded or restricted intrauterine growth (specialist visits 383€; hospital admissions 550€; laboratory and imaging procedures 513€; surgical procedures 1736€; and medication 5€) and of 12,132€ for threatened premature delivery (hospital admissions 5976€; laboratory and imaging procedures 5904€; and medication 252€) (Fig. 2).
For postpartum events, an estimated annual cost per patient of 120,364€ was associated with neonatal admissions for preterm infants <28 weeks derived from 436€ for specialist visits, 92,789€ for hospital admissions, 11,767€ for laboratory and imaging procedures, 8058€ for surgeries, 126€ for medication and 7190€ for other resources. Admissions to neonatology from 28 to 32 weeks entailed an annual cost per patient of 44,709€ derived from 174€ for specialist visits, 40,835€ for hospital admissions, 3699€ for laboratory and imaging procedures and .83€ for medication. For neonatal admissions from 33-37 weeks the cost was 5507€ associated with 26€ for specialist visits, 4817€ for hospital admissions, 638€ for laboratory and imaging procedures; and 26€ for other resources (Fig. 2).
DiscussionIMIDs are chronic disabling diseases of major economic and social impact, resulting in impaired quality of life. In this regard, women of reproductive age with these diseases may present a significant risk of events around their pregnancy (fertility, conception, and pregnancy) and in the newborn in the postpartum period, leading to increased costs associated with the management of these events. Based on the literature reviewed, the most frequent events suffered by women and the newborn are miscarriage, pre-eclampsia, preterm birth, low birth weight or neonatal death.4,29–31 In addition, the decision to conceive often has great psychological impact for women with IMIDs, as they must balance the effectiveness of treatment for their underlying disease, the possible adverse events of this therapy and the potential risks during gestation and postpartum. Adequate disease control, without increasing the risk of foetal damage, through effective and compatible management and treatment, is therefore essential to ensure the health of both mother and foetus.7,23,32,33 The choice of optimal therapy before and during pregnancy should be made by assessing each patient individually to tailor the most appropriate therapy for the greatest efficiency. Thus, it is advisable to identify, quantify and assess the cost associated with events in women with IMIDs to allocate healthcare resources appropriately.
To the authors' knowledge, this is the first cost analysis in Spain from the perspective of the Spanish healthcare system to evaluate the cost of events in women of reproductive age with PsA, RA, axSpA and PSO. According to the results of this study, the events associated with women with PsA, RA, axSpA and PSO of reproductive age have high economic impact, and a higher cost is estimated for postpartum events (5,507−120,364€/patient) compared to the other stages considered in the analysis (events during fertility and conception [229−4,339€/patient] and in pregnancy [1,214−12,122€/patient]).
The present analysis is not without limitations, which should be considered when interpreting the results. These include the inherent theoretical nature of health economic evaluation models, which must address the uncertainty associated with routine clinical practice. Thus, the parameters used in the model are drawn from different sources; however, all the variables are based on official information or publications with a high level of clinical evidence and were validated by the multidisciplinary panel of experts. In addition, due to the paucity of information found in the literature on potential events in women of reproductive age with IMIDs or in the newborn, the resource consumption of these events was provided by the expert panel based on their clinical experience. However, expert opinion was used to make economic estimates in the absence of data in the literature.
The analysis was undertaken from the perspective of the Spanish national health system and therefore the cost of the events estimated in this analysis would be underestimated, as only direct healthcare costs were considered. However, this group of diseases is associated with a high cost for the social services and for the patients themselves, as a consequence of disability due to progression of the disease. In this sense, studies are necessary that provide additional information on direct non-health costs and indirect costs due to absenteeism from work and loss of productivity, as these costs represent a significant percentage of the total cost.18,34,35
Finally, the most prevalent IMIDs at the national level were considered for the analysis. These data were validated by the panel of experts and although they could be extrapolated to the other diseases that form part of this group of diseases because they share similar pathogenic mechanisms, it should be borne in mind that IMIDs comprise a highly heterogeneous group of diseases that can be associated with very different medical care.36 Despite the limitations described above, the present analysis provides preliminary insight into the cost associated with events experienced by women of reproductive age with IMIDs in Spain.
In conclusion, the results obtained suggest a high impact associated with events in women of reproductive age with IMID. These results could be useful in the healthcare decision-making process for the management of these patients, enabling the currently available healthcare resources to be efficiently allocated.
FundingThis project was funded by UCB Pharma S.A. The publication is independent of UCB Pharma S.A.
Conflict of interestsOnica Armijo, María Castellanos, Natalia Marin Huarte, Julia Martínez-Barrio, Nuria Martínez and Olga Villar received honoraria for participation in this work. Miguel Ángel Casado and María Mareque are employees of PORIB, who received consultancy fees for undertaking this work.
Please cite this article as: Martínez N, Villar O, Armijo O, Castellanos M, Marin Huarte N, Mareque M, et al. Impacto económico asociado a eventos obstétricos en mujeres en edad fértil con artritis psoriásica, artritis reumatoide, espondiloartritis axial y psoriasis en España. Reumatol Clin. 2022;18:105–113.