The incidence of depression accompanying medical pathologies is elevated and has prognostic importance.
ObjectivesTo determine the frequency of depression in patients with systemic autoimmune diseases (SAD), as well as to determine the frequency of pain, fatigue and sleep disorders in these patients and their relation with depression.
Material and methodsWe performed a descriptive, prospective study on 88 patients with AID. The CES-D depression questionnaire, FSS fatigue questionnaire and the Pittsburgh sleep quality index were administered.
Results69% (n=61) of patients were depressed. Pain was found in 97% (59/61) of depressed patients and in 62% (17/27) of non-depressed patients (P=.0006). Sleep disorders were found in 95% of depressed patients, whereas 60% of non-depressed patients presented them (P=.00008). Depression was associated with fatigue: 80% (49/61) for depressed and 44% for non-depressed (P=.001) persons.
DiscussionA very elevated prevalence of depression was found in SAD: 69%; constituting the most frequent comorbidity. Depression was significantly associated with pain, fatigue and sleep disorders.
La incidencia de trastornos depresivos acompañando a patologías médicas es elevada y tienen importancia pronostica en su evolución.
ObjetivoDeterminar la frecuencia de depresión en pacientes con enfermedades autoinmunitarias sistémicas (EAS) y su relación con el dolor, fatiga, trastornos del sueño.
Material y métodosSe realizó un estudio prospectivo descriptivo en 88 pacientes con EAS. Se aplicó cuestionario de depresión CES-D, cuestionario de fatiga FSS y calidad del sueño de Pittsburgh.
ResultadosEl 69% (n=61) de los pacientes se encontraba deprimido. El dolor se halló en 97% (59/61) de los pacientes deprimidos y en el 62% (17/27) de los no deprimidos (p=0,0006), trastornos del sueño en 95% (58/61) de los pacientes deprimidos, y en el 60% (15/27) de los no deprimidos (p=0,00008). La depresión se asoció a la fatiga: 80% (49/61) para deprimidos y 44% (12/27) para no deprimidos (p=0,001).
DiscusiónLa prevalencia de depresión en las EAS hallada fue muy elevada, 69%, siendo la comorbilidad más frecuente. La depresión se asoció significativamente al dolor, la fatiga y los trastornos del sueño.
The incidence of depressive disorders associated with medical conditions is high. Establishing a bidirectional relationship between them, each one has a negative impact on the prognosis of the other.
In 1929, Gillespie distinguished between endogenous depressive disorders (related to a disease) and psychogenic affective disorders. In 1970, depression associated with medical illness was called “reactive” or “secondary”, considering that its course was less severe than the “primary”.
Currently, depression with medical comorbidity is not considered a different diagnostic entity, but a part of the ongoing symptoms of depressive disorders. The medical condition is a risk factor for depression. It can act as a “stressor”, triggering or exacerbating depression in an otherwise predisposed patient.
Numerous studies have assessed the negative impact of depression on the progression of medical illness. It occurs in 27% of patients after a myocardial infarction (AMI). The risk of death at 6 months after the AMI quadruples in depressed patients compared to non-depressed. Similar results were reported in depression associated with other diseases.1 Therefore, depression that accompanies medical pathology can be considered an element of poor prognosis, determining increased morbidity and mortality.
Treating depression in patients with medical comorbidity is less effective, the response is slower and requires higher doses of antidepressive drugs.1
Systemic autoimmune diseases (SAD) are no exception to the above. The incidence of depression in rheumatoid arthritis (RA) is, according to some studies, 64%. Depression is associated with a doubling of premature mortality in these patients.
Cardinal symptoms of these diseases, such as fatigue, chronic pain, and changes in physical appearance, affect the psychic sphere and can act as triggers of depression (stressors).2,3 Depression, in turn, changes the perception of pain and is linked to fatigue and changes the perception of body changes.4 Both pain and depression lead to another disorder of great importance, sleep disorders.5
The SAD have the distinction of per se causing nervous system damage.6–8 Neuropsychiatric disorders are cited mainly in lupus, Sjogren's syndrome, vasculitis, and antiphospholipid syndrome. Their frequency and pathophysiology are controversial. The most common psychiatric manifestations are depression, mania, hallucinations, and psychosis.9
ObjectivesTo determine the frequency of depression in patients with SAD.
To describe the frequency and characteristics of pain, fatigue and sleep disorders in patients with SAD and their relation to depressive disorders.
Patients and MethodsWe conducted a descriptive study, which included all patients with SAD who attended the rheumatology clinic of the Hospital Maciel in the 4 months after the start of the study and gave their written informed consent to participate in the study. The study was approved by the ethics committee of the Hospital.
Data collected were surnames, marital status, workplace, immune-mediated pathology, duration, and comorbidities. Questionnaire applied were CES-D depression (Center for Epidemiologic Studies Depression Scale), fatigue questionnaire FSS (Fatigue Scale Severity), and the determination of the Pittsburgh Sleep Quality. Patients were asked to evaluate their pain in the last 2 weeks on a graded visual analogue scale, which was measured in millimeters. They were questioned about their appearance, compliance to treatment, consultation with a psychiatrist, and past treatment with antidepressant medication.
Wes considered a diagnosis of depression when the CES-D score >16,10 which has a sensitivity and specificity greater than 80%. The FSS fatigue questionnaire assesses a total score of 36 or more as an indicator of suffering from fatigue. The Pittsburgh sleep quality questionnaire classifies patients into good sleepers if they have a score <5 and poor sleepers if they have a score greater than or equal to 5.
For statistical analysis we used Student's t test and χ2, as appropriate, to assess differences between depressed and non-depressed patients. A statistically significant value was considered when P<.05.
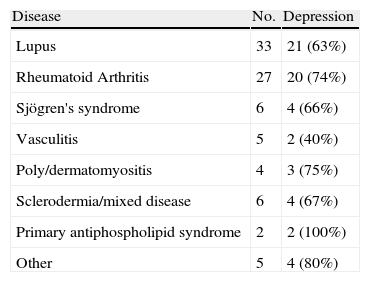
ResultsWe evaluated 88 patients with SAD. 90% (n=80) were women aged between 16 and 76 years, mean age 46.19±12.6 years. According to the CES-D questionnaire, 69.32% (n=61) of patients were depressed, thus being the most frequent comorbidity. The distribution according to conditions is shown in Table 1. Hypertension was associated in 29%, alterations in thyroid function in 23%, asthma in 15%, 11% had dyslipidemia, and diabetes in 9% of patients.
Distribution of Patients According to Disease and Association to Depression.
| Disease | No. | Depression |
| Lupus | 33 | 21 (63%) |
| Rheumatoid Arthritis | 27 | 20 (74%) |
| Sjögren's syndrome | 6 | 4 (66%) |
| Vasculitis | 5 | 2 (40%) |
| Poly/dermatomyositis | 4 | 3 (75%) |
| Sclerodermia/mixed disease | 6 | 4 (67%) |
| Primary antiphospholipid syndrome | 2 | 2 (100%) |
| Other | 5 | 4 (80%) |
Pain as a symptom was found in 86% (n=76) of patients, of whom 59 were depressed (59/61=80%) and 17 belonged to the non-depressed group (17/27=63%). We found statistical significance (SS) between pain and depression (P=.00008). Patients with pain had a SS tendency to score their pain higher: mean 25.6±64.7mm between depressed and 43.3±24.9mm and non-depressed (P=.0025). Among depressed patients, 95% (58/61) were bad sleepers, while non-depressed were 60% (15/27), which was also a significant difference (P=.00008). Depression was also significantly associated with fatigue: 80% (49/61) in depressed patients and 44% (12/27) for non-depressed (P=.0012). Perception of physical appearance was significantly different between depressed: 31% (19/61) and non-depressed: 59% (16/27), P=.0182. Depressed patients also fully or partially complied less with treatment (62% [38/61]) than non-depressed who showed a compliance of 89% (24/27), P=.0211.There were no differences between depressed and non-depressed patients in terms of age and time since onset of illness and marital status.
Thirty-six patients had sometime consulted with a psychiatrist, 35 patients in the depressed group (35/61=57%) and 21 (34%) received antidepressants. Among non-depressed subjects taking antidepressants 2 received antidepressants.
Discussion and ConclusionsThe frequency of depression found in SAD was surprisingly high: 69%, according to the CES-D questionnaire of depression, the most frequent comorbidity. The estimated rate of depression in our population is 4%–6%.11
Depression was found significantly related to pain, fatigue, sleep disorders, and dissatisfaction with physical appearance.12,13 Pain is an individual experience determined by many more factors than just the disease process, and subject to many variables and fluctuations. Pain and depression are linked in complex ways. Pain generates depression and depression causes pain. Both cause sleep disorders and fatigue.
Fatigue is a prominent and disabling symptom in patients with SAD. It is linked to disease progression in lupus. Some studies report that it affects 80% of patients. However, in most of them the cause of fatigue is unclear and the correlation with disease activity is weak and probably due to several factors: disease activity, mood disorders, sleep disorders, low physical activity, association with fibromyalgia, pain, medication effect, and depression.14
The association with fibromyalgia was not assessed in this study, which may have been important due to its link with some symptoms analyzed, but in no case constituted the patient's primary diagnosis.
Pain, fatigue, sleep disturbances, and depression impair quality of life, and affect family, work, and doctor–patient relationship. The link between them is complex. Other consequences have been recognized: Depression is associated with an increase in premature mortality of patients, and in the case of RA is duplicated.3
While the importance of detecting and treating depression early seems clear, it is not. Just over half of the patients identified as depressed (57%) had consulted a psychiatrist once, and 34% received antidepressant treatment. Only 2 patients in the non-depressed group were receiving antidepressant treatment. This finding is also a fact that is already known: the evolution of depression and response to treatment is less effective in patients with a medical illness than in those with depressive disorder alone. The response is slower and requires higher doses of antidepressives.1,15
The diagnosis of clinical depression is made with the implementation of the diagnostic criteria of the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders-IV, of the American Psychiatric Association. This is the gold standard for diagnosis of affective disorders and was equated with a broader classification system of diseases, the Tenth International Classification of Diseases.
However, there are tests evidence that allows for diagnostic screening with good sensitivity and specificity. These are useful for the first level of care in diagnosing and assessing treatment effectiveness. Despite the easy access to this resource (they can be used before entering the consultation), there has been resistance by physicians in their application.
A combination of factors hinder the recognition, evaluation, and treatment of depression in patients with SAD; however, their surprising frequency makes a comprehensive approach to our patients necessary, without which they miss out enormous therapeutic tools that meet their needs.
Conflict of InterestThe authors have no conflict of interest.
Please cite this article as: Arias S, et al. Enfermedades autoinmunitarias sistémicas y trastornos depresivos. Reumatol Clin. 2011;7(6):389–91.