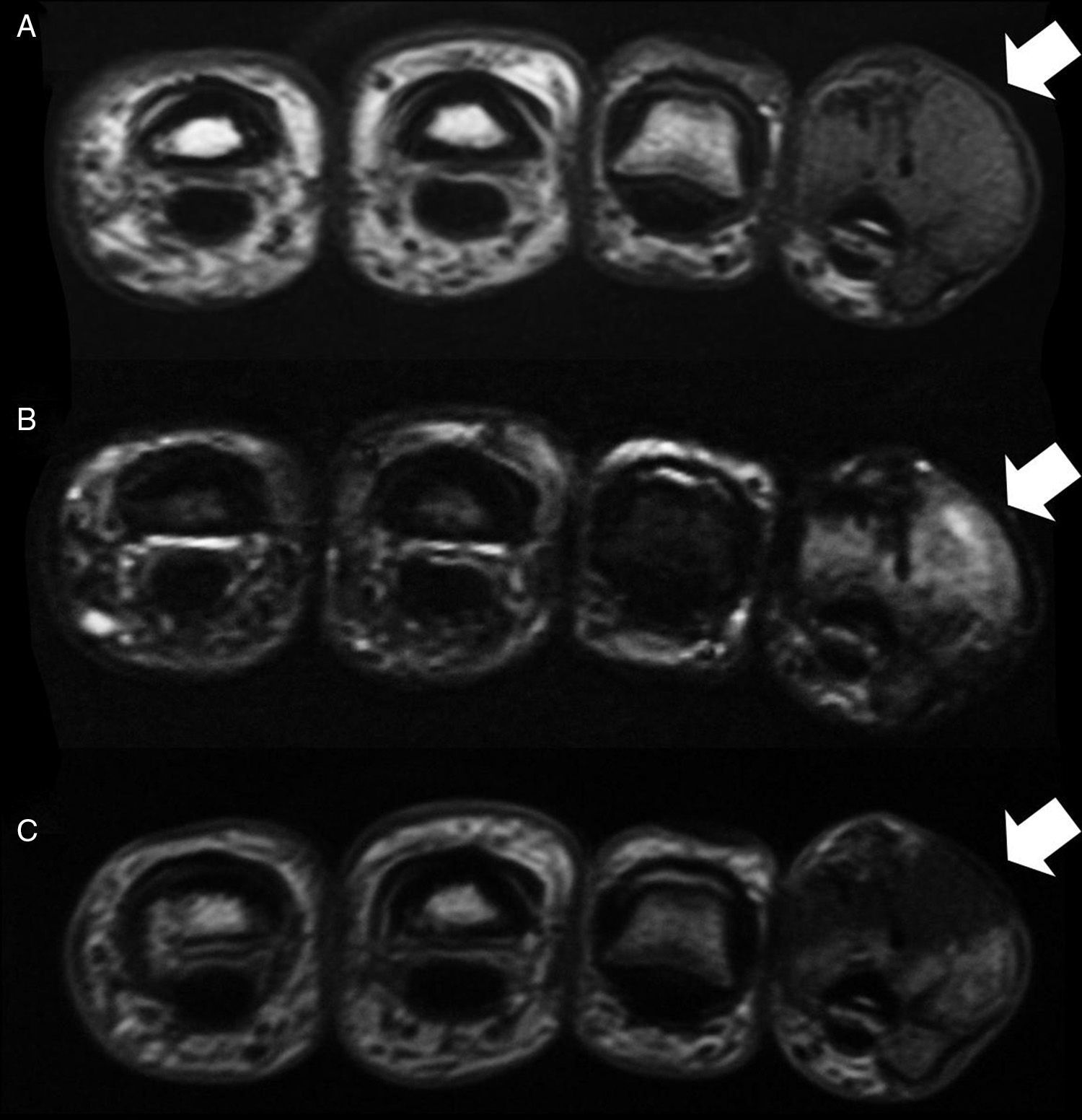
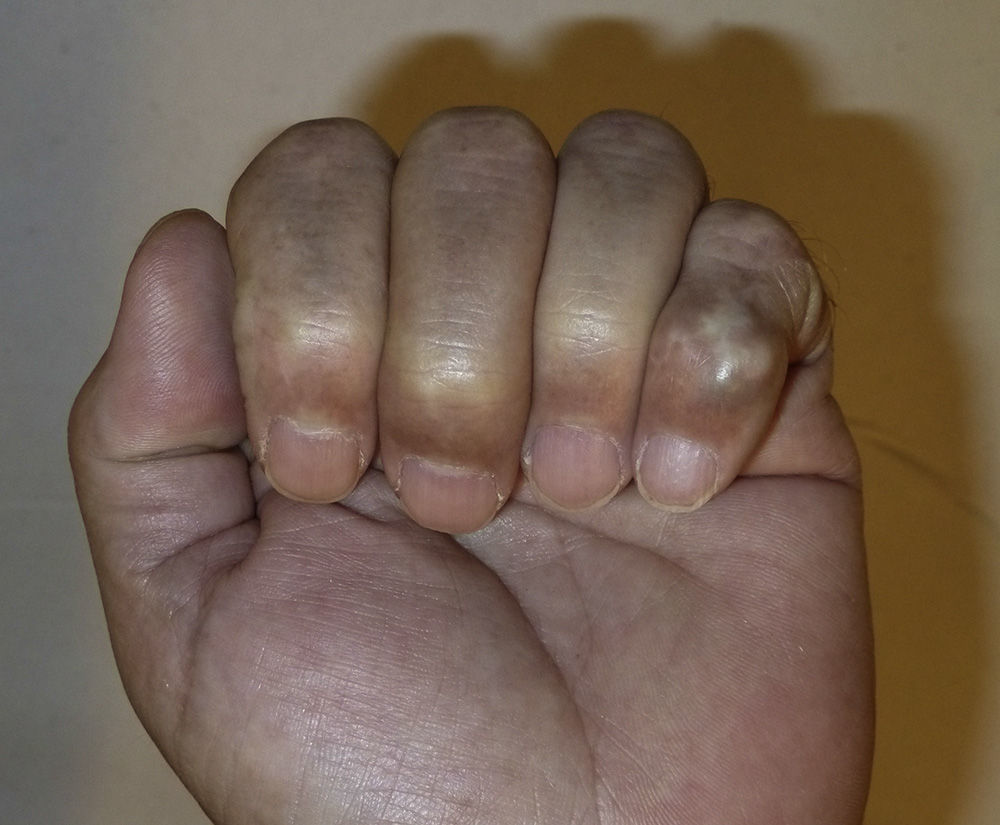
The case was a male patient, 65 years old, with no relevant medical history, who was consulted due to painless swelling on the dorsal side of the fifth finger of the left hand which had lasted for 4 years, with no history of trauma. Physical examination confirmed the tumor, elastic on palpation, with preserved finger mobility (Fig. 1) Simple X-rays showed a soft tissue tumor (Fig. 2); the ultrasound demonstrated the same lesion and the MRI showed a lesion measuring 16×10×12mm in diameter craneo-caudally, anteroposterior and transversely, unhomogeneous, with a hypointense signal and loculations on T1, predominantly hyperintense on T2 and showing moderate contrast enhancement (Fig. 3).
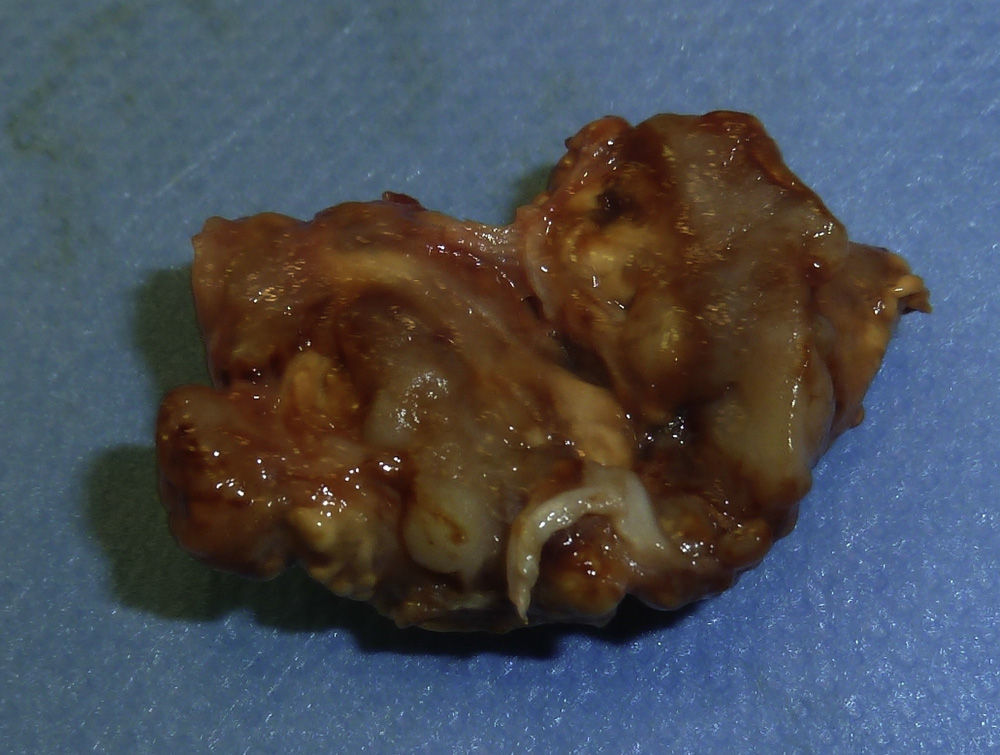
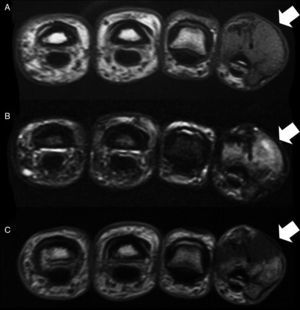
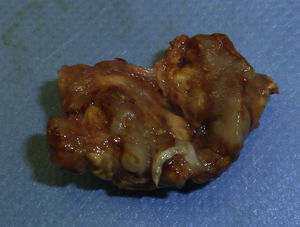
The lesion was diagnosed to be a giant cell tumor of the tendon sheath of the fifth finger and was removed in its entirety (Fig. 4). Two years later the lesion recurred (Fig. 5) and the patient underwent surgery. Currently, after two years, there have been no new recurrences, the mobility of the distal interphalangeal joint is limited, although the function of the patient's hand is normal.
The TSGCT of unknown etiology, excluding ganglia, represent almost half of the soft tissue tumors of the hand.1 It is common to find nodular forms and they occur in patients 30–50 years of age, although with a wide age range, being often female (in 55%–70% of cases). They are usually found on the volar side, the laterovolar side or the fingers, especially in the vicinity of the distal interphalangeal joint, without preference for a particular finger.1–6 Regarding laterality, the lesion is more common on the right and the dominant hand.4,6
The suspected diagnosis of TSGCT of the hand is made clinically and through complementary imaging tests, including simple radiographs and ultrasound, which are usually sufficient, and no biopsy is needed. Clinically, it is suspected when documenting a solitary soft tissue nodule that respects the skin, is often eccentric, painless and slow-growing.1 1%–24% of patients report some pain,3,4,6 usually in conjunction with increased volume and, sometimes, neurovascular compromise. The clinical differential diagnosis is extensive. Ultrasound identifies a generally homogeneous, hypo- or hyperechoic solid lesion or, rarely, a heterogeneous one, with increased vascularity on Doppler study, and in relation to the tendon sheath, with which it does not move for that reason.6–8 It is also common to find satellite lesions, and although this lesion could be confused with a ruptured synovial cysts, confusion has no therapeutic significance if intervened upon. Among complementary imaging, MRI is considered by some to be the most accurate imaging test for diagnosis.4,7,8
Treatment of TSGCT is based on the complete removal of the lesion. The technique seems more reliable using a large exposition and using magnifying glasses or microsurgical tools.6,9 Radiation therapy, although controversial, could be indicated in cases with higher risk of recurrence (lesions with mitosis, bone involvement or incomplete resection). This occurs in up to 45% of treated cases.
The authors declare that they have read and approved the manuscript and that the requirements for authorship have been met.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of InterestNone.
Please cite this article as: Ramos-Pascua LR, Guerra-Álvarez OA, Casas-Ramos P, Arias-Martín F. Tumor de células gigantes de las vainas tendinosas de los dedos de la mano. Reumatol Clin. 2015;11:252–254.