Granulomatosis with polyangiitis (GPA) is an autoimmune vasculitis which rarely affects the lower genitourinary tract. We share the case of a 53-year-old man who presented with a retroperitoneal mass and thereafter developed a left multiseptated hydrocele that conditioned a testicular infarction. The pathology report of the orchidectomy was consistent with GPA.
La granulomatosis con poliangeítis (GPA) es una vasculitis autoinmune que raramente afecta al tracto genitourinario inferior. Presentamos el caso de un varón de 53 años que debutó con una masa retroperitoneal y posteriormente desarrolló un hidrocele multiseptado izquierdo que condicionó un infarto testicular. El informe anatomopatológico de la orquiectomía reveló hallazgos sugestivos de GPA.
Granulomatosis with polyangiitis (GPA) is a necrotising granulomatous vasculitis of unknown aetiology that predominantly affects the respiratory tract and kidneys. Other genitourinary tract manifestations are considered exceptional and have been described as isolated cases or case series.1–5
Clinical observationA 53-year-old man with a history of right hemicolectomy for Crohn's disease was admitted with general malaise, scrotal and lower extremity oedema. Blood tests showed normal values except haemoglobin 12.1 g/dL and C-reactive protein 5.99 mg/dL. An NT-proBNP value of 139 pg/mL helped rule out heart failure. Basic urine test was normal. CT scan revealed a large retroperitoneal mass, suggestive of retroperitoneal fibrosis. Treatment was started with methylprednisolone 250 mg for three days, with improvement in symptoms.
Two months later, the patient began to experience intense and intermittent daily pain and swelling in the left hemiscrotum. Physical examination showed an enlarged and painful left hemiscrotum with no palpable masses. Ultrasonography confirmed left epididymitis and a large multiseptated left hydrocele, exerting a mass effect on the testicle, with compromised vascular flow, suggestive of testicular torsion. Emergency surgical exploration via the inguinal route was performed, finding a destructured testis with necrotic areas, resulting in a left orchidectomy.
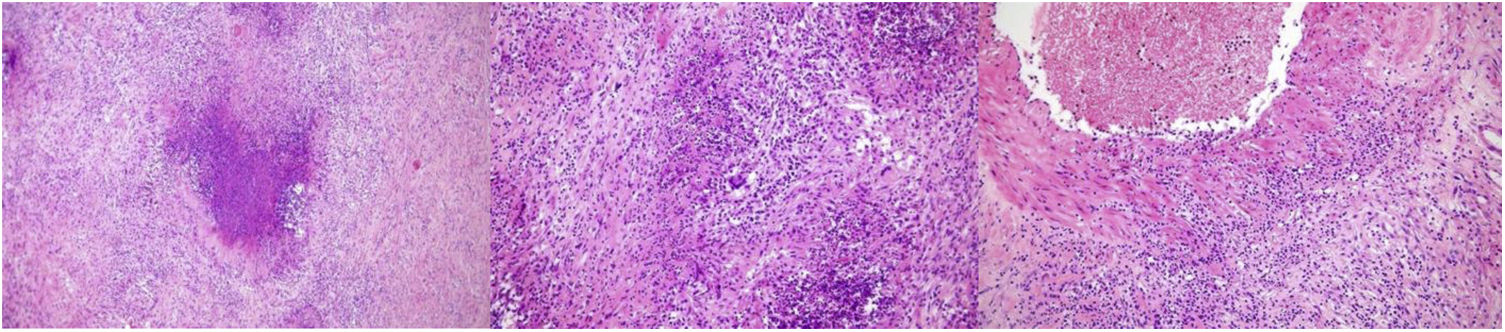
The pathology report described acute necrotising orchiepididymitis with granulomatous reaction (suppurative granulomas) and marked transmural inflammatory infiltrate in the vascular wall (Fig. 1), suggestive of granulomatosis with polyangiitis. The autoimmunity study confirmed positivity for cytoplasmic anti-cytoplasmic neutrophil antibodies (c-ANCA), directed against proteinase 3 (PR3-ANCA) at a titre of 31, detected by ELISA (positive: >25 UA/mL). Mycobacteria were ruled out by microbiological studies, sputum smear microscopy, polymerase chain reaction, and interferon. Serology was negative for hepatitis B and C virus, human immunodeficiency virus (HIV), and syphilis. One month later, the patient developed polyarthralgias and subsequently developed sensorimotor mononeuritis multiplex, diagnosed as a result of paraesthesias, dysesthesias, and neuropathic pain in both lower extremities, limiting ambulation.
After histological confirmation compatible with GPA (total seven points according to the ACR/EULAR 2022 classification), treatment was started with prednisone 30 mg daily and cyclophosphamide 1 g every two weeks, continuing every three weeks thereafter until a total of five boluses were given. The patient responded favourably with clinical remission under immunosuppressive treatment.
However, six months later, he presented with episcleritis in the right eye diagnosed as a result of photophobia, which was treated topically with dexamethasone eye drops 1 mg/mL, this dose was insufficient and therefore he received prednisolone acetate eye drops 10 mg/mL, combined with oral prednisone at initial doses of 60 mg/day for one week and then continuing at a dose of 30 mg/day, and rituximab i.v. 1 g was started with an initial dose and another after 14 days, with a favourable clinical response.
DiscussionGPA is an autoimmune disease affecting small and medium-sized vessels characterised by inflammation and granuloma formation. Lower genitourinary tract involvement is estimated in less than 1% of patients,6 prostatitis being the most common finding.2
Regarding testicular involvement, polyarteritis nodosa (PAN) is the most common cause of necrotising vasculitis of the testis, often associated with positive serology for hepatitis B surface antigen (HBsAg) and HIV. In ANCA-associated vasculitis, however, testicular involvement is infrequent, and may be encouraged by drug use (hydralazine, propylthiouracil, minocycline), leading to segmental testicular infarction.7
In our case, we presented an acute scrotum as the initial manifestation of systemic GPA, which required urgent orchidectomy due to suspected vascular involvement. In this context, surgical exploration is essential. In the absence of vascular involvement, however, testicular biopsy is considered the choice for diagnosis.3 PR3-ANCA antibodies are useful in diagnosis, as they are associated with GPA in 80%–90% of cases8; tumour markers, however, are usually negative.6
Although there is little data on the association with systemic disease, Brimo et al.9 describe in their series that only 25% of patients with localised testicular infarction showed symptoms of systemic vasculitis, stating that this association is more common in granulomatous vasculitis than in PAN (50% vs. 14%). Our patient started arthralgias after orchidectomy and was diagnosed with mononeuritis multiplex (initial Birmingham Vasculitis Activity Score [BVAS] v3: 12 points). Despite clinical remission with immunosuppressive treatment, he was diagnosed with episcleritis six months after the start of treatment (BVAS v3: 2).
In terms of therapeutic approach, surgical treatment (simple orchidectomy) is considered curative in most cases, because about 80% of cases are unilateral.10 The need for adjunctive immunosuppressive therapy is controversial in the limited form because the risk of progression to systemic disease is unknown. Some authors argue that if the patient remains asymptomatic after orchidectomy and biochemical findings are normal, a watchful waiting strategy could be adopted to avoid toxicity and the risk of sterility associated with it.9 In any case, although limited disease seems to entail better prognosis, a follow-up of at least six months is essential to ensure absence of progression.9
ConclusionsTesticular involvement is exceptional in GPA and may present as an acute scrotum. Surgical exploration is necessary in case of suspected vascular involvement, and surgical treatment is curative in most of the limited forms.
FundingNo funding was received for this work from public or private sources.
Conflict of interestsThe authors have no conflict of interests to declare.