Rheumatic diseases (RDs) are among the most common chronic health problems of the Catalan adult population. They cause important problems for individuals, their families and for the society overall, with high direct and indirect economic costs. The Department of Health of Catalonia promoted the creation of a Master Plan for the rheumatic diseases, as a tool for planning an integral approach to these problems.
ObjectiveTo present the work methodology that has been used in the development of the Master Plan and its final proposals.
MethodsFirst an analysis of the burden caused by these problems in our community was performed and the objectives of the Plan were established. Later, strategic lines were defined and work groups organized to analyze proposals for improvement, which after consensus were accepted.
ResultsThe proposals of the Plan comprise actions in the scope of prevention, rationalization in the use of resources and the formation of professionals among others. Changes in the health care model for RDs were proposed in order to improve specialized and primary care coordination with clinics and musculoskeletal functional units.
ConclusionsThe Master Plan recommends actions to improve the attention of the population through operative planning and the services to different providers. The Master Plan will establish the health policy action lines directed against these disorders.
Las enfermedades reumáticas son el problema de salud crónico más prevalente de la población adulta catalana. Conllevan importantes problemas para el individuo y para la sociedad, con elevados costes económicos directos e indirectos. Desde el Departamento de Salud de Cataluña se propuso la creación del Plan director de las enfermedades reumáticas y del aparato locomotor, como herramienta de planificación para abordar de forma integral estos problemas.
ObjetivoPresentar la metodología de trabajo que se ha utilizado para el desarrollo del Plan y las propuestas finales de este.
MétodosInicialmente se realizó un análisis de situación de estos problemas en nuestra comunidad y se establecieron los objetivos del Plan. Posteriormente, se definieron las líneas estratégicas y se organizaron grupos de trabajo para analizar las diferentes propuestas de mejora que fueron consensuadas con los actores implicados.
ResultadosLas propuestas del Plan incluyen aspectos que van desde la prevención a la rehabilitación con el objetivo de racionalizar el uso de los recursos y aumentar la eficiencia en la atención. Se propone un nuevo modelo asistencial que acerca la asistencia especializada a la atención primaria en forma de consultorías y la organización de unidades funcionales de aparato locomotor, entre otras propuestas.
ConclusionesEl Plan director establece las líneas de actuación de la política sanitaria y de la planificación en relación con estos trastornos a partir del análisis de la situación, el establecimiento de objetivos de mejora de la atención y la propuesta de acciones concretas para conseguirlos.
Rheumatic diseases are a prevalent health problem. According to the 2006 Catalan Health Survey (ESCA2006), dorsal and lumbar pain, neck pain and more rheumatoid arthritis, among other types of arthritis are the three chronic health problems most frequently reported by our population.1 The prevalence of these problems is higher in women and increases with age and low socioeconomic status.1 The impact of these diseases can be enormous for the individual who presents them, as well as for her/his family and society in general, both socially and economically. These disorders are one of the main reasons for work disability and the leading cause of lost work days,3 while in the elderly often they often involve dependence on others. The cost to health systems is between 1% and 1.5% of European countries gross national income.4 In Catalonia, the activity related to these processes occupies 32% of the time of primary care physicians (PC), generates a large volume of activity in rheumatology, orthopedic surgery and traumatology (TOC), and is the main consultation reason in pain units and rehabilitation5 services. Attention to these disorders is characterized by high fragmentation of care with inadequate flow of patients between different specialties and levels of care, duplication of visits, additional examinations and dissatisfaction of patients and professionals.
In order to improve the care of rheumatic diseases, the Department of Health launched in 2008 the Master Plan for rheumatic and musculoskeletal diseases (MP), in line with previous6 master plans, constituting the planning tool to comprehensively address these problems. The aim of this paper is to describe the methodology that was used and the final proposals that have been finally approved. The prioritization criteria of health problems to be addressed have resulted from population prevalence and impact on health services studies rather than specialty clinics. In this sense, some rheumatic processes with significant impact on affected individuals have a low prevalence population and have not been specifically addressed in this MP. The description of the operational lines of the MP and subsequent evaluation are not the subject of this article.
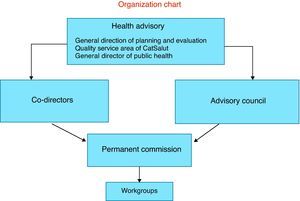
MethodsThe structure of the MP (Fig. 1) is organized according to the Directorate for Planning and Evaluation, Department of Health, in coordination with the Directorate General of Public Health and the CatSalut Management Services Quality Area. Two rheumatologists (ML and XS) joined the Directorate General to direct it and who were responsible for promoting, directing and coordinating the process of developing the MP. It was an Advisory Board with two chairs, a specialist in TOS and a rheumatologist, and 70 members linked to the field of rheumatic diseases from universities, health centers, scientific societies, professional associations, patient associations, suppliers and representatives of Public Administration. There was also a standing committee with 18 members of the advisory council, chosen for their expertise in musculoskeletal diseases and who eventually formed working groups, coordinated by an orthopedic surgeon (JA). Together with them worked 114 professionals in the groups and the final proposals were endorsed by patients, professionals, planners and managers.
The work was carried out in phases (Table 1), the first of which an analysis of the overall situation of rheumatic diseases in Catalonia. For the analysis of morbidity were used ESCA20061 data, which also allowed evaluation of the impact of these diseases in the quality of life, restriction of activities and use of health services.2 Hospital activity data was analyzed by recording hospitalization and social health (MDS-AH and SS), while the impact on work disability was obtained from the Catalan Institute of Medical Assessments records.3 Data were also obtained of the medications and joint replacement registry of Catalonia (official registry established to collect information on patients undergoing arthroplasty).7 Simultaneously, we conducted a literature search to compare the epidemiological and health services use in Catalonia with those published in other environments. From the initiative of the MP two studies were derived: a study on the current delay in surgery of osteoporotic hip fracture through the Catalan Society of TOS and an opinion survey among primary care physicians and related specialties with the musculoskeletal system (TOS, rheumatology, rehabilitation and medical pain units), to obtain qualitative information on aspects of care organization, relationship between levels of care and some improvement proposals.5
The outcome of this analysis derived from the MP targets was chosen and the strategies were prioritized based on the following criteria: magnitude of the problem, social importance (impact on activity and work disability, processes that cause dependence) and impact on the use of health services. The problems identified related to the management of health services led a strategic change in a specific health care model.
In a second phase, we developed the working groups, in the case of clinical trials, made by experts in the specific issue in question and both PC and medical specialties as mentioned above and others (geriatrics, pediatrics, neurosurgery, pharmacology, psychology, occupational health, public health), and representatives of nursing and physiotherapy. Patients’ associations, as well as being represented in decision-making bodies of the plan (advisory council and standing committee) participated in a working group that drafted their own proposals that were discussed at the Standing Committee and incorporated into the final conclusions. They were also members of the working group on health care model. Each group had one or two officials, with the functions of directing and coordinating the group, who set the work plan and the proposed actions, always within the framework of the general objectives as defined by the MP. The working methodology consisted of regular meetings for discussion and evaluation of the proposals made by members of the group. The established care model working group was a team of people representing relevant scientific societies (rheumatology, family medicine, TOS, physical medicine and rehabilitation, anesthesia and pain management), schools or companies (physiotherapists and nurses), patient associations, entities providing different services and areas of the Department of Health. The objectives of this group were to evaluate existing models of care in other settings and make a proposal for a new model of care.
The proposals from each working group were presented in a technical report that was given to the team manager and, if approved by the Permanent Commission, presented to the advisory board for approval. The results of the MP were collected in a final document, currently available on the website of the Department of Health.8
ResultsThe overall objectives set by the MP were: (a) strengthening health promotion, prevention and self-care in diseases of the musculoskeletal system, (b) improving the response capacity of PC in these diseases, (c) reducing the variability and increasing the efficiency of the diagnostic and therapeutic process, (d) improving continuity of care and efficiency of care through the definition of a new model of care, and (e) promoting the training of professionals.
In addition to the care model group, the other groups worked on back pain, osteoarthritis, osteoporosis, arthritis, chronic shoulder pain and fibromyalgia.
Since the general objectives of the MP were common to all groups, their proposals had were marked similarities between them. For the presentation of results in this paper we will initially introduce the proposed care model and then the specific proposals of the different strategies. MP proposals are summarized in Table 2.
Summary of the MP Proposals.
| Proposals from the assistance model group. Generic proposals | |
| Elements of care shared by PC and SC | Common Assistance And Health Objectives between PC and SC |
| Process based care on prevalent diseases | |
| Definition of assistance levels, involved specialties and moment of action | |
| Detailed criteria and adequate diagnostic tests | |
| Shared clinical information between assistance levels | |
| Basic care package across assistance levels | |
| Protocol for referral | |
| Strengthening of patient associations | |
| Actions to improve resolution by PC | Incorporation of nursing in education, prevention, health promotion and disease control |
| Specific information material for health education and self care advice | |
| Promotion of physical exercise | |
| Basic physiotherapy available in the context of PC | |
| Protocol for access to complementary actions | |
| Advice in narrowing the gap between PC and SC | |
| Promotion of continuing education for physicians and nurses | |
| Promotion in the detection and declaration of musculoskeletal work related diseases | |
| Actions to improve efficiency of SC | Organization of locomotor function units with: |
| Protocols for disease care | |
| Shared clinical information | |
| Service portfolio and agreed upon access circuits between different specialties | |
| protocol for access to diagnostic tests | |
| Coordination systems | |
| Regular information on follow up and discharge directed at PC | |
| Strategic line proposals. Specific proposals | |
| Attention to osteoarthritis | Potentiation and generalization of the Arthroplasty Registry of Cataluña |
| Definition of capacitation criteria for the arthroplasty specialization team in joint replacement | |
| Attention to osteoporosis | Reducing the incidence of osteoporotic fracture through: |
| Determination of the absolute risk of fracture as an instrument of decision making in osteoporosis treatment. Validation of the FRAX index | |
| Prevention of osteoporotic fractures in high risk population, such as steroid treated patients and institutionalized persons | |
| Reducing mortality and disability associated to hip fracture through: | |
| Reduction to a maximum of 48 hours for surgery | |
| Multidisciplinary support upon hospitalization | |
| Attention to low back pain | Implementation of electronic tools for diagnosis support (quality care guidelines) and data alert on “alarm signs” |
| Analyzing variability in the indications for lumbar spine surgery | |
| Attention to chronic arthritis | Early detection of early onset arthritis cases through consulting with PC |
| A maximum time of 3 months for onset of remission inducing treatment. Creation of specific early arthritis clinics | |
| Establishment of cost benefit criteria when indicating biologic drugs | |
We propose a model of care that involves the AP and specialist care (AE) working in locomotor territorial area equivalent to the area of influence of each hospital. The elements of this new model are generic, affecting different diseases prevalent.
- 1.
Shared management elements. It is stated that the objectives and health care for certain processes and diseases are common between PC and SC with regard to responsibility for the design, implementation and achievement of these. Specific management measures are specified in Table 2.
- 2.
Actions to improve the responsiveness of PC. The actions proposed are: incorporation of nurses in education and the use of measures of health education and self-care, provision of basic physical therapy framed in the field of PC, logging of access to additional examinations depending on the complexity of pathology and a pre-defined portfolio of services, consulting face-to-face in order to close the gap between the PC and rheumatology and other specialties on demand, allowing for the improvement in attention to cases of low complexity and appropriateness of referrals to SC, promoting the continuing education of medical professionals and nurses in the areas of prevention, diagnosis, clinical management and treatment of different musculoskeletal diseases, and promoting the detection and reporting of musculoskeletal diseases through specific computer reminders.
- 3.
Actions to improve the efficiency of the SC. We propose the organization of locomotor functional units, defined as assistance units, primarily hospitals, enabling them to organize the activity of different specialties and professionals involved in the care of musculoskeletal diseases. These units, without specific hierarchical structure, are based on organizational agreements among professionals to give a single, orderly and phased answer in the care of more prevalent musculoskeletal diseases. The management of these diseases should be formalized and agreed upon between specialties with shared clinical information. This should allow continuity of care, multiple referrals and avoidance of overloading certain specialties or resources.
Specific proposals as strategic lines:
- 1.
Osteoarthritis care: enhancement and generalization of the Arthroplasty Register of Catalonia is proposed, as well as the definition of criteria for training of specialized teams for joint replacement arthroplasty.
- 2.
Care of osteoporosis raises two specific objectives: to reduce the incidence of osteoporotic fractures and reducing the mortality and disability associated with hip fractures. The first objective seeks to promote the determination of the absolute risk of fracture as an instrument of decision to initiate treatment for osteoporosis, requiring only the validation of the FRAX index in the Catalan population. For the prevention of osteoporotic fractures in high-risk populations such as patients treated with corticosteroids, the implementation of a computer alert linked to the prescription of these drugs within the PC electronic medical record is proposed. We also propose the widespread treatment with calcium and vitamin D among institutionalized persons over 65 years. To improve the process of care of hip fracture we proposed the reduction to a maximum of 48h waiting time for surgery and the provision of multidisciplinary support during hospitalization.
- 3.
Back pain care: we recommend the implementation of electronic tools to support diagnostics (such as clinical practice guidelines of proven quality) and a computer alert advising on “red flags” in back pain. We also contemplate the analysis of the variability in the indication of lumbar spine surgery.
- 4.
Care for chronic arthritis: we aim to improve early detection of cases of early onset arthritis, through consulting primary health care centers, and a maximum of 3 months for the start of remission inducing treatment in early arthritis, through the creation of specific units. We also proposed the establishment of cost–benefit criteria in the indication of biological treatments.
- 5.
Care and attention to fibromyalgia and painful shoulder. In these working groups there were no defined specific actions, with their proposals and discussed in previous sections.
The mission of the MP led by the Department of Health is to improve the care of rheumatic diseases through interventions of proven efficacy and effectiveness, and to establish a model of care focused on the needs of the population. Following these principles, the proposals include aspects of prevention, rational use of resources, improved efficiency of services, use of information technology as an aid to decision making, implementation of measures and demonstrated evidence in professional training.
Care for chronic diseases involves different levels of health care professionals and makes coordination a key process of care. Only with coordination between research and professionals can adequate care be given in the right place, ensuring continuity of care by avoiding duplication and optimally managing transitions between levels of care.
It is not usual in our country to have a health planning focused on musculoskeletal problems. Back in the nineties, the Health Plan of the Ministry of Health and Consumption9 recognized these diseases as a priority intervention area due to its high morbidity and potential for impaired quality of life, disability, restricted activity and high consumption of drugs, as well as health and labor costs associated with it. Since then, different regions have been introducing elements unevenly. Certain lines, such as cancer, cardiovascular diseases or mental disorders are common to many, but in this case there are only are isolated lines specifically targeted to rheumatic problems. Several health plans, such as Galicia's and Andalusia's advocate generic measures, such as promoting healthy lifestyles (exercise, control of obesity, improved postural hygiene), the protocols for certain processes or formation of PC professionals. Among the objectives directed to specific problems we can find the plan of Valencia, aimed at the prevention and management of osteoporosis, which has shown positive results.10 A different situation is presented by several developed countries where the “Bone and Joint Decade 2000–2010”11 led to the implementation of different initiatives. This project began in 1990, backed by the United Nations Organization and the World Health Organization as a global initiative whose objectives were to promote research and increase awareness and education on musculoskeletal diseases. The ‘Decade’ objective was to improve the quality of life of people with these conditions, raising awareness about the growing burden to society, promoting effective preventive measures and treatment, and stimulating research in order to generate appropriate prevention strategies and treatment. 63 governments gave support to this initiative, including 28 European countries (not Spain) and more than 850 entities, of which 7 were Spanish. The activities of the “Decade” ended in September 2010 and due to the success and recognized the importance of their actions have been extended another decade (http://www.boneandjointdecade.org).
The statement of the European Parliament on rheumatic4 diseases lies in this direction, in which a number of considerations recall their high prevalence, chronic condition and the fact that they are a leading cause of disability and early retirement for workers. The adoption of adequate social and health policies reduces economic and social costs associated with these diseases. Therefore, the Parliament urges Member States to establish and implement national plans to fight rheumatic diseases, and develop a strategy on them.
The MP is designed for a period of 4 years, time for the goals of care to the population and the actions that will make it possible to achieve these objectives through operational planning and buying services to the various suppliers to be achieved. The future phase of the plan is the gradual implementation and evaluation of results. We hope these will vouch for the validity of their proposals and content, and efficiently display their generalization to benefit the health of our citizens.
Conflict of InterestThe authors declare no conflict of interest.
Please, cite this article as: Larrosa M, et al. Planificación en enfermedades reumáticas. Elaboración del Plan director de las enfermedades reumáticas y del aparato locomotor de Cataluña. Reumatol Clin. 2012;8(2):72–7.