Recently, we treated a patient with interstitial granulomatous dermatitis (IGD) associated with systemic lupus erythematosus (SLE). Given the refractoriness of the condition to standard therapy, treatment with belimumab was begun, and the response was satisfactory. In view of the absence of data in the literature on the efficacy of belimumab in IGD associated with SLE, the report of this case was considered to be interesting, as it would enable us to examine new therapeutic lines in refractory IGD.
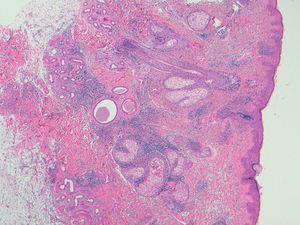
The patient was a 40-year-old white man who had been diagnosed with SLE at the age of 35 on the basis of leukopenia, oral and nasal ulcers, arthritis of the hands, myositis and cutaneous involvement in the form of diffuse alopecia. He was also positive for immunological markers (antinuclear, anti-Smith, anti-Ro and anti-double-stranded DNA antibodies) and had decreased complement levels. Given the predominance of joint involvement, at first, he was treated with prednisone at 10mg/day and hydroxychloroquine at 400mg/day. There was a partial response in the joints, but none with respect to the skin. He had a substantial deterioration of the cutaneous manifestations, developing patches of alopecia areata, palpebral edema and nonpruritic, erythematous violaceous macular lesions on his face, torso and proximal portion of extremities, producing a serious physical and psychological distress for the patient. In addition, he had constitutional symptoms, with fever and an elevation of serum markers of lupus activity. A biopsy of the skin lesions revealed an interstitial lymphohistiocytic infiltrate in superficial and deep dermis, with the presence of mucin deposits arranged around collagen fibers, corresponding histopathologically to IGD (Fig. 1). It was decided to treat the patient with high-dose corticosteroids (1mg/kg body weight [bw]/day of prednisone), to which he responded only partially. His response to the association of metronidazole (250mg/8h) and mycophenolate mofetil (1g/12h) was not satisfactory either, and he did not tolerate methotrexate. Given the high clinical activity and extension of the lesions, we decided to start treatment with intravenous belimumab (10mg/kg bw each month), associated with hydroxychloroquine. The patient showed an evident satisfactory response after 1 month of treatment, with resolution of the skin lesions and alopecia, as well as clinical remission and normalization of the biological parameters. Four years after the start of this approach, he remains in remission.
Interstitial granulomatous dermatitis is an uncommon skin condition, that is occasionally associated with autoimmune diseases (rheumatoid arthritis, SLE, vasculitis, thyroiditis or diabetes), lymphoproliferative disorders and even certain drugs like anti-tumor necrosis factor agents.1,2 The skin lesions usually develop in patients with SLE although, in some cases, they can also be the presenting sign of the disease.3 Its treatment has not been well established. In the case of IGD associated with drugs, it seems to be necessary to discontinue the causative agent and assess introducing treatment with corticosteroids. In general lines, these are the primary therapeutic options for IGD. In cases of IGD associated with an autoimmune disease, it may be necessary to combine corticosteroids with the treatment of the underlying disease. For this, we utilize immunosuppressive drugs, like methotrexate, mycophenolate, hydroxychloroquine, dapsone and even metronidazole (the latter indicated in granulomatous diseases). Our patient did not tolerate methotrexate or respond to other treatments. With respect to biological therapy, there are reports of cases of IGD associated with arthritis in which there was a good cutaneous response to infliximab,4 etanercept,5 tocilizumab,6 ustekinumab7 and immunoglobulins,8 treatments that were not indicated in our patient. Belimumab has been seen to be effective in individuals with SLE and with cutaneous and joint involvement that is refractory to standard immunosuppressive agents.9 There is no evidence of its efficacy in IGD. It is a fully humanized monoclonal antibody against B lymphocyte stimulator (BlyS), the action of which focuses on the indirect depletion of B lymphocytes and plasma cells, thus reducing the production of antibodies. Given the elevated clinical and serum activity, considering the extension, severity and refractoriness of the skin lesions, we began treatment with belimumab, which achieved complete resolution of IGD. These results are surprising, considering that the mechanism of action of this drug does not appear to be related to the pathophysiology of the granulomatous lesion. The literature provides cases in which the development of IGD associated with autoimmune diseases was related to the presence of autoantibodies and immune complex deposition.10 This suggests that the depletion of these elements would impede the perpetuation of the inflammatory cascade causing the granuloma.
In short, the development of IGD during the course of SLE is an uncommon cutaneous condition, with no established treatment, and it may be resistant to different therapeutic strategies. The case we report is the first in which belimumab was found to be effective in IGD associated with SLE.
Please cite this article as: Arévalo M, Moreno M, Gratacós J. Dermatitis intersticial granulomatosa asociada al lupus: a propósito de un caso. Reumatol Clin. 2017;13:367–368.