Overlap syndromes are uncommon conditions in which the diagnostic criteria of more than one systemic autoimmune disease are met in a single patient.1 In contrast to mixed connective tissue diseases (MCTD), in which certain clinical or serological characteristics are identified, they do not fulfill the diagnostic criteria in order to be categorized as a defined disease.1,2
“Rhupus” is an entity in which there is an overlap of systemic lupus erythematosus (SLE) and rheumatoid arthritis (RA), and the incidence involves less than 1% of the SLE population.1,2 Autoimmune hepatitis (AIH) is a chronic progressive liver disease. Its prevalence is relatively low, as it affects around 16.9 individuals in population of 100,000.3
We report the case of a 30-year-old woman, with a history of RA, who came to the hospital with acute pyelonephritis. Therapy was begun with antibiotics and symptomatic treatment, and the patient responded favorably. Four days later, she presented with pain in hypogastrium and right hypochondriac region, nausea, vomiting, paleness, pain and stiffness in the metacarpophalangeal joint (with synovitis) and bilateral coxofemoral joint, red eye syndrome, malar erythema and photosensitivity.
Ancillary tests: albumin: 4g/dL; globulin: 4g/dL; immunoglobulin (Ig) G: 1669.4mg/dL; IgM: 473.0mg/dL; antinuclear antibodies positive: 1/400, homogeneous pattern; native SS-A+++; single-stranded DNA++; RNP: positive; RNP A: negative; RNP C: negative; Scl 70: negative; PM-Scl: negative; Jo-1: negative; centromere protein B: negative; serum complement C3-C4 level: low; lupus anticoagulant (kaolin): 0.83 (−); IgG anticardiolipin: 12 (+); IgM anticardiolipin: 19 (+); and beta 2 glycoprotein I: not determined.
Total bilirubin: 1.5mg/dL (0.4–1.2mg/dL); direct bilirubin: 1mg/dL (0–0.3mg/dL; aspartate aminotransferase: 31IU/L; alanine aminotransferase: 25IU/L; gamma-glutamyltransferase: 61IU/L; prothrombin time: 13.9s; international normalized ratio (INR): 1.22; Australian antigen (HBsAg): negative; anti-hepatitis C virus: negative; anti-hepatitis A virus (HAV) IgM: negative; rheumatoid factor: 21IU/mL; erythrocyte sedimentation rate: 66mm/h; anti-smooth muscle antibodies (+); and anti-liver-kidney microsomal (LKM) antibody: negative.
Abdominal ultrasound: chronic diffuse liver disease and hepatomegaly, right diffuse renal disease and nephromegaly.
Soft tissue ultrasound: capsular distension with effusion, synovitis in proximal metacarpophalangeal joints compatible with RA.
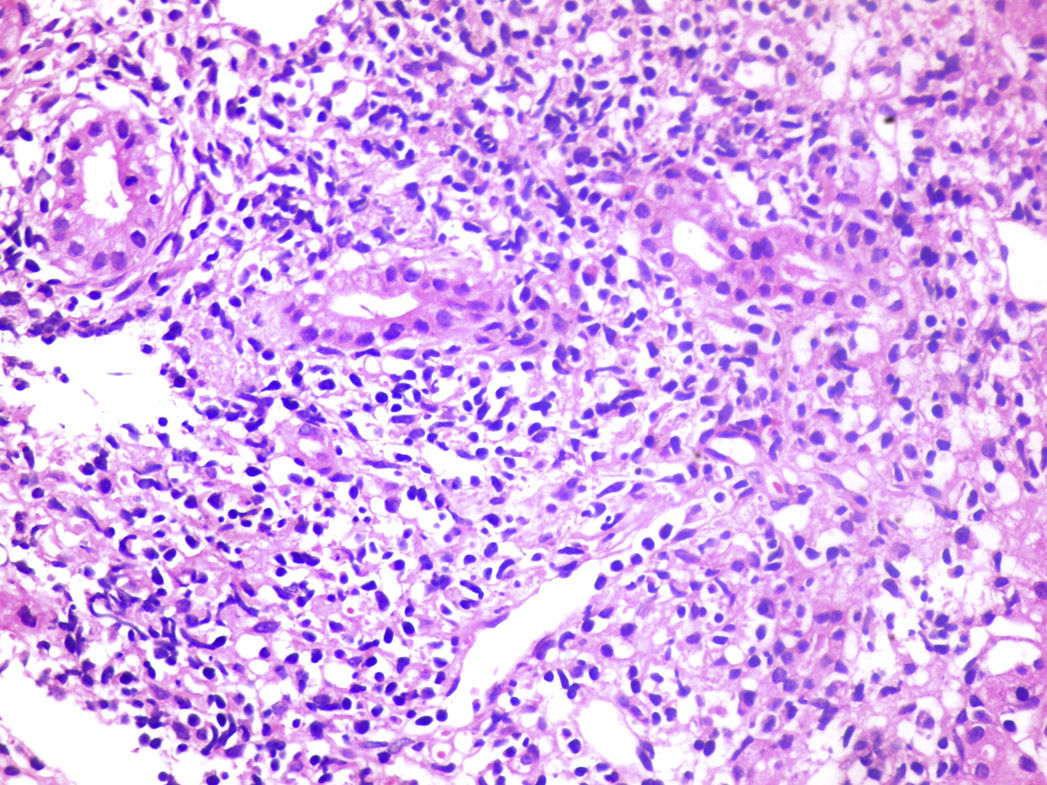
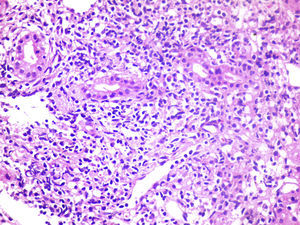
Liver biopsy: changes in liver architecture, with portal spaces widened by the chronic mononuclear lymphocytic inflammatory process that damaged the limiting plate. Presence of piecemeal necrosis, or interface hepatitis, necroinflammatory foci, mild plasmacytosis, binucleated reactive hepatocytes, disarranged trabeculae (Fig. 1). The findings were consistent with chronic active liver disease.
Symptoms suggestive of SLE were manifest. Thus, we requested an immunological profile that subsequently would corroborate the diagnosis, together with the history of RA and evidence from the soft tissue ultrasound, pointed to the diagnosis of rhupus. Patients with rhupus often present with a diagnosis of RA and, later, develop secondary signs of SLE.4 The clinical symptoms and signs associated with SLE in rhupus are cutaneous photosensitivity, malar rash, alopecia, and hematologic changes such as leukopenia and thrombocytopenia. Renal and neurological involvement are uncommon.5,6
Diffuse liver disease, hypergammaglobulinemia and the presence of anti-smooth muscle antibodies were noteworthy and, given the suspicion of AIH, we requested a liver biopsy. The findings were consistent with interface hepatitis with mononuclear infiltrate, and the simplified criteria for AIH were evaluated7 and the result was positive, with a score of 7.
The presence of antiphospholipid (aPL) antibodies pointed to the suspicion of aPL syndrome. However, the absence of clinical manifestations or obstetric history ruled it out. Another study found that up to 3% of the patients with autoimmune liver disease had aPL, although this result was not significant.8
In conclusion, the overlap of rhupus and autoimmune hepatitis is an uncommon condition that requires suspicion on the part of the clinician and multidisciplinary management for appropriate treatment.
AuthorshipEZF and DLO participated in the conception of the article, in its writing and in the critical review of the text. All of the authors approved the article for publication.
Please cite this article as: Zavala-Flores E, Loja-Oropeza D. Rhupus y hepatitis autoinmune: una asociación infrecuente. Reumatol Clin. 2017;13:365–366.