We report a case of de novo lipoma arborescens in a pediatric patient, in which nuclear magnetic resonance (NMR) was decisive in the diagnosis, ruling out other causes of monoarthritis.
Lipoma arborescens is an uncommon benign tumor affecting synovial joints and bursae, that is characterized by the replacement of normal synovial tissue by mature fat cells, which provokes villous lipomatous proliferation. It is usually associated with synovitis.1,2 The cause is unknown and, although it has been reported in both adults and children, there are very few articles involving the latter.
It typically affects the suprapatellar pouch of the knee joint and is, usually, monoarticular, although there are cases in which it is bilateral or occurs at another location like the elbow, ankle, wrist or hip.1,2
In most cases, it occurs de novo, but it is not that rare that it be associated with osteoarthritis, rheumatoid arthritis or an injury.1–4
The clinical signs include intermittent episodes of pain and joint inflammation with inconclusive laboratory findings and synovial fluid that shows no evidence of inflammation.1,2,5
Although plain radiography, ultrasound, arthrography and computed tomography can be of help, NMR is the best imaging technique for the diagnosis.6–9
The recommended treatment is total synovectomy1,2,5 by arthrotomy or arthroscopy.
Our patient was a 12-year-old girl with no significant previous medical history, except for a diagnosis of septic arthritis of the shoulder when she was 9. She had been treated with empirical antibiotic therapy and arthrotomy for drainage. There had been no signs of microorganisms in either the synovial fluid or blood cultures. All of the studies performed during her hospital stay were negative and all of the symptoms had completely disappeared.
Three months before a follow-up visit, she noted progressive inflammation in her right knee, with occasional functional disability. She came to the emergency department, where she underwent arthrocentesis, which yielded a yellowish fluid with negative cultures, including Ziehl-Neelsen staining and culture on Löwenstein-Jensen medium. She was referred to rheumatology to be studied.
She had no other symptoms or evidence of disease in a physical examination, except swelling of the knee, which was painless at that time, and there was only slight synovial effusion. Chest radiograph was normal, purified protein derivative (PPD) test was negative, complete blood count was normal, erythrocyte sedimentation rate 6mm/h, urine analysis normal, C reactive protein 0.21mg/L, antinuclear antibody test negative, rheumatoid factor 7IU/mL, immunoglobulins normal, human leukocyte antigen (HLA)-B27 negative, and her celiac profile and α-1-acid glycoprotein were normal.
We also took a plain radiograph of the knee, which was normal.
Ultrasound of the affected knee: marked thickening of the synovium, especially in the suprapatellar recess, where it was accompanied by slight joint effusion. The synovial membrane showed, at some points, polypoid thickening that seemed to be floating in the middle of the effusion.
Right knee NMR: there was a small Baker's cyst on the medial side of the popliteal fossa and a moderate joint effusion in the suprapatellar recess. In the middle of the effusion there was a marked thickening of the synovial membrane that gave it finger-like or polypoid images, and occupied the suprapatellar recess, Hoffa's fat pad and the part adjacent to the cruciate ligaments and menisci. These formations had a signal like that corresponding to fat. After the intravenous administration of the contrast medium, there was an enhancement marked by the synovium that surrounded the polypoid lesions. This image was the confirmation of lipoma arborescens (Fig. 1).
Ultimately, we decided to perform an NMR study of the patient's shoulder in view of the septic arthritis, and the result was normal.
She was referred to an orthopedic surgeon for synovectomy, and the symptoms disappeared.
Five months after the synovectomy, she noted inflammation in the left knee and functional disability. Nuclear magnetic resonance and ultrasound led to a diagnosis of lipoma arborescens.
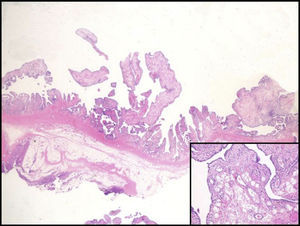
She underwent surgery, and the pathological study of the synovial membrane confirmed the diagnosis (Fig. 2).
Nuclear magnetic resonance can be highly useful in the evaluation of noninflammatory processes in patients with atypical monoarthritis.
Please cite this article as: Ruiz Montesino MD, Moreira Navarrete V, Vargas Lebrón C, Rios-Martín JJ. Lipomatosis arborescens en rodilla pediátrica. Resonancia magnética nuclear. Reumatol Clin. 2017;13:180–181.