Macrophage activation syndrome (MAS) occurs in a minority of patients with adult Still's disease (ASD).1,2 It can be the diseases’ first manifestation or be triggered by an infection or change in treatment.3 Two cases are presented.
The first case is a 30-year-old woman with ASD, who came to the ER with a fever lasting for one week that did not improve with antibiotics, so she was admitted to the Rheumatology department. During admission, treatment with ceftriaxone and glucocorticoids (GC) mg/kg was started, and multiple complementary tests performed: blood culture positive for pneumococcus and positive serology for cytomegalovirus; analytically: hepatitis, elevated acute phase reactants (APR), hyperferritinemia, hypertriglyceridemia, thrombocytopenia, and anemia, in addition to splenomegaly in the computed tomography (CT).
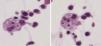
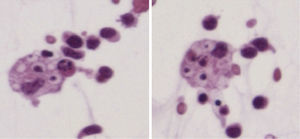
Despite treatment, evolution was unfavorable, with persistent thrombocytopenia and declining ESR. With these data, we decided to perform a bone marrow biopsy (BMB), observing hemophagocytic cells (HC), diagnosing MAS and initiating treatment with cyclosporine (CSP) 5mg/kg/day and 60GC mg/day, with progressive improvement.
The second case is a 35-year-old woman who presented with fever, a sore throat, musculoskeletal pain, vomiting and rash for a week, diagnosed as the flu. Three days later she came to the ER because of persistent fever and rash, and the onset of lymphadenopathy, and was hospitalized. During admission, treatment was started with ceftriaxone and gentamicin; associated infection and autoimmunity was ruled out. Analytically she presented: anemia, elevated APR, hepatitis, hyperferritinemia, hypertriglyceridemia, impaired renal function and ascites. A CT was performed, which reported a systemic infection with lymphadenopathy and hepatosplenomegaly.
The initial suspicion was ASD, starting GC therapy at a dose of 1mg/kg/day and presenting an initial improvement. Subsequently, the fever persisted and skin lesions progressed, added to respiratory and renal failure, which led to her transfer to the Intensive Care Unit (ICU) of our hospital. On admission to the ICU, we performed a BMB, ascites analysis, observing HC in both (Fig. 1). She was diagnosed as MAS. Evolution was poor despite GC, so we added CSP 5mg/kg/day, with partial improvement and anakinra 100mg/day. The evolution was favorable, so she was transferred to the rheumatology department, where after a few days she was discharged.
Both conditions share several features, such as fever, hepatosplenomegaly, lymphadenopathy, hepatitis, coagulopathy and hyperferritinemia, and often are indistinguishable.2,3 Pleuritis, acute respiratory distress syndrome and pancytopenia are more common in the MAS1,2 and cutaneous and articular affection in ASD.2,3 Leukopenia, thrombocytopenia and hypertriglyceridemia are not common in ASD, so these could serve as warning signs1,2; Additionally, hyperferritinemia is generally higher in MAS.2,4
Most of the cases described in the literature have been treated with GC, immunoglobulins, CSP and biological drugs.1,2 Both conditions share certain pathophysiologic characteristics such as the production factor tumor necrosis α and interleukins (IL), IL-1, IL-6, IL-8 and IL-18, with these being potential therapeutic targets.5,6
The first patient probably presented MAS after a triggering infection. We hypothesize that the MAS in ASD can occur after a change in treatment or an infection; the most studied is the Epstein–Barr virus infection, but it has also been described2,3,6 in cases of cytomegalovirus.
Patient 2 presented HC in ascites; the first case was described in 2007 in a patient with liver cirrhosis and Escherichia coli infection.7 In addition, cases described with HC in8,9 pleural fluid and in cerebrospinal fluid.10
Conflict of InterestThe authors have no disclosures to make.
Please cite this article as: Egües Dubuc C, Uriarte Ecenarro M, Errazquin Aguirre N, Belzunegui Otano J. Síndrome de activación macrofágica como complicación severa de la enfermedad de Still del adulto. Células hemofagocíticas en líquido ascítico. Reumatol Clin. 2014;10:420–421.