To analyze the requirements for osteoporosis (OP) treatment of primary care physicians (PCP), before and after knowing the result of a bone densitometry (DXA).
Material and methodsStudy of over 50 women from two Spanish health areas (Canary Islands and Alicante). The FRAX risk factors were collected and we reviewed the requirements for OP treatment before DXA and in the subsequent months (bisphosphonates, strontium, raloxifene/bazedoxifene, estrogens, parathyroid hormone). To evaluate the appropriateness of treatment we used published guidelines. A high risk for hip fracture was considered if FRAX ≥3% or the patient had a history of fragility fracture
ResultsWe included 339 women (mean age: 63 years). Before DXA, 14% of Canarias and 58% of Alicante were receiving treatment. 37% of treated patients and 26% of the untreated patients had a high fracture risk before DXA. The average FRAX for a high risk of fracture and hip fracture was 5.6% and 2%, respectively. After DXA, the percentage of patients treated rose from 35% to 39%: increasing from 14% to 28% in the Canary Islands and dropped from 58% to 51% in Alicante. Overall, treatment was received by 64% of cases with OP, 38% of patients with osteopenia and 15% of those with normal DXA. When the OP treatment guidelines were applied, we found that 7% needed treatment according to the more restrictive guideline up to 43% with the most flexible one.
ConclusionsThere is great variability in treatment for OP prescribed before and after DXA between GP. A broad consensus guideline between different specialties is required to optimize clinical practice.
Analizar las prescripciones de tratamiento para la osteoporosis (OP) de los médicos de atención primaria (AP), antes y después de conocer el resultado de la densitometría ósea (DXA).
Material y métodosSe estudió a mujeres mayores de 50 años procedentes de 2 áreas sanitarias españolas (Islas Canarias y Alicante). Se recogieron los factores de riesgo del FRAX y se revisaron las prescripciones de tratamiento para OP antes de la DXA y en los meses posteriores (bisfosfonatos, estroncio, raloxifeno/bazedoxifeno, estrógenos, parathormona). Para evaluar lo apropiado del tratamiento, se utilizaron guías publicadas. Se consideró riesgo elevado de fractura si FRAX para cadera ≥ 3% o historia de fractura por fragilidad.
ResultadosSe incluyó a 339 mujeres (edad media: 63 años). Antes de la DXA, recibían tratamiento el 14% de Canarias y el 58% de Alicante. Un 37% de las pacientes tratadas y un 26% de las no tratadas antes de la DXA tenían un riesgo de fractura elevado. El FRAX promedio para fractura mayor y para fractura de cadera fue 5,6% y 2%, respectivamente. Tras la DXA, el porcentaje de pacientes tratadas pasó del 35 al 39%: aumentó del 14 al 28% en Canarias y se redujo del 58 al 51% en Alicante. En conjunto, recibía tratamiento: el 64% de los casos de OP, el 38% de las osteopenias y el 15% con DXA normal. Cuando se aplicaron las guías de tratamiento de OP, se obtuvo desde un 7% a tratar con la guía más restrictiva hasta un 43% con la más flexible.
ConclusionesExiste gran variabilidad en la prescripción de tratamiento para la OP antes y después de la DXA entre los médicos de AP. Se precisa de una guía de consenso amplia entre las diferentes especialidades para optimizar la práctica clínica.
Osteoporosis (OP) is a skeletal disorder characterized by a disturbance of bone strength, which predisposes to an increased risk of fracture.1 The public health impact is enormous, due to the high morbidity and impact on quality of life when fractures are involved, as well as the fact that it leads to very high health spenditure.2–4
Among doctors who handle OP, diagnostic approaches and treatments are very heterogeneous. There are patients who remain untreated despite a high risk of fracture, while others receive only medication based on the results of densitometry (DXA), and some are treated even without DXA or prior risk assessment. It is essential to distinguish between patients with increased risk of fracture, which are those that are going to benefit from drug treatment, so favorable interventions to optimize the risk/benefit ratio may be designed. Different instruments have been developed to estimate fracture risk based on risk factors, one of them is the FRAX tool® published in 2008 (http://www.shef.ac.uk/FRAX/). It is a computer application that combines the different clinical risk factors for fracture, with and without DXA.5 FRAX® calculates the absolute 10-year probability of major fracture (spinal, forearm, hip and humerus).
Although FRAX® has limitations in a situation where DXA is not available, or when there is the possibility of requesting it, its use would allow recommendations for or against the treatment, or request a DXA in doubtful cases. If you have DXA, the FRAX® is also very useful because the value of BMD is one of the factors that influence the risk of fracture, along with the age and history of fracture.6 The score varies widely according to ethnicity. Consequently, the definition of high, moderate or low risk must be defined for each country. Some authors have proposed that the elevated risk for Spanish population could be at >10% for major fracture.7
Despite the limitations and expert opinions for its improvement, the use of a tool such as FRAX® can be useful for professionals aware of the importance of assessing the risk of fracture that is not based solely on the results of DXA.8
Many OP patients are treated in primary care (PC), so general practitioners should have sufficient knowledge and diagnostic tools to treat these patients. However, we found a large variability in the application of tools such as FRAX®, as well as between the different national and international guidelines for the management of OP.6,9–11
In the CANAL (Canary-Alicante) study, we decided to analyze prescribing habits for OP treatment in postmenopausal women by primary care physicians, before and after performing DXA. We also compared the results with those that would result from applying 3 different clinical guidelines for the treatment of the OP.
Materials and MethodsWe studied women over 50 years of age who had been requested their first DXA by a PCP. The study was undertaken in the last quarter of 2010 in two Spanish health areas: Marina Baixa (Hospital of Villajoyosa, Alicante) and Gran Canaria Norte (Hospital Dr. Negrin, Las Palmas). At the time of DXA, the following data were collected: age, sex, weight, height, history of parental hip fracture, personal history of fragility fracture after age 50, early menopause, treatment with glucocorticoids, toxic habits, rheumatoid arthritis and other causes of secondary OP. We inquired on OP pretreatment. This was confirmed on computerized medical records before performing DXA and 3 months later.
Medications for OP considered were bisphosphonates, strontium ranelate, selective modulators of estrogen receptors (SERM), estrogen and PTH (teriparatide and 1–84).
DXA was performed using a Hologic QDR 4500W (Gran Canaria) and a Lunar DPX/General Electric (Alicante). The results were classified into groups proposed by the World Health Organization (normal, osteopenia or osteoporosis) by the worst T score, obtained in the spine and femoral neck.
The FRAX® index was available online, for Spanish population. We calculated the absolute risk, at 10 years, of hip fracture and major fracture (vertebral, hip, forearm and proximal humerus). We defined high risk of fracture when this was equal or higher than 3% for hip fracture.
To compare the therapeutic decisions made by primary care physicians to those derived from the clinical guidelines for the treatment of OP, we used the following documents:
- 1.
Consensus document of the Spanish Society of Rheumatology (SER)9 which recommends treating all patients with low-intensity trauma fracture, regardless of the DXA; to all OP patients, to patients with osteopenia and increased risk of fracture (high risk interpreted for this study when the FRAX® was greater than or equal to 3% for hip fracture).
- 2.
Recommendations for the assessment and treatment of OP in the Community of Madrid10: it is applied to women with primary OP after menopause, after age 50, giving treatment to those with OP by DXA with medium risk (10%–20%) for hip fracture or vertebral morphometric fracture in the next 10 years, from their own risk tables. Patients with very high risk of fracture (>20%), regardless of the values of the DXA also receive treatment.
- 3.
National Osteoporosis Foundation (NOF)11: which recommends treating all patients with hip and vertebral fracture, patients with T score values <−2.5, and patients with values in the range between −1 and −2.5 and a FRAX index® ≥3% or ≥20% higher for OP major fracture.
Descriptive statistics were performed to estimate the significance of differences at 0.05. To compare results between groups we employed contingency tables when the variables were qualitative and Student's t-test when the variables were numeric.
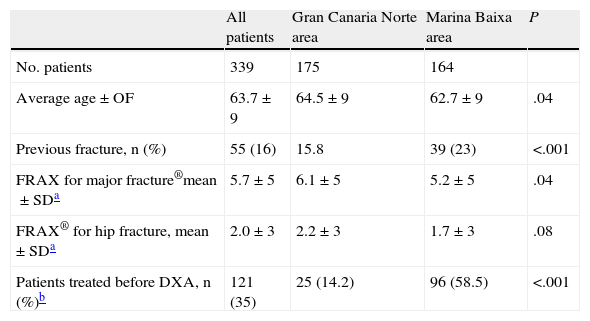
ResultsThe study included 339 women with an average age of 63 years. The distribution of age by decades was as follows: 131 (38.6%) under 60, 118 (34.8%) between 60 and 70, 64 (18.9%) between 70 and 80 and 26 (7.7%) over 80 years of age. Other features and the comparison between health areas are shown in Table 1.
Characteristics of the Women Included.
| All patients | Gran Canaria Norte area | Marina Baixa area | P | |
| No. patients | 339 | 175 | 164 | |
| Average age±OF | 63.7±9 | 64.5±9 | 62.7±9 | .04 |
| Previous fracture, n (%) | 55 (16) | 15.8 | 39 (23) | <.001 |
| FRAX for major fracture®mean±SDa | 5.7±5 | 6.1±5 | 5.2±5 | .04 |
| FRAX® for hip fracture, mean±SDa | 2.0±3 | 2.2±3 | 1.7±3 | .08 |
| Patients treated before DXA, n (%)b | 121 (35) | 25 (14.2) | 96 (58.5) | <.001 |
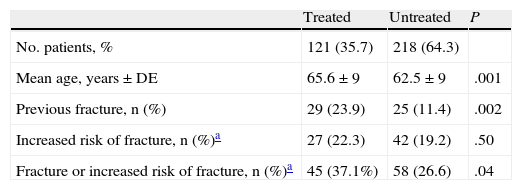
16% of women had a history of fragility fracture, although the percentage was significantly higher in the group that received treatment (Table 2). 35% of the patients received treatment before DXA, and most used bisphosphonates (85%).
Characteristics of the Treated and Untreated Women Prior to the Completion of Densitometry.
DXA was normal in 87 cases (25%), showed osteopenia in 158 (46%) and OP in 94 (27%). The percentage of regular DXA was significantly higher in Gran Canaria (32.8%) than in Marina Baixa (20.3%) (P=.02).
By introducing the value of DXA® into FRAX, the average absolute risk decreased to 5.1% (±5.1) for major fracture and 1.5% (±1.5) for hip fracture.
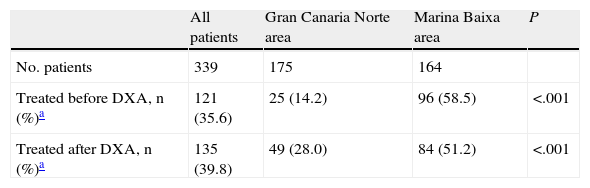
Treatments After Bone DensitometryThe percentage of women treated after DXA increased from 14% to 28% in Gran Canaria and was reduced from 58% to 51% in Marina Baixa (Table 3).
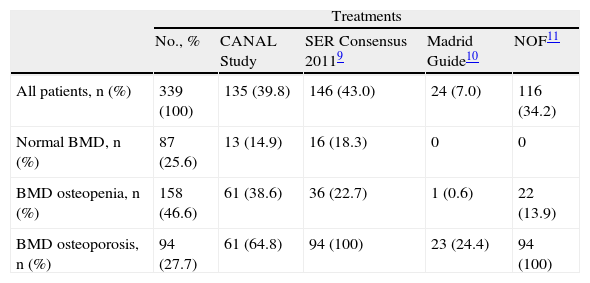
Table 4 shows the estimation of patients to be treated by guided management proposed by 3 guidelines for OP.
Patients Treated and Estimation of Different Treatment According to Clinical Guidelines.
| Treatments | |||||
| No., % | CANAL Study | SER Consensus 20119 | Madrid Guide10 | NOF11 | |
| All patients, n (%) | 339 (100) | 135 (39.8) | 146 (43.0) | 24 (7.0) | 116 (34.2) |
| Normal BMD, n (%) | 87 (25.6) | 13 (14.9) | 16 (18.3) | 0 | 0 |
| BMD osteopenia, n (%) | 158 (46.6) | 61 (38.6) | 36 (22.7) | 1 (0.6) | 22 (13.9) |
| BMD osteoporosis, n (%) | 94 (27.7) | 61 (64.8) | 94 (100) | 23 (24.4) | 94 (100) |
CANAL, Canary Islands-Alicante study; BMD, bone mineral density by densitometry; NOF, National Osteoporosis Foundation; SER, Spanish Society of Rheumatology.
The CANAL study systematically recorded risk factors included in the FRAX®, DXA results and the treatments received by patients in two Spanish health departments. They had been referred for DXA by their primary care physicians in a real clinical situation.
Our data on the percentage of OP diagnosed by DXA and its treatment are very similar to those of the ESOVAL study, which collected data from 5310 women from 272 health centers in Valencia.12
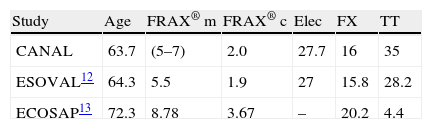
However, the average FRAX estimate® and a history of fractures are lower than13 in the ECOSAP study, which included 5201 Spanish women recruited in 52 PC centers, probably because these patients were older (Table 5).
Comparison of CANAL Study Results With Other Spanish Studies.
| Study | Age | FRAX® m | FRAX® c | Elec | FX | TT |
| CANAL | 63.7 | (5–7) | 2.0 | 27.7 | 16 | 35 |
| ESOVAL12 | 64.3 | 5.5 | 1.9 | 27 | 15.8 | 28.2 |
| ECOSAP13 | 72.3 | 8.78 | 3.67 | – | 20.2 | 4.4 |
Data are expressed as means and %.
CANAL, Canary Islands and Alicante; FRAX® c, hip fracture; FRAX® m, for major fracture; FX, fractures; OP, densitometric osteoporosis; TT, treatment for osteoporosis.
In our experience in PC and also in specialized care, there is little use of FRAX® and other tools for fracture risk assessment. As in other studies in Spain, the absolute risk of fracture at 10 years, calculated by FRAX®, in patients referred to a bone densitometry unit for BMD assessment is low.7
In the study of Gómez-Vaquero et al., the average risk of fracture without inclusion of DXA was 10% lower when DXA was included in the calculation,7 results similar to those shown in our work.
In our study only one-third of the patients who were sent to a DXA by their PC doctor had an increased risk of fracture, which indicates that we must insist on the calculation of fracture risk in health centers before applying DXA. Who should be submitted to a DXA remains an open question. In addition, the more DXA was requested, the more patient candidates appeared, in our series one in every 4 cases.
In our country there have been several studies in PC on the applicability of FRAX® to determine the absolute risk of fracture in postmenopausal women depending on the outcome and consider recommendations on whether to request DXA and/or initiate antiresortive treatment.14,15 Serra Torresa et al. after evaluating 118 patients with osteopenia from an urban health center in Barcelona, tested data from the clinical history and determined that 16% were receiving a bisphosphonate or raloxifene, and that treatment was more frequent in patients with lower bone mass; however, a previous fracture did not influence the treatment.16
The burden of care, together with the large volume of knowledge required by primary care physicians for their daily work, makes OP a priority condition or not to be treated according to the preferences of each doctor. This is compounded by the lack of unanimity of the existing guides when applying for DXA and, above all, defining which patients to treat.
In this study, 40% of patients eventually received treatment after DXA, drawing attention to the fact that treatment was not started in a third of cases of DXA with OP, while treatment was maintained in 15% of cases with standard DXA. However, in our opinion prescribing habits of PC physicians in management before DXA are more questionable: only 37% of women treated had a prior fracture or high risk of hip fracture, i.e. another 63% were treated without the ‘high risk’. In 26.5% of the untreated group, on the other hand, there was increased risk of fracture, so they could have benefitted from treatment.
In the present study, 121 patients were treated for OP (35.7%), at the time in which they were referred for DXA. The indication for treatment, prior to DXA, it seems, had been adequate. In fact, only 37.1% of treated women had a higher risk of hip fracture (FRAX® high or previous fractures), i.e., another 62.9% were treated without the “high risk” (overtreatment). In contrast, 26.5% of those untreated did present these circumstances, so they could have benefited from an antiosteoporotic drug, but were not receiving treatment (undertreatment).
When DXA was performed, the number of women treated increased to 135, representing an increase of 11.5% of treatments. In reality, there was a redistribution of the treatments, as primary care physicians in the Canaries, who had fewer previous treatments, doubled them, while Alicante fell by 12.5% (Table 3). Both populations were collectively similar in risk factors (FRAX®), but Alicante had the most prevalent fractures, so that in this group, the result was somewhat less critical for DXA, since it is plausible that the treatment continued if the patient had fragility fractures.
Studies conducted in Spanish PC, in different regions, on the closeness of the prescription to the recommendations of various guidelines for the management of OP are extremely variable, ranging from 15% of inappropriate prescribing in two PC centers in Barcelona, up to 48% of cases that did not meet criteria for treatment in the community of17,18 Madrid.
We have contrasted the treatment requirements made by our primary care physicians to the SER guidelines, the recommendations of the Community of Madrid and NOF.9–11 The SER Guide is the most flexible as it allows to treat all cases with a history of fracture. This is debatable, since in women with forearm fracture under 65 years have less than half the increased risk of fracture as quantified by FRAX®.6 In addition, the SER guide does not clearly define which cases are at high risk of fracture, so that the estimate we have made with FRAX® ≥3% for hip fracture is indicative only.
On the opposite side of forearm fractures we would find hip and vertebrae fractures, in which case the majority will present OP by DXA and immediate treatment would be indicated as advised by most of the guidelines.
The guide of the Community of Madrid is more restrictive because, in applying risk tables, this is low in the 50–60 years of age group, so treatment is not recommended. From age 60, treatment is defined by age, the results of the DXA and the percentage of risk for hip fracture and vertebral morphometry in the next 10 years. However, the NOF guide seems reasonable because it includes those patients with osteopenia and increased risk of fracture (in our case 14% of all osteopenias). Finally, the guide of the Spanish Society of Family and Community Medicine (not included in the analysis of this paper) algorithm introduced, for the treatment of OP, the presence of a previous fracture, and in the absence of the same, considering age, DXA results and other risk factors.19
Although there are no thresholds considered for high risk of fracture by FRAX® in the Spanish population, some authors believe that the figure of 10% may be appropriate for major fracture.7 In our study, we found that 47 patients (13%) met this criterion (including DXA, data not shown), while the recommendation of Anglo-Saxon countries of ≥3% for hip fracture was met the 72 patients (21%). Thus, if the NOF guide is adapted to a hypothetical high risk threshold for the Spanish population of 10% for major fracture, the percentage of patient candidates would be reduced from 34% to 30%, at the expense of a reduction of osteopenias treated from 14% to 6%.
In conclusion, with the CANAL study we noted a large variability in the prescribing habits for OP treatment depending on the health area. Although the prescription prior to DXA is often performed in patients at increased risk of fracture, only a third have high risk by FRAX® and/or a history of fracture. After performing the DXA, an adjustment is made of the treatment, however, one-third of the cases with DXA OP remains untreated and one out of 6 patients with treatment has a normal DXA. A national consensus guideline for the management of OP that is valid for all specialties is needed. Given the social and health importance of OP, it is essential to implement programs for the continuing education of primary care in this field. National consensus guidance is needed for the management of OP, which should contain recommendations for the appropriate use of case selection tools such as FRAX® and DXA, as well as treatment.
Ethical ResponsibilitiesProtection of people and animalsThe authors declare that the performed procedures conformed to the ethical standards of the committee responsible for human experimentation and were in accordance with the World Medical Association Declaration of Helsinki.
Data confidentialityThe authors declare that they have followed the protocols of their workplace regarding the publication of data from patients and all patients included in the study have received sufficient information and gave their written informed consent to participate in this study.
Right to privacy and informed consentThe authors have obtained informed consent from patients and/or subjects referred to in the article. This document is in the possession of the corresponding author.
Conflict of InterestThe study was supported by the Association for Research in Rheumatology at the Marina Baixa (AIR-MB).
CANAL Group: Canary Islands: Antonio Naranjo, Soledad Ojeda, Ana Bilbao, Fabiola Santana (S. Rheumatology, Hospital Dr. Negrin). Villajoyosa: Jose Rosas, Esteban Salas, José Miguel Senabre-Gallego, Gregorio Santos-Soler, Catherine Cano (S. Rheumatology, Hospital Marina Baixa), Carlos Santos-Ramirez (S. Rheumatology, Hospital Marina Alta. Denia), Xavier Barber (Operations and Research Center of the Miguel Hernández University, Elche), Mabel Sánchez-Barrioluengo (WIT [CSIC-UPV], Polytechnic University of Valencia).
The names of the members of the CANAL group are listed in Annex 1.
Please cite this article as: Naranjo A, et al. Manejo de la osteoporosis en atención primaria antes y después del resultado de la densitometría; tratamiento instaurado versus tratamiento recomendado en los consensos (estudio CANAL). Reumatol Clin. 2013;9:269–273.