Systemic mastocytosis (SM) is a clonal disease of mast cell progenitors from the bone marrow. The clinical picture varies from asymptomatic forms (indolent) to a highly aggressive form with a very short (mast cell leukemia) survival. Between 28 and 34% of patients with SM are related to bone condition at the time of diagnosis and 16% have symptomatic fractures. The presentation of SM as clinical vertebral fractures in young men is rare. Here, we describe a case of established osteoporosis as the only manifestation of SM.
La mastocitosis sistémica (MS) es una enfermedad clonal de los progenitores mastocíticos de la médula ósea. El cuadro clínico varía desde una forma asintomática (indolente) hasta una forma altamente agresiva con una supervivencia muy corta (leucemia de mastocitos). Un 28-34% de los pacientes con MS tiene síntomas relacionados con la afección ósea en el momento del diagnóstico y el 16% fracturas. La presentación de MS como fracturas vertebrales clínicas en varones jóvenes no es frecuente. A continuación describimos un caso de osteoporosis establecida como única manifestación de MS.
Systemic mastocytosis (SM) was reported by Ellis in 1949 as an abnormal proliferation of mast cells infiltrating the skin, bone marrow, liver, spleen, alimentary canal and lymphatic nodes. It is an uncommon disease that occurs in adults, with a slight predominance of men. The clinical manifestations are variable, and develop as a consequence of the infiltration of organs and tissues by mast cells and the release of biochemical mediators.1 The diagnosis of SM is established when 1 of the major criterion and 1 of the minor ones are met, or if 3 minor criteria coexist (Table 1). Once the diagnosis is reached, the percentage of infiltration of mast cells into the bone marrow indicates whether or not the patient has mast cell leukemia (≥20% of infiltration). If the infiltration is less than 20%, and there is no evidence of the findings listed under B or C (Table 1), the disorder is indolent mastocytosis; if only those reported under B are detected, the diagnosis is SM; and, in the presence of those listed under C, we are speaking of aggressive SM.2,3
| Diagnostic criteria (laboratory) | |
| Major | Presence of mast cell (MC) clusters (>15 mast cells) in the biopsy of bone marrow or other tissues |
| Minor | •>25% MC with abnormal morphology in the bone marrow extension •Expression of CD25 or CD2 antigen detected by flow cytometry •Serum tryptase >20ng/mL (not valid if there is an associated myeloid hematologic disease) •Presence of a c-Kit activating mutation in MC of bone marrow or other tissues |
| Mastocytosis is considered to be systemic if a mayor and a minor criterion are met, or 3 minor criteria coexist | |
| Severity criteria (clinical) | |
| B manifestations | Indicative of a high tumor burden and expansion of the genetic defect to several myeloid cell lines •Bone marrow/extracutaneous mastocytosis >30% with serum tryptase <200ng/mL •Hypercellular bone marrow with loss of lipid material, subtle signs of dysmyelopoiesis in the absence of cytopenia, or the World Health Organization criteria for myelodysplastic or myeloproliferative syndrome. •Organomegaly: palpable hepatomegaly/splenomegaly or lymphadenopathy >2cm according to images, with no evidence of functional involvement. |
| C manifestations | Indicative of organic functional changes owing to the infiltration •Cytopenia: neutrophils <1000/μL, platelets <100,000/μL, hemoglobin <10g/dL •Hepatomegaly with ascites and an alteration in liver function •Palpable splenomegaly with hypersplenism •Malabsorption syndrome with hypoalbuminemia and weight loss •Severe osteolytic or osteoporotic lesions with pathological fractures •Enlargement of diverse organs with critical risk due to mast cell infiltration |
Bone disease in mastocytosis is related to the infiltration of the bone marrow by mast cells, and is detected in 70% of the cases. The release of histamine by the mast cells induces sclerosis, a fact that explains the presence of osteoblastic lesions, and the release of heparin and of prostaglandins induces lysis. This means that the differential diagnosis must include other processes such as myelofibrosis, Paget's disease, bone metastasis or fluorosis, in the case of blastic lesions, or cystic fibrosis-related osteoporosis, thalassemia or Gaucher disease in lytic lesions. The most common bone involvement consists of trabecular osteoporosis (OP). The bone changes have an extensive clinical variability, from asymptomatic alterations that often go unnoticed, to more aggressive presenting symptoms, with multiple vertebral fractures,4 as in the case we report.
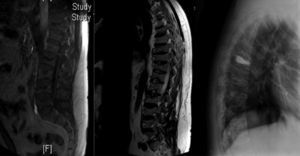
Clinical ObservationThe patient was a 40-year-old man with nothing remarkable in his medical records. He was admitted in July 2013 with a 1-week history of intense thoracic back pain. The radiological study revealed the presence of multiple signs of vertebral compression (Fig. 1). Bone densitometry measured by dual energy X-ray absorptiometry confirmed the presence of lumbar OP (T-score −3.37). Causes secondary to OP in men (hepatitis C virus, hypogonadism, hyperparathyroidism, etc.) were ruled out, as were lymphoproliferative disorders and other tumorigenic processes. The patient required vertebroplasty in thoracic 7 due to thoracic back pain refractory to opioids (Fig. 1); at that time the decision was made to initiate treatment with subcutaneous teriparatide. Given the negative findings in the extensive study performed, we found serum tryptase levels that were persistently high (around 53.9μg/L [normal, 5.5–13.5]). A bone marrow aspirate and biopsy were consistent with mastocytosis. Cytometry detected a mast cell concentration of 0.13%, 99.5% of which were activated, and 0.5% expressed CD25. The c-Kit D816V mutation (A7176T), detected in whole bone marrow, was restricted to mast cells (TaqMan).
Magnetic resonance image of the thoracolumbar spine: a decrease can be seen in the thoracic and lumbar vertebral body height. Thoracic 7 vertebral body is notably diminished in height and presents an alteration in signal intensity. There are similar changes, although less marked, in the upper borders of thoracic 11 and lumbar 2. Lateral radiograph of the thoracic spine: vertebroplasty in thoracic 7.
Once the diagnosis of SM had been confirmed (24 months after the first vertebral fractures), the patient underwent 2 years of teriparatide therapy, and we opted for continuing with an antiresorptive agent (denosumab every 6 months). Although his bone mineral density did not get worse, he had additional vertebral compression fractures. Starting in July 2015, with the diagnosis of indolent SM, treatment with disodium chromoglycate was begun and, to date (December 2015), he has had no new fractures.
DiscussionAs the risk of OP and fractures in SM is high, especially among men,4 routine measurement of bone mineral density and morphometric study are recommended in these patients. Systemic mastocytosis can appear in an indolent form, with no cutaneous or organ manifestations and, thus, the diagnosis is not suspected. We report the case of a young healthy man who had had several vertebral compression fractures in the absence of traumatic injury. He had risk factors for OP, and secondary causes had been ruled out. The diagnosis was idiopathic osteoporosis, although the diagnosis of SM was not discovered for years as there were no compatible symptoms. For this reason, we consider that SM should be included in the diagnostic study of OP in adults in whom an identifiable cause or risk factors are not detected.
At the present time, the most adequate treatment according to histomorphometric studies seems to be antiresorptive therapy; however, although the bone mass increases, certain patients are still at risk for fractures.
ConclusionsSystemic mastocytosis is more common than we actually detect in clinical practice. Even in patients with cutaneous mastocytosis, the average time between the onset of symptoms and the diagnosis is 1 year. In the absence of clinical signs, SM should be suspected in men with OP and in patients with osteoblastic or osteolytic bone lesions of unknown origin. In these cases, repeatedly high serum tryptase levels make it possible to identify patients who should undergo a bone marrow study, to provide early support in the definitive diagnosis.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of InterestThe authors declare they have no conflicts of interest.
Please cite this article as: Carrasco Cubero C, Chamizo Carmona E. Fracturas vertebrales múltiples en varón joven como primera manifestación de una mastocitosis sistémica. Reumatol Clin. 2017;13:107–109.