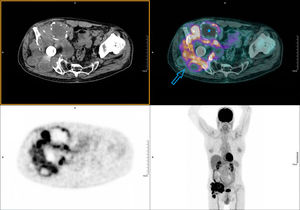
We present the case of a 66-year-old patient, recently diagnosed with bladder carcinoma after a haematuria study, with a picture of lameness and a painless right groin mass, of hard consistency on palpation. As personal background, we highlight a total right hip arthroplasty a few years ago due to severe osteoarthritis. The AP bilateral hip X-ray showed significant bone destruction of the right coxofemoral joint (Fig. 1). In light of these findings, an 18F-FDG PET CT was performed as an extension study of the primary bladder neoformative process, with the possibility of metastatic bone involvement. In the images at 60min post-injection of 18F-FDG a large mass of hypermetabolic multi-lobed soft tissue was observed in the right iliac region, which included the prosthetic material and produced lysis of the iliac wing, with significant destruction of the coxofemoral joint (Fig. 2). A biopsy was performed in view of the findings indicating malignancy, the result was particle disease due to wear and tear of the arthroplasty components. The patient refused surgical revision and is currently undergoing regular follow-up.
PET-CT performed 60min following intravenous administration of 200.14MBq 18F-FDG. Emission and attenuation-corrected images with low-dose CT, from skull vault to upper third of the thighs (whole body protocol). A hypermetabolic mass in the right iliac region, multi-lobed, of approximately 15×13cm and high uptake intensity (SUVmax 14.64). It encompasses the prosthetic material of the hip and extends cranially towards the iliac muscle, causing bone destruction of the iliac wing, the coxofemoral joint and the ischium (arrow). Ametabolic zones are associated indicative of a necrotic/cystic component (star).
The particles produced by the friction mechanism of the prosthesis migrate to the prosthesis-bone interface and produce a biological response that causes linear or rounded areas of osteolysis, similar to tumour or infectious processes, leading to loosening and displacement of the prosthesis.1 Macrophages are the cells responsible for the recognition of these particles and the production of pro-inflammatory cytokines that lead to the activation of osteoclasts, which are responsible for periprosthetic bone resorption. This hyperosteoclastogenesis induced by joint implant degeneration products constitutes the most common mechanism of failure of arthroplasties after 10 years, with few cases before this time.2,3 Radiographic evidence of periprosthetic bone loss is a slow process and infrequent under 5 years following implantation. Therefore, it is recommended that patients are periodically evaluated by radiological study (especially at 5–8 years) to rule out subclinical periprosthetic osteolysis.3 It is essential to know the physiopathology and morphological-functional characteristics of this entity, which produces a local inflammatory state that is difficult to distinguish from aggressive processes.1–3
Total joint replacement is the optimal therapeutic strategy for patients with late-stage osteoarthritis of the hip or knee.1–4 Preoperative (radiological severity, comorbidities, disability, educational level), perioperative (length of stay in hospital, place of discharge) and postoperative (complications) determinants have been identified that contribute to assessing the improvement of pain and functional quality of life, and that facilitate health economic analyses in the field of osteoarthritis.4
AuthorsManuscript concept and design: Elena Espinosa Muñoz.
Data collection: Elena Espinosa Muñoz.
Data analysis and interpretation: Elena Espinosa Muñoz, Antonio Luis Gutiérrez Cardo, Carmen Puentes Zarzuela.
Writing, review and approval of the manuscript: Elena Espinosa Muñoz, Antonio Luis Gutiérrez Cardo, Carmen Puentes Zarzuela.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Espinosa Muñoz E, Gutiérrez Cardo AL, Puentes Zarzuela C. Osteólisis periprotésica por micropartículas que simula un proceso tumoral en cadera derecha en estudio 18F-FDG PET/TC. Reumatol Clin. 2021;17:425–426.