This article presents evidence and recommendations regarding the efficacy and safety of the approved and available therapies in Mexico to treat severe or established osteoporosis (OP) with the aim of developing a position regarding therapeutics in this stage of the disease, according to the descriptive cards of the National Drug Formulary of the National General Health Council of Mexico (CBCMSS).
MethodsWe performed a systematic and narrative review of the evidence of teriparatide and denosumab, from their pharmacological profile, effectiveness, and safety derived from clinical trials, as well as an analysis of the general recommendations of the national and international clinical practice guidelines.
ResultsThe evidence establishes that teriparatide and denosumab belong to different therapeutic classes, with biologically opposed mechanisms of action and indications of use, which are clearly differentiated in their respective national codes, therefore these drugs cannot be substitutable or interchangeable in severe OP therapy. Both represent the best options currently available for this stage of the disease; being similar in their efficacy in preventing new vertebral fragility fractures, with an RR of .35 (CI = 95%, .22−.55) for teriparatide, and .32 (CI = 95%, .26−.41) for denosumab. The absolute risk reduction (RRR) is higher with teriparatide 9.3% (21 months) compared with denosumab at 4.8% (36 months).
ConclusionsOur results agree with the recommendations available in national and international clinical practice guidelines, with both therapies proposed as a sequential, but not a substitute, treatment.
El presente artículo muestra la evidencia y recomendaciones al respecto de la eficacia y seguridad de las terapias hasta hoy aprobadas y disponibles en México para el tratamiento de la osteoporosis (OP) en su etapa severa o establecida, con la finalidad de establecer una postura terapéutica acerca de la eficacia y seguridad para esta etapa del padecimiento, de acuerdo a las cédulas descriptivas del Cuadro Básico y Catálogo de Medicamentos del Sector Salud en México (CBCMSS).
MétodosSe realizó una revisión sistemática y narrativa de la evidencia de teriparatida y denosumab, desde su perfil farmacológico, efectividad y seguridad derivada de ensayos clínicos, además de un análisis de las recomendaciones generales de las principales guías de práctica clínica nacionales e internacionales.
ResultadosLa evidencia establece que teriparatida y denosumab pertenecen a clases terapéuticas distintas, con mecanismos de acción biológicamente opuestos e indicaciones de uso claramente diferenciadas en sus respectivas cédulas, por lo cual no son sustituibles o intercambiables en la terapia de OP severa. Ambas representan la mejor opción disponible hasta el momento para esta etapa del padecimiento; siendo similares en su eficacia de prevención de nuevas fracturas vertebrales por fragilidad, con un RR de 0,35 (IC = 95%, 0,22−0,55) para teriparatida, y de 0;32 (IC = 95%, 0,26–0,41) para denosumab. La reducción absoluta del riesgo (RRR) es mayor con teriparatida 9,3% (21 meses) en comparación con denosumab 4,8% (36 meses).
ConclusionesNuestros resultados concuerdan con las recomendaciones disponibles en las principales guías de práctica clínica nacionales e internacionales, siendo propuestas ambas terapias como consecutivas y nunca sustitutivas.
Osteoporosis (OP) is currently a public health problem due to fracture occurrence and impaired quality of life in patients worldwide.1,2 The stages include severe or established OP, defined by the World Health Organization as the presence of a previous fracture and a bone densitometry (BMD) 2.5 SD or more below the mean value, measured by DXA.3 The prevalence of OP and fractures increases with age: 20% in the population aged 50–59 years; 46% in the population aged 60–69 years; 59% in the population aged 70–79 years and 69% in the population aged >80 years.4 Vertebral and hip fractures have a major influence on mortality rates.5,6 Globally, the economic impact of these fractures is significant.7 In Mexico, the direct cost of more than 75,000 fragility fractures was estimated at 256.2 million dollars in 2010, and a real growth of 41.7% is expected in this area for 2020.8
There are 2 pharmacological approaches in the treatment of patients with OP aimed at reducing the risk for fracture:9 anabolic treatment, which stimulates bone formation, and anti-resorptive treatment, which decreases bone resorption.10,11 There are several drug therapy options in the 2016 edition of the Basic Table and the Catalogue of Health Sector Drugs in Mexico (CBCMSS), drawn up by the General Health Council, a constitutional collegiate body and the highest health authority in the country,12 which include bisphosphonates, calcitriol and calcitonin in the first line. However, in the event of first-line treatment failure or if the patient has severe OP, second line drugs are indicated.
Therapeutic failure is characterized as: 1) presenting 2 or more incident fragility fractures; 2) presenting an incident fracture and high baseline serum levels of β-carboxy-terminal telopeptide of collagen type I (βCTX) or N-terminal propeptide (PINP) of type I without significant reduction during treatment, a significant decrease in BMD or both and 3) presenting non-significant reduction in βCTX or PINP and significant decrease in BMD.13
Currently, in Mexico only teriparatide and denosumab are the drugs whose descriptive card in the CBCMSS shows that they are indicated in patients with severe OP or those with therapeutic failure to first-line agents. In the CBCMSS, teriparatide is a hormone with anabolic activity that belongs to group 5 (endocrinology and metabolism) and is indicated for women and men with OP with previous hip or spinal fractures, high risk of refracture and who have not responded to treatment with calcitriol or bisphosphonates. Denosumab is a monoclonal antibody that also belongs to group 5, and group 17 (oncology) as well, and is indicated in postmenopausal women who are intolerant to oral bisphosphonates, with previous fracture or with a high risk for fracture.12 The present paper, therefore, will focus exclusively on these 2 drugs.
The objective of this article was to perform a systematic and narrative review of the evidence on these drugs, as well as a pharmacological comparison of efficacy, effectiveness, and safety between teriparatide and denosumab and to analyse the recommendations established for severe OP in national and international treatment guidelines. This document includes the position of 3 societies in this regard: The Bone and Mineral Metabolism Association, the Mexican College of Orthopaedics and Traumatology and the Mexican College of Rheumatology.
MethodsFor the pharmacological review of the drugs, the differences in the mechanisms of action, pharmacokinetics, pharmacodynamics and safety and tolerability profile a specialist review was undertaken in 2 platforms, Micromedex®, Truven Health Analytics,14 and the VigiBase®,15 platform, which is the World Health Organization's global database for reporting adverse reactions for both drugs.
For the analysis of effectiveness, efficacy and safety, a systematic review of the literature was conducted, focusing on a search for randomised clinical trials of both drugs, compared with placebo or another molecule using the following terms: Severe osteoporosis/established osteoporosis (teriparatide/denosumab); Severe osteoporosis denosumab or teriparatide; Severe osteoporosis and teriparatide or denosumab, in the following: PubMed, Cochrane Library and TripDatabase (until 2017). Two investigators undertook screening by title, abstract and full text in parallel and independently, and discrepancies were resolved with the intervention of a third investigator.
The inclusion criteria were in accordance with the acronym PICO. Population: adult females diagnosed with OP receiving drug treatment. Interventions: teriparatide or denosumab, under their approved dosage and application regimens. Comparators: compared with placebo. Measurement of fracture outcomes (by anatomical site) and adverse events leading to discontinuation of the study. The methodological quality was evaluated by applying the criteria of the Spanish version of the Critical Appraisals Skills Programme (CASPe).16
Finally, the clinical practice guidelines and national consensuses: CENETEC 2013,9 AMMOM 2015,17 Interdisciplinary Groups 201518 and CENAPRECE 2017,19 and international institutions such as ESCEO/IOF Europe 2013,20 NOGG UK 2017,21 NICE updated 2010 and 2017,22 Haute Autorité de Santé France 2014,23 AACE/ACE USA 201624 were considered for analysis of the recommendations on therapy for severe OP.
ResultsPharmacological comparisonTeriparatide is a synthetic polypeptide hormone made up of the first 34 amino acids of human parathyroid hormone (PTH),25 which give it its biological activity, 26 mimicking the actions of endogenous PTH, resulting in a catabolic effect on bone. However, when administered in low doses and intermittently, it results in anabolic properties in the bone system.27–30 Administered by subcutaneous injection of 20 μg once a day, serum concentrations peak at 30 min and decrease to undetectable levels after 3 h. The bioavailability of teriparatide is 95% on average, with a one-hour half-life, with elimination of 62 L/h in women and 94 L/h in men. Elimination occurs by non-specific enzymatic mechanisms in the liver, followed by its excretion via the kidneys (Table 1).25
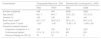
Main pharmacological differences between teriparatide and denosumab.
| Pharmacology | Teriparatide | Denosumab |
|---|---|---|
| ATC Code | H05AA02 - Teriparatide | M05BX04 - Denosumab |
| H-Systemic Hormone Preparations | M-Musculo-skeletal system | |
| H05-Calcium homeostasis | M05-Drugs used for the treatment of bone diseases | |
| H05A-Parathyroid hormones and analogues | M05B-Drugs affecting bone structure and mineralisation | |
| H05AA-Parathyroid Hormones and analogues | MB05BX-Other drugs affecting bone structure and mineralization | |
| Structure | ||
| Polypeptide chain | Monoclonal antibody | |
| Molecular weight | 4,117.7 Daltons | 144,700.0 Daltons |
| Description | Synthetic polypeptide hormone comprised of amino acids 1–34 of the human parathyroid hormone (HPT). It is the biologically active N-terminal region of PTH | Fully human IgG2 monoclonal antibody specific to RANKL (nuclear factor kappa-B ligand) |
| Dose | 20 μg once a day up to 18 months | 60 mg once every 6 months |
| Route | Subcutaneous | Subcutaneous |
| Pharmacodynamics | ||
| Mechanism of action | Mimics the mechanism of action of PTH, stimulating bone formation by direct effect on osteoblasts and on intestinal absorption of calcium | Specifically binds to RANKL, inhibits the formation of RANKL-RANK complex, and indirectly causes a decrease in the formation and activity of osteoclasts |
| Pharmacokinetics | ||
| Absorption | ||
| Bioavailability (subcutaneous administration) | 95% | 61% |
| Maximum plasma concentration (Cmax) | Approximately 140 pg/mL | 6 μg/mL (range from 1–17 μg/mL) |
| Time to Cmax (Tmax) | 20−30 min | 10 days (range from 2 to 28 days) |
| Distribution | ||
| Binding to proteins | Yes. It is assumed that it is transported in the same way as parathyroid hormone (PTH), through the alpha-globulin fraction | Not available, although it is considered that behaviour is the same as other monoclonal antibodies which do not bind to proteins |
| Volume of distribution (Vd) | 1 L/kg (intravenous) | No values are indicated; however, it has been mentioned that extravascular distribution decreases |
| Metabolism | ||
| Site of metabolism | Hepatic | Metabolism could be mediated by 3 mechanisms: |
| It is assumed that it is metabolised in the same way as PTH, through proteolytic liver enzymes | a) Proteolysis by the liver and by the reticuloendothelial system | |
| b) Elimination mediated by markers | ||
| c) Non-specific endocytosis followed by intracellular degradation. In this type of mechanism there can be protection of the Fc portion, causing increased half-life time | ||
| Excretion | ||
| Renal clearance | 90% | Due to its molecular weight, denosumab is not excreted in the urine, it is metabolised to peptides and amino acids, which can be reused for de novo protein synthesis |
| Renal clearance like that of PTH is assumed | ||
| Total clearance | Women: 62 L/h Men: 94 L/h | Not available |
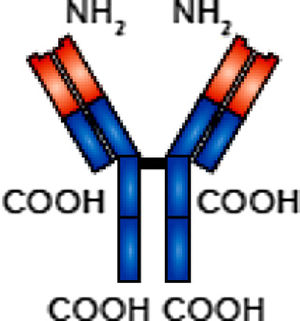
Denosumab is a human monoclonal antibody of recombinant DNA origin that binds to the cytosine RANKL (receptor activator of nuclear factor k B ligand), which prevents its binding to the RANK osteoclast membrane receptors (NFB receptor activator of NFκB). By reducing RANKL-RANK binding, the formation of the mature osteoclast is inhibited thus promoting decreased bone resorption.31–33 With these characteristics, the effect of osteoprotegerin, which is fundamental for bone resorption capacity, is simulated.34 After a subcutaneous dose of 60 mg, bioavailability is 61%, maximum serum concentration (Cmax) is 6 μg/mL (range 1–17 μg/mL) in an average of 10 days (range 2–28 days), with a half-life of 26 days (range 6–52 days) (Table 1).35
Main pharmacological differences between teriparatide and denosumabThere are significant differences between the two agents at all levels of classification according to the Anatomical, Therapeutic, Chemical (ATC) Classification System.36 With pharmacokinetic and pharmacodynamic properties that differ radically from each other in terms of pharmacophore, biological, mechanistic, and chemical activity (Table 1).
Safety and tolerability profileSafety can be determined by the frequency and severity of adverse reactions. In the case of denosumab, adverse events reported for the therapeutic indications for this drug are included, not only OP studies. The most frequent adverse reactions to denosumab include constipation, sciatica, exanthem rashes, limb pain, cataracts, among others. Mention should be made of mandibular osteonecrosis (1%–2%) and associated atypical fractures (case series report), serious events that warrant discontinuation of treatment.37–39 The most frequent adverse reactions to teriparatide include nausea, limb pain, dizziness and hyperuricaemia.25,35 Specialist consultation in Micromedex,® finds differences and similarities in the safety and tolerability of each of these drugs (Table 2).14 When assessing adverse reactions reported in VigiBase® up until May 2017, 95,175 adverse reaction reports were made over the last 27 years for teriparatide, and 50,680 for denosumab over a period of 14 years.
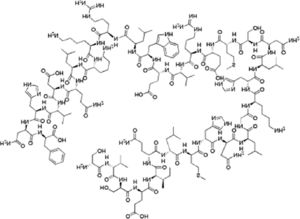
Description of adverse reactions reported per system, for teriparatide and denosumab.
| Teriparatide | Denosumab |
|---|---|
| Cardiovascular effects: angina pectoris (2.5%), hypertension (7.1%), hypotension (case report) and orthostatic hypotension (5%) | Cardiovascular effects: angina pectoris (2.6%), endocarditis (case report), hypertension (6.4%), peripheral oedema (24% in hypercalcaemia of malignancy and 4.9% in osteoporosis) |
| Dermatological effects: pain at injection site, erythema, rash, and hives (unknown incidence) | Dermatological effects: cellulitis (.4%), dermatitis (4.2%–10.8%), erysipelas (case report), reactions at injection site (3%), pruritus (2.2%), rash (2.5%–5.1%) |
| Endocrine and metabolic effects: hypercalcaemia (11%), hypocalcaemia (case report), hypoparathyroidism (case report) and hyperuricaemia (3%) | Endocrine and metabolic effects: hypercalcaemia (unknown incidence), hypercholesterolaemia (7.2%), hypermagnesaemia (3%), hypocalcaemia (1.7%–18%), hypopotassaemia (3%), hypophosphataemia (32%−76%) |
| Gastrointestinal effects: nausea (8.5%) | Gastrointestinal effects: constipation (21%), loss of appetite (24%), dental abscess (.3%), diarrhoea (21%), flatulence (2.2%), gastro-oesophageal reflux (2.1%), nausea (4.3%), pancreatitis (.2%–.8%), abdominal pain (3.3%), vomiting (15%–24%) |
| Immunological effects: development of antibodies (3%) | Haematological effects: anaemia (3.3%) |
| Musculo-skeletal effects: arthralgia (10.1%), leg cramp (2.6%), spasm (1%–10%) | Immunological effects: anaphylaxis (case report), antibody development (less than 1%), herpes zoster (2%), hypersensitivity reactions (case report), severe infections (4%) and influenza (8%) |
| Neurological effects: dizziness (8%), depression (4%) | Musculo-skeletal effects: arthralgia (6.7%–14.3%), aseptic necrosis (1.8%), back pain (8.3%–34.7%), bone pain (3.7%), bone fracture (3.8%), musculo-skeletal pain (6%–7.6%), myalgia (2.9%), osteomyelitis (.7%), pain in extremities (9.9%–11.7%) and spondylosis with myelopathy (2.1%) |
| Neurological effects: asthenia (2.3%–20%), headache (11%–24%), insomnia (3.2%), sciatica (4.6%) and vertigo (5%) | |
| Ophthalmic effects: bilateral cataracts (4.7%) | |
| Renal effects: cystitis (5.9%) and urinary tract infections (8%) | |
| Respiratory effects: cough (15%), dyspnoea (21%–27%), nasopharyngitis (6.7%) and pharyngitis (2.3%) | |
| Other: cancer (1.9%–4.8%), fatigue (11%–25%) and fever (6%) |
Source: Based on information from Micromedex®.14.
From the electronic libraries consulted, analysing a total of 411 original references, 2 studies were obtained (kappa .40–.80; P < .0001), both of high methodological quality (10 of 11 CASPe items).
The 2 clinical trials selected are pivotal studies of teriparatide29 and denosumab40: it should be noted that the proportion of patients with prevalent vertebral fracture varied significantly between these studies. The teriparatide study29 included patients with at least one moderate fracture or 2 mild fractures not caused by trauma to the vertebrae,29 while the study of denosumab only included 24% of patients with this characteristic.37,40 Another important difference was that 15%–16% of the patients in the teriparatide study had received previous therapy for unspecified OP,29 but not in the denosumab study. However, the remaining baseline characteristics such as age, sex, body mass index and T score at the lumbar spine were comparable40 (Table 3).
Relevant baseline characteristics in the clinical trials selected.
| Characteristic | Teriparatide Neer et al., 2001 | Denosumab Cummings et al., 2009 | ||
|---|---|---|---|---|
| PBO | TPDa | PBO | DSM | |
| Number of patients | 448 | 444 | 3906 | 3902 |
| Age (years) | 69 ± 7 | 69 ± 7 | 72.3 ± 5.2 | 72.3 ± 5.2 |
| Female (%) | 100 | 100 | 100 | 100 |
| Body mass indexb | 26.7 ± 4.7 | 26.8 ± 4.2 | 26.0 ± 4.1 | 26.0 ± 4.2 |
| Lumbar spine T-score | −2.6c | −2.6c | −2.82 ± .70 | −2.84 ± .69 |
| Prevalent vertebral fracture | ||||
| Proportion of patients in % | 100 | 100 | 23.4 | 23.8 |
| Fractures per patient | 2.3 ± 1.8 | 2.3 ± 1.8 | NR | NR |
| Previous therapy for OP (%) | 15 | 16 | 0 | 0 |
DSM: Denosumab; NR: Not reported; OP: Osteoporosis; PBO: Placebo; TPD: Teriparatide.
Data reported that include the ± symbol, indicate mean (left) and standard deviation (right).
The primary measure of efficacy in both studies was a statistically significant reduction in the occurrence of vertebral fragility refracture (Table 4). Comparison against placebo showed an RR of .35 (95% CI: .22−.55) for teriparatide and .32 (95% CI: .26−.41) for denosumab. The absolute risk reduction (ARR) was higher with teriparatide than with denosumab (9.3% vs 4.8%), although the follow-up time was shorter in the teriparatide study (21 months) than in the denosumab study (36 months).29,40
Comparison of efficacy to prevent vertebral and non-vertebral fragility fractures.
| Drug | Population | TPD (N = 444) | PBO (N = 448) | RAR | RR (95% CI) | P |
|---|---|---|---|---|---|---|
| Teriparatide (Neer et al., 2001) | Women with vertebral fracture | 22 (5.0%) | 64 (14.3%) | 9.3% | .35 (.22−.55) | ≤ .001 |
| TPD (N = 541) | PBO (N = 544) | RAR | RR (95% CI) | P | ||
| Women with non-vertebral fracture | 14 (2.6%) | 30 (5.5%) | 2.9% | .47 (.25−.88) | .02 | |
| Denosumab (Cummings et al., 2009) | Population | DSM (N = 3702) | PBO (N = 3691) | RAR | RR (95% CI) | P |
| Women with vertebral fracture | 86 (2.3%) | 264 (7.2%) | 4.8% | .32 (.26−.41) | < .001 | |
| DSM (N = 3.902) | PBO (N = 3906) | RAR | HR (95% CI) | P | ||
| Women with non-vertebral fracture | 238 (6.5%) | 293 (8.0%) | 1.5% | .80 (.67−.95) | < .001 |
ARR: Absolute Risk Reduction; DSM: Denosumab; PBO: Placebo; RR: Risk Ratio or Relative Risk; TPD: Teriparatide.
Follow-up times: teriparatide study (21 months), denosumab study (36 months).
Occurrence of non-vertebral fragility fractures was a secondary measure of efficacy in both studies (Table 4).29,40 In both cases a significant reduction in their incidence was achieved, although the point estimate varied significantly: RR .47 (95% CI: .25−.88) with teriparatide and HR .80 (95% CI: .67–.96) with denosumab. This implies that teriparatide reduced the incidence of non-vertebral fragility fractures by 53%, while the reduction obtained with denosumab was 20%. The ARR was also higher with teriparatide than with denosumab (2.9% vs. 1.5%). Another difference to consider is that the risk estimates in the denosumab study come from a Kaplan-Meier analysis,40 while those corresponding to teriparatide are simple proportions.29 Denosumab showed a reduction in the risk for fragility hip fracture of HR .60 (95% CI .37–.97). The teriparatide study indicates that the number of non-vertebral fragility fracture events, not anatomical site-specific, was too low to precisely estimate their incidence, and that the point estimate of RR for hip fracture compared to placebo was .25, which represents a reduction of 75%.29
The two studies categorised adverse events differently, although they had in common the classification of adverse events leading to discontinuation of therapy, shown in Table 5. As can be seen, the point incidences are similar between both agents and in neither of the 2 cases were the differences statistically significant.
Comparison of incidence of adverse events leading to discontinuation of therapy.
| Reference: Neer et al. 2001 | TPD (N = 541) | PBO (N = 544) | RR (95% CI) | P |
|---|---|---|---|---|
| Women with fractures | 35 (6.5%) | 32 (5.9%) | 1.10 (.69−1.75) | .688 |
| Reference: Cummings et al. 2009 | DSM (N = 3886) | PBO (N = 3876) | RR (95% CI) | P |
|---|---|---|---|---|
| Women with fractures | 192 (4.9%) | 202 (5.2%) | .95 (.78−1.15) | .55 |
Adverse effects defined as those leading to discontinuation of the therapy under study.
DSM: Denosumab; PBO: Placebo; RR: Risk Ratio or Relative Risk; TPD: Teriparatide.
Follow-up times: teriparatide study (21 months), denosumab study (36 months).
The 4 guidelines consulted clearly distinguish the mechanisms of action of both agents, defining teriparatide as osteoforming and denosumab as anti-resorptive. They all emphasize that teriparatide should be administered in high-risk populations, such as women with OP and those with previous fractures, i.e., with severe OP. For denosumab, the recommendation is that it should be used in women who are not candidates for first-line drugs. All recommendations agree on the need for subsequent treatment after discontinuation of teriparatide or denosumab (Table 6).
Summary of main national and international clinical practice guidelines: Information in postmenopausal women.
| Preparation; year of publication | Comments or recommendations on teriparatide | Comments or recommendations on denosumab |
|---|---|---|
| CENETEC, 2013 | • It is a good therapeutic option in patients with previous vertebral fractures | • It is a new therapeutic option for the treatment of post-menopausal osteoporosis, when the patient is not a candidate for first-line drugs |
| • It is important to consider continuing treatment with bisphosphonates after discontinuation of 2-year treatment with teriparatide, since the effect on reducing the risk for vertebral fractures is lost | ||
| AMMOM, 2015 | • It is an osteoforming treatment, indicated in women with postmenopausal OP at high risk for fracture, with multiple fractures, in those who do not tolerate other types of treatment or with no response | • It is an anti-resorptive treatment |
| • Other treatment options are necessary when teriparatide is discontinued | • The anti-resorptive action is rapid at the start of treatment and this effect is also quickly lost when treatment is discontinued | |
| • The main side effect is hypercalcaemia | • Skin infections have been reported in some patients, as a major side effect | |
| Interdisciplinary groupa, 2015 | • It is an osteoforming treatment, indicated in postmenopausal women with OP, with a high risk of fractures, simple or multiple, intolerance to other treatments or who have not had a satisfactory response | • It is an anti-resorptive treatment |
| • Additional options are necessary after treatment has been discontinued | • The anti-resorptive action is rapid at the start of treatment and this effect is also quickly lost when treatment is discontinued | |
| • The main side effect is hypercalcaemia | • Skin infections have also been reported as side effects | |
| CENAPRECE, 2017 | • Osteo-forming mechanism | • Anti-resorptive mechanism, activated through different routes than the bisphosphonates |
| • Indicated in the treatment of men and women with OP with previous fracture, at high risk of refracture and those who do not respond to bisphosphonates | • Recommended for use in postmenopausal women who do not tolerate it orally | |
| • Adverse effects: headache, myalgia, hypercalcaemia, hypercalciuria, hyperuricaemia | • Adverse effects: headache, hypocalcaemia, skin manifestations, meteorism | |
| Preparation, year of publication, region/country | ||
| ESCEO/IOF, 2013, Europe | • Evidence for reducing the risk of vertebral (re) fracture in women with severe or established OP (e.g., with previous vertebral fracture) | • Evidence for reducing the risk of vertebral and non-vertebral fractures in a mixed group of osteoporotic women with and without prevalent vertebral fracture |
| • The benefit in non-vertebral fractures persists for up to 30 months after treatment is discontinued | • Effects are particularly marked in patients at high risk for fracture | |
| • The most common adverse events include nausea, lower limb pain, headache, and dizziness | • Mandibular osteonecrosis is a major adverse event | |
| NOGG, 2017, United Kingdom | • It has been shown to reduce vertebral and non-vertebral fractures in post-menopausal women with OP | • It reduces vertebral and non-vertebral fractures, including hip fractures in postmenopausal women with OP |
| • Its high cost restricts its use in women at extremely high risk, particularly of vertebral fracture | • Appropriate alternative in patients who are intolerant to oral bisphosphonates or where first-line treatment is contraindicated | |
| • Use limited to 24 months | ||
| NICE, 2008 (updated in 2017) for teriparatide and 2010 for denosumab, United Kingdom | • Anabolic agent for osteoforming treatment | • Only recommended for postmenopausal women at high risk of fracture: |
| • Approved for women with severe or established OP | Who have contraindications or are intolerant to or unable to receive alendronate, risedronate or etidronate (oral bisphosphonates) | |
| • Recommended for women who are intolerant or have a contraindication for alendronate, risedronate or strontium ranelate or with unsatisfactory response to treatment with alendronate or risedronate and aged ≥65 years with T score of −4.0 or less, or −3.5 or less and more than 2 fractures, or between 55 and 64 years of age, T score of −4 SD or lower and more than 2 fractures | Who have a combination of T score (minimum score −3.0), age (minimum of 65 years) and number of clinical risk factors (none over 70 years, 1 or 2 in other age groups) | |
| Haute Autorité de Santé, 2014, France | • Indicated for women with postmenopausal OP with at least 2 vertebral fractures | • Indicated for women with postmenopausal OP as a second line of post bisphosphonate treatment |
| • Reduces vertebral and non-vertebral fractures | • Reduces vertebral and non-vertebral fractures, including hip fractures | |
| Maximum duration of 24 months | • Several years’ duration | |
| AACE/ACE, 2016, USA | • Osteoforming treatment | • Broad-spectrum anti-resorptive treatment (reduces vertebral and non-vertebral fractures including hip) |
| • Reduces vertebral and non-vertebral fractures. Recommended in patients at high risk of fracture | • Recommended for patients at high risk for fracture | |
| • Maximum duration of 24 months and start anti-resorptive treatment after discontinuation | • Agent of choice in patients with kidney failure | |
| NOF, 2014, USA | • Anabolic agent approved for treatment of postmenopausal OP in women at high risk | • Antiresorptive agent approved for treatment of postmenopausal OP in women at high risk |
| • It is common to administer an anti-resorptive after discontinuing teriparatide | • Pharmacological alternatives should be considered after discontinuation | |
| • Common adverse events include leg cramps, nausea, and dizziness | • Increases the risk for serious skin infections (cellulitis) and can cause hypocalcaemia. Other adverse events (although rare) are mandibular osteonecrosis and atypical fractures. | |
| Toward Optimized Practice, 2016, Alberta/Canada | • Osteoforming therapy approved for the treatment of women with post-menopausal OP | • Anti-resorptive therapy approved for the treatment of women with post-menopausal OP |
| • Reduces vertebral and non-vertebral fractures and helps to reduce the pain associated with vertebral fracture | • Reduces vertebral and non-vertebral fractures, including hip fractures | |
| • Can cause hypercalciuria and hypercalcaemia, although these events are generally mild and transient | • Possible adverse events: mandibular osteonecrosis, atypical fracture, serious infections | |
| Asociación Argentina de Osteología y Metabolismo Mineral y la Sociedad Argentina de Osteoporosis, 2017, Argentina | • Anabolic treatment | • Anti-catabolic treatment (reduces remodelling) |
| • Can be considered a first-choice drug in patients with severe OP and a history of fractures or exceptionally low BMD (T score < −3) in patients > 65 years | • Reduces vertebral, femoral, and non-vertebral fractures | |
| • Can also be used in patients with suboptimal response (fragility fractures or bone loss during treatment) | • Adverse events: skin rash, cellulitis, and possible association with spontaneous fractures | |
| • Adverse events: dizziness, flushing at injection site, headache, nausea, arthralgia, myalgia, lethargy, and weakness | • It may be advisable to continue with a bisphosphonate to avoid a rebound effect after discontinuing denosumab | |
| • The ideal duration of treatment should be reconsidered | ||
| Sociedade Brasileira de Reumatologia, 2017, Brazil | • Anabolic treatment | • Monoclonal antibody used as an anti-resorptive treatment |
| • First line in patients with postmenopausal OP and high risk of fracture or with a history of fragility fracture | • First line in patients with post-menopausal OP and renal dysfunction | |
| • Second line in patients with OP who have failed (e.g., have had a re-fracture) or are intolerant to previous treatments | • Second line in patients with postmenopausal OP where bisphosphonates have failed, are contraindicated, or not tolerated | |
| • Administer another treatment after discontinuation | • Administer another treatment after discontinuation | |
| RACGP, 2017, Australia | • Anabolic agent | • Antiresorptive treatment |
| • Recommended in women with postmenopausal OP who have failed treatment with an anti-resorptive agents or for whom anti-resorptive therapy is contraindicated | • Recommended in women with postmenopausal OP at high risk of re-fracture | |
| • Reimbursed in patients with severe OP at extremely high risk: | • Shown to reduce the risk of vertebral and non-vertebral fractures, including hip fractures | |
| T score ≤ −3 | • Severe adverse events: mandibular osteonecrosis and atypical femoral fracture occurrence | |
| History of 2 or more fragility fractures | ||
| Occurrence of at least one symptomatic fracture after at least 12 continuous months of antiresorptive therapy at adequate doses | ||
| • Adverse events: dizziness, leg cramp, nausea, reactions at injection site and headache |
AACE/ACE: The American Association of Clinical Endocrinologists/American College of Endocrinology; AMMOM: Asociación Mexicana de Metabolismo Óseo y Mineral A.C. (Mexican Association of Bone and Mineral Metabolism); CENAPRECE: Centro Nacional de Programas Preventivos y Control de Enfermedades (National Centre of Preventive Programmes and Disease Control); CENETEC: Centro Nacional de Excelencia Tecnológica en Salud (National Centre for Technological Excellence in Health); ESCEO: European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis; IOF: International Osteoporosis Foundation; NICE: National Institute for Health and Care Excellence; NOF: National Osteoporosis Foundation; NOGG: The National Osteoporosis Guideline Group; OP: osteoporosis; RACGP: The Royal Australian College of General Practitioners.
The main guidelines identified at international level (North America, Europe, South America and Australia21–24,41–45) refer to the difference of both drugs in terms of their mechanisms of action and treatment approach (osteoforming and anti-resorptive). The guidelines consulted recommend teriparatide in patients at high or extremely high risk for fracture, either as first or second line, after failure with anti-resorptive agents or in some cases if there is intolerance. Denosumab is recommended as a first-line alternative in high-risk patients and as agent of choice in patients with renal failure. Most of the authors agree in recommending its use in case of intolerance or contraindication to bisphosphonates (Table 6).
Discussion and conclusionsThe present document summarises the 2 pharmacological treatment approaches for severe OP: teriparatide anabolic (osteoforming) and denosumab catabolic (anti-resorptive). It also summarises the specific indications for their administration in accordance with the CBCMSS descriptive cards, adverse events according to the Micromedex® and VigiBase® platforms and, finally, it summarises the therapeutic indications published in the different national and international guidelines for this entity.
Teriparatide, a synthetic polypeptide hormone, directly stimulates osteoblasts to form new bone; while denosumab, a monoclonal antibody, inhibits osteoclastogenesis. The anti-fracture efficacy of both drugs has been sufficiently proven, but due to their different mechanisms of action, therapeutic interchange or therapeutic substitution are not indicated. The criteria for therapeutic substitution do not apply in the case of 2 drugs belonging to different ATC classes and therefore differing in their pharmacological composition, which can lead to heterogeneous efficacy and safety profiles that are not very comparable.
On the other hand, results of indirect comparisons and network meta-analyses involving pivotal clinical trials of teriparatide and denosumab should be viewed cautiously due to differences in some baseline characteristics of the patients recruited, which are critical (e.g., percentage of women with previous fracture).46,47
Teriparatide is indicated in men and women with severe OP, high risk for refracture, risk for imminent fracture or those who have not responded to treatment with calcitriol or bisphosphonates. Denosumab is indicated for postmenopausal women who are intolerant to bisphosphonates, women with previous fracture and risk of subsequent fractures and for the prevention of bone complications (pathological fractures, bone radiotherapy, spinal cord compression or bone surgery), in patients with breast cancer with bone metastasis and with signs of impaired renal function.12
It is important to note that there is inter-institutional agreement on the criteria and main recommendations issued by national and international clinical practice guidelines. However, there are no data for us to determine the level that physicians adhere to the cards when prescribing.
Both drugs have an acceptable safety profile, as the most frequent adverse reactions are mild and moderate and do not put the patient's life at risk. Although the number of reports of suspected adverse reactions is approximately double for teriparatide (95,175 in 27 years) compared to denosumab (50,680 in 14 years). This could be attributed to the difference in years on the market, together with the emphasis on adverse reaction reporting, especially with innovative products, over the last decade. Finally, we must bear in mind that there are drugs with more adverse reactions per se.
The recommendations issued in national and international guidelines follow a general pattern in terms of the indication of both drugs for treating severe OP in patients with inadequate response to bisphosphonates. However, they cannot be said to be substitutable for the reasons mentioned above. Therefore, their prescription should be individualised and based on the characteristics of the patient, such as age, site of previous fractures, risk profile, previous treatments, and desired effect, to achieve better clinical outcomes.
It is important to highlight that recent research on the sequence of OP treatment in patients with imminent risk for fracture, understood as imminent risk the first year following a vertebral or hip fracture,48 has shown that the use of teriparatide is recommended primarily to build bone mass, followed by transition to denosumab or a bisphosphonate, considering the benefit in BMD gain with this sequence.49,50
One of the strengths of the present study which means we can take a position on the treatment of severe OP is our use of solid literature search methodologies and having consulted reliable databases, and the involvement of specialist researchers in various areas of knowledge, which enabled a comprehensive and multidisciplinary approach.
Given the nature of the summary studies, the main limitation of this work is the inclusion of studies with highly heterogeneous population characteristics. This shortcoming is attributed to the availability of primary studies.
The position of this working group based on the published evidence can be summarised as follows: a) both medicines have high quality evidence according to CASPe and are indicated in the treatment of severe or established OP, b) teriparatide and denosumab belong to different therapeutic classes, with biologically opposed mechanisms of action and clearly differentiated indications for use on their respective CBCMSS descriptive cards, and therefore, c) these medicines are not interchangeable or substitutable in the treatment of severe OP.
FundingThis project was undertaken with an unrestricted grant, number 4100501768 from Eli Lilly & Compañía de México, S.A. de C.V. in which the authors had full autonomy in its development.
This study was carried out by a multidisciplinary group of experts in systematic review methodology and a group of experts in the field. This review was endorsed by the Mexican College of Rheumatology, the Mexican College of Orthopaedics and the Mexican Association of Bone and Mineral Metabolism.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Clark P, Rivera FC, Méndez Sánchez L, Mendoza Gutiérrez CF, Vargas Neri JL, Carrillo Vázquez SM, et al. Osteoporosis severa: fundamentos para su terapia farmacológica en México. Reumatol Clin. 2021;17:97–105.