A 67-year-old woman presented with a 5-year history of mechanical thoracolumbar pain that responded satisfactorily to nonsteroidal anti-inflammatory agents. She had intermittent inflammatory low back pain since the age of 25 years, and 2 episodes of acute anterior uveitis at 30 and 32 years of age, respectively. She had 2 siblings who had been diagnosed as having human lymphocyte antigen (HLA)-B27-positive ankylosing spondylitis (AS). Physical examination revealed limited axial mobility (modified Schöber test: 2.5cm) and chest expansion (2cm), and bilateral positive sacroiliac maneuvers. The results of her analyses were normal (erythrocyte sedimentation rate 16mm/h; C-reactive protein 2.6mg/dL) and she was HLA-B27-positive. Thoracic spine radiographs showed bone bridges on right anterolateral aspect of 4 contiguous vertebrae (Fig. 1) compatible with Forestier-Rotés-Quérol disease, or diffuse idiopathic skeletal hyperostosis (DISH), and, in pelvis, bilateral grade 3 sacroiliitis (Fig. 2A). Computed tomography (CT) of the sacroiliac joints revealed sclerosis and erosions (Fig. 2B and C), confirming the coexistence of AS and DISH.
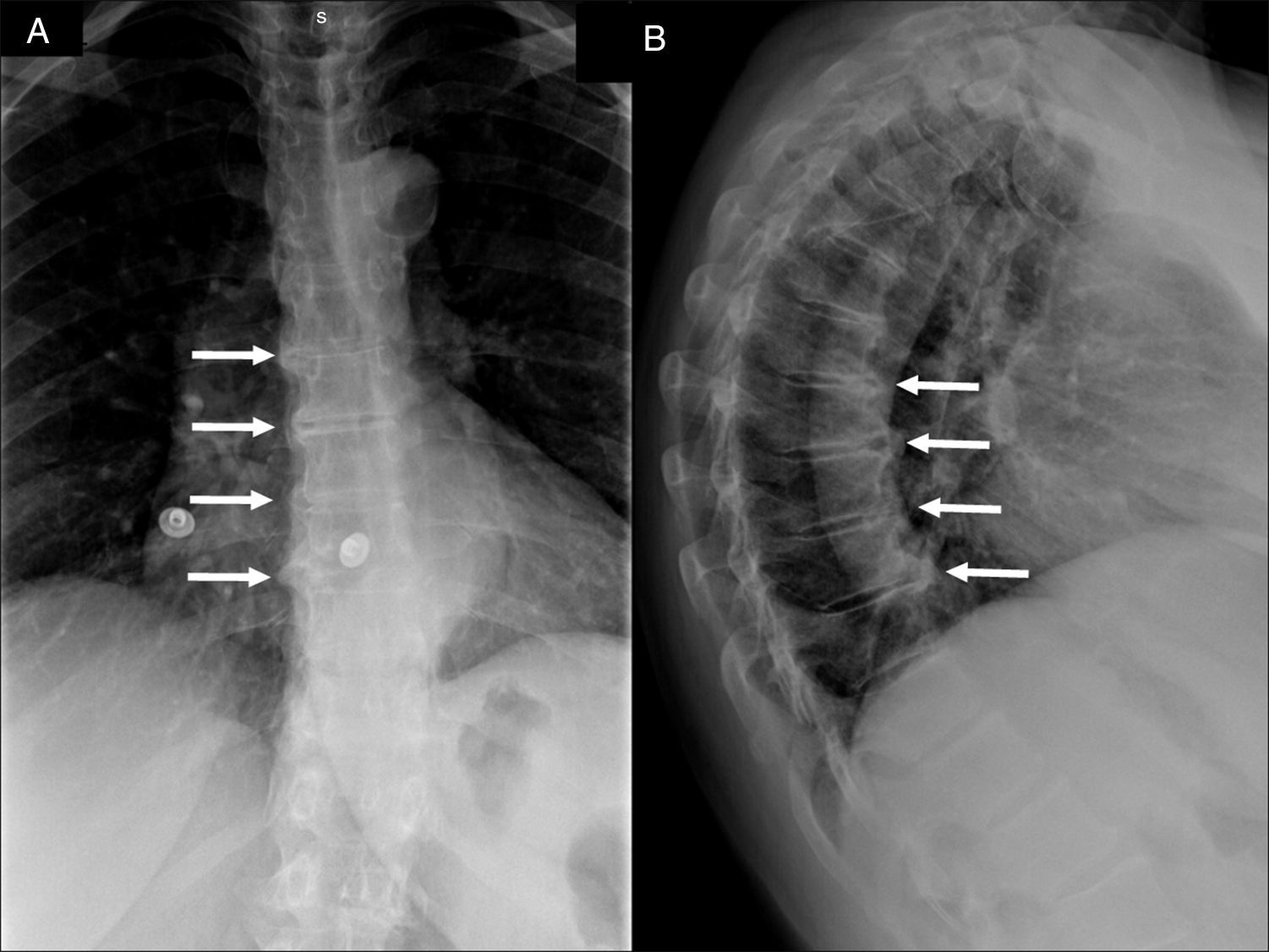
Anteroposterior (A) and lateral (B) radiographs of thoracic spine showing the bone bridges in right anterolateral aspect of 4 contiguous vertebral bodies (white arrows) consistent with the diagnosis of diffuse idiopathic skeletal hyperostosis (DISH). The lateral radiograph also reveals that these bone bridges form angles of more than 45° with the vertebral border.
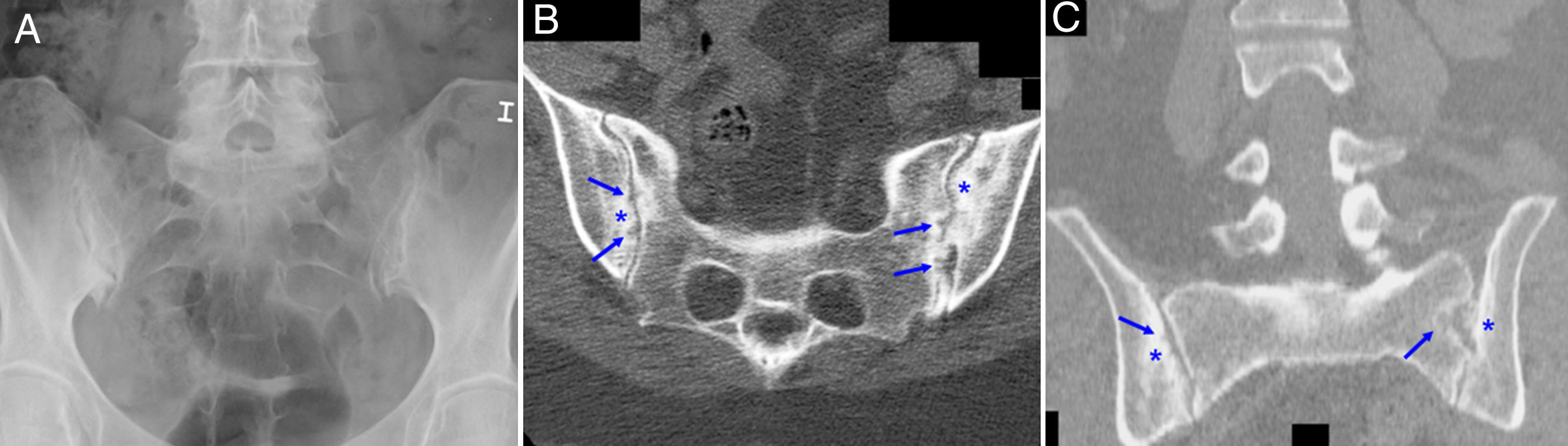
Radiograph of pelvis (A) showing sclerosis, joint space narrowing and erosions in right sacroiliac joint and sclerosis and pseudo-widening on the left (bilateral grade 3 sacroiliitis). Computed tomography of sacroiliac joints showing axial (B) and coronal (C) planes with areas of sclerosis (asterisks) and erosions (arrows) in both joint margins.
Ankylosing spondylitis and DISH have similar rates of new bone formation and functional limitations.1,2 However, AS has an inflammatory basis, develops in individuals of less than 40 years of age, and is associated with HLA-B27 (90%), whereas DISH has a metabolic basis, appears in those over the age of 50, and is not associated with HLA-B27 (8%).3 The type of vertebral bone formation also differs; AS is characterized by “typical syndesmophytes” that are vertical and narrow and originate in the annulus fibrosus, whereas DISH shows bone excrescences that begin in the anterior longitudinal ligament and paravertebral tissues, forming angles >45°.1,4 Diffuse idiopathic skeletal hyperostosis affects the sacroiliac joints in their most cranial portion (ligamentous), with vacuum phenomenon, joint space narrowing, sclerosis and even ankylosis, which can be confused with grade 4 sacroiliitis in plain radiographs (and CT is useful in these cases), but without inflammatory changes or erosions.3,5,6 These 2 disorders are not mutually exclusive and can coexist, although few cases have been reported (16 according to the literature).7–9
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of InterestThe authors declare they have no conflicts of interest concerning the publication of this article.
Please cite this article as: Macía-Villa CC, Sifuentes-Giraldo WA, Medina-Luezas J. Presentación simultánea de espondilitis anquilosante e hiperostosis esquelética idiopática difusa (enfermedad de Forestier-Rotès-Quérol). Reumatol Clin. 2017;13:237–238.