The aim of this study was to conduct a systematic review of the quality of the transcultural adaptation procedure and the clinimetric properties of the self-administered hip-disability functional assessment questionnaires adapted for the Spanish population.
Material and methodWe searched the MEDLINE, EMBASE, CINAHL and Web of Science databases (from inception until June 2016) to locate all the scales adapted to Spanish and to analyse the different phases of the adaptation process and its psychometric properties.
ResultsEight scales were identified, and were grouped into three sections, according to the type of diseases in which they can be used: (a) lower limb: Lower Limb Functional Index (LLFI), Lower Extremity Functional Scale (LEFS) and Arthrosis of Membres Inférieurs et Qualité de vie (AMICAL); (b) knee and/or hip: Western Ontario and McMaster Universities Osteoarthritis (WOMAC) index, Osteoarthritis Knee and Hip Quality of Life (OAKHQOL) and Hip and Knee Questionnaire (HKQ); and (c) specific for hip: Hip Outcome Score (HOS) and International Hip Outcome Tool-33 (iHOT-33). The transcultural adaptation procedure was satisfactory in all cases, albeit somewhat less rigorous for the HKQ and LLFI than for the remaining questionnaires. No study evaluated all the psychometric properties.
ConclusionWe currently have eight hip-disability functional assessment questionnaires adapted to Spanish with satisfactory psychometric properties. We can measure the patient's perceived impact of his or her hip disease by selecting, among the different options, those alternatives that best fit our clinical or research objectives.
Realizar una revisión sistemática de la calidad de los procedimientos de adaptación y de las propiedades psicométricas de los cuestionarios autoadministrados de valoración funcional de cadera adaptados a la población española.
Material y métodoSe realizó una búsqueda en las bases de datos MEDLINE, EMBASE, CINAHL y Web of Science (desde su inicio hasta junio de 2016) para localizar todas las escalas adaptadas al español y analizar las diferentes fases del proceso de adaptación y sus propiedades psicométricas.
ResultadosSe identificaron 8 escalas que se agruparon en 3 apartados, según el tipo de patologías en las que se pueden utilizar, a) todo el miembro inferior: Lower Limb Functional Index (LLFI), Lower Extremity Functional Scale (LEFS) y Arthrose des Membres Inférieurs et Qualité de vie (AMICAL); b) rodilla y/o cadera: Western Ontario and McMaster Universities Osteoarthritis (WOMAC) index, Osteoarthritis Knee and Hip Quality of Life (OAKHQOL) y Hip and Knee Questionnaire (HKQ), y c) exclusivas de cadera: Hip Outcome Score (HOS) e International Hip Outcome Tool-33 (iHOT-33). El procedimiento de adaptación transcultural fue aceptable en todos los casos, aunque algo menos riguroso para las escalas HKQ y LLFI. Ningún estudio evaluó todas las propiedades psicométricas.
ConclusiónDisponemos actualmente de 8 cuestionarios de valoración funcional de cadera adaptados al español con aceptables características psicométricas. Podemos medir la repercusión percibida por el paciente de su patología de cadera seleccionando, entre las diferentes opciones, aquellas alternativas que mejor se adapten a nuestros objetivos, ya sean clínicos o de investigación.
Accurate assessment is essential in hip disability management in order to evaluate the progression of symptoms and functional limitation and to determine the efficacy of different treatments. This assessment may be carried out through several methods. In clinical practice increasing significance is given to measuring health and quality of life and numerous tools have been developed to measure both parameters.1 Functional evaluation scales provide information on the impact of the condition from the patient's viewpoint and are complementary to physical examination (mobility, strength, etc.) and the outcome obtained from imaging studies.2 Many questionnaires have been developed on an international scale to assess impact perceived by patients with hip disabilities. The majority of these questionnaires have been developed in English-speaking countries, which causes inconvenience when they are to be used in countries with different languages or cultures. An appropriate cross-cultural adaptation3,4 is necessary for them to be applied to patients of a different culture (a more complex process than simple translation) and validation of the scale,5 i.e. their reliability and validity must be established in the new linguistic groups in which they are to be applied.6 After Mandarin Chinese, Spanish is the second most spoken language in the world, with a broad geographical reach,7 both in countries which use it as an official language and those where it is used by immigrants residing in countries with different maternal languages.
In 2013 a review was made of questionnaires adapted into Spanish for patients with cervical and lumbar pain,8 but we have found no similar reviews for hip disabilities.
The aim of this article was to become acquainted with the cross-cultural adaptations of hip-specific patient-reported outcome measures in Spanish, with additional analysis of the methodological quality of the cross-cultural adaptation process and the psychometric properties of the new version obtained as a result.
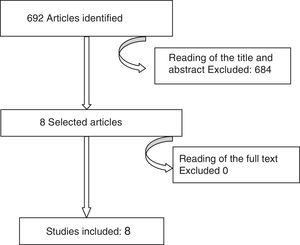
Material and MethodsSearch StrategyA systematic review of published articles on all cross-cultural adaptations of hip-specific patient-reported outcome measures in Spanish was carried out. We performed a bibliographic search from inception up to June 2016, in the electronic data bases MEDLINE (1966–2016), EMBASE (1974–2016), CINAHL (1977–2016) and Web of Science (1900–2016). The terms used and search strategy in MEDLINE used were as follows: “Outcome” or “Questionnaire” or “Assessment” or “Instruments” and “Hip” or “Lower limb” and “Spanish” or “Spanish version” or “Spanish validation” or “Spanish translation” or “Cross-cultural adaptation” or “Cross-cultural validation”. We also made a manual search using the names of the different hip scales as key words in the different data bases. A web search was also made which included Google Scholar, in order to cover a different type of publication. Finally, we manually examined the references of the articles obtained. Fig. 1 shows the selection of included studies.
Selection CriteriaFor each article found, two of the authors reviewed the title and the abstract. If these suggested that they could be selected, a complete reading of the article was made. We included articles without any language restriction on studies which described the cross-cultural adaptation into Spanish of self-completion questionnaires for functional assessment of patients with hip disabilities and which also analysed the psychometric properties of the new version. Articles which only analysed the properties of a previously adapted questionnaire, research protocols or congress summaries were excluded.
Information AnalysisTwo authors structured and analysed the manuscript results from the selected articles. Where discrepancy arose consensus was sought and when necessary a third reviewer became involved. The information analysis included:
- (a)
Participant traits. Patient data forming part of the study were collected: country and locality, total number of patients included, diagnosis, age and gender. We confirmed that at least 50 patients were included, the minimum recommended number for cross-cultural adaptation studies.4,5
- (b)
Assessment of cross-cultural adaptation. We confirmed whether this coincided with the 5 standard recommended steps in international references5,9,10 and if they had been followed appropriately. The five steps are: (1) direct translation of the original questionnaire into Spanish (made independently by at least two bilingual translators); (2) summary of translations and resolution of possible discrepancies; (3) inverse or retro-translation (of the consensual translation into Spanish back into the original language, by at least two independent translators, who were not aware of this said version); (4) review by a committee of experts for the development of the pre-final version, with assurance of semantic, idiomatic and conceptual equivalence of the scale and (5) pilot test (pre-test) of the pre-final questionnaire with Spanish speaking subjects (recommendations are to do this with 30–40 people), searching for unanswered items and possible comprehension problems. Each step was considered positive (+) when the procedure was correctly implemented; doubtful (?) when the description was unclear; negative (–) when it was correctly implemented but with an insufficient number of translators/patients, or zero (0) when information was insufficient to assess each step.
- (c)
Assessment of psychometric properties. The following aspects were analysed: reliability, validity and sensitivity to clinical changes.5,10–14 Reliability was measured using 3 parameters: (a) internal consistency, to determine the stability of the scores between the different elements which compose a scale —a measure of homogeneity—through Cronbach's alpha test with sufficient alpha values being considered above 0.7–0.8; (b) the reproducibility test-retest or appropriate time interval —temporary stability—measured with the intraclass correlation coefficient (ICC) with adequate values considered to be above 0.8, and (c) the degree of agreement measured by the standard error of the mean (SEM) and the minimum detectable change (MDC).
Validity was measured using two parameters: (a) The Pearson or Spearman correlation coefficients, with values ranging between –1 and +1. The value 0 indicates that there is no lineal association between the 2 study variables; (b) the floor and ceiling effects which appear when over 15% of respondents give the highest total scores (ceiling) or the lowest score possible (floor).
Sensitivity to clinical changes is the ability of the tool to detect clinically important changes over time. These are mostly measured through the size effect (SE) and the standardised response mean (SRM).
- (d)
Assessment of the applicability in different Spanish speaking countries. We analysed whether the adaptations made in Latin American countries needed any modifications to be able to be used in Spain, and vice versa.
We identified 8 relevant articles,15–22 which described 8 self-completion questionnaires cross-culturally adapted to the Spanish population and the clinimetric properties of which had been studied in the new version. Three questionnaires were applicable to any lower limb disability: Lower Limb Functional Index (LLFI)15; Lower Extremity Functional Scale (LEFS)16 and the questionnaire Arthrose des Membres Inférieurs et Qualité de vie (AMICAL).17 Three questionnaires were applicable to knee and hip disabilities: Western Ontario and McMaster Universities Osteoarthritis (WOMAC) index18; Osteoarthritis Knee and Hip Quality of Life (OAKHQOL)19 and Hip and Knee Questionnaire (HKQ).20 Lastly, there were 2 specific hip questionnaires: Hip Outcome Score (HOS)21 and the International Hip Outcome Tool-33 (iHOT-33).22
In all cases the original questionnaire had been created in English, save in 2: AMICAL17 and OAKHQOL,19 designed in French. Our search was not able to locate any questionnaires which had been originally designed in Spanish.
Table 1 lists the demographic and clinical characteristics of the population in which each of the studies was carried out. The adapted scale, together with instruction for the patient, was included in the publication in all cases except for 2 questionnaires: WOMAC18 and iHOT-33.22
Demographic and Clinical Characteristics of the Cross-cultural Adaptation Study Sample.
| Scale | Author, year of adaptation | Country (population) | Total number of patients included | Diagnosis | Age in years | Percentage of females (%) |
|---|---|---|---|---|---|---|
| LLFI15 | Cuesta-Vargas et al., 2014 | Spain (Malaga) | 136 | Chronic disability (>12 weeks) of lower limbs | Mean: 48 (SD±19) | 54.4 |
| LEFS16 | Cruz-Díaz et al., 2014 | Spain (Jaen) | 132 | Lower limb disability (1.5% diagnosed with osteoarthritis; 22% muscular pain; 9.1% ligament injury; 23.5% meniscus cartilage injury; 22–0% patellofemoral pain; 7.6% joint fracture, muscular or soft tissue) | Mean: 27.11(SD±6.22) | 44.7 |
| AMICAL17 | Espinosa-Cuervo et al., 2014 | Mexico | 100 | Coxarthrosis radiological grade II-III from the Kellgren and Lawrence classification | Mean: 56.34 (SD±13) | 67 |
| WOMAC18 | Villanueva et al., 2004 | Spain (Seville) | 73 | Coxarthrosis (at least grade II of the Kellgren and Lawrence classification) | Mean: 58.71 Range: 35–73 | 89 |
| OAKHQOL19 | González Sáenz de Tejada et al., 2011 | Spain (Canary islands) | 409 | Coxarthrosis | Mean: 71.26 (SD±7.71) | 63.3 |
| HKQ20 | Castellet et al., 2014 | Spain (unspecified) | 316 | Coxarthrosis with referral for knee prosthesis before and after surgery | ≥18 | – |
| HOS21 | Seijas et al., 2014 | Spain (unspecified) | 100 | Mixed acetabular impingement (37), Cam (26) type impingement, Cam +labrum (15), Tönnis II (5), Tönnis I (5), pincer type impingement (4), labrum lesion (3), trochanteritis (2), Salter-Harris fracture sequelae (1), Perthes disease sequelae (1) and osteonecrosis (1) | Mean: 45.1 (SD±12.1) Range: 18–65 | 36 |
| IHOT-3322 | Ruiz-Ibán et al., 2015 | Spain (unspecified) | 97 | Acetabular impingement (78: 65 mixed, 11 Cam type, 2 Pincer type), arthrosis (10), gluteus medius condition (3), Perthes disease sequelae (2), Salter-Harris fracture sequelae (2), psoas tendinitis (1), congenital hip dysplasia (1) and osteonecrosis (1) | Mean: 43.8 (SD±10.9) Range: 22–60 | 38.1 |
AMICAL, Arthrose des Membres Inférieurs et Qualité de vie; SD, standard deviation; HKQ, hip and knee questionnaire; HOS, hip outcome score; IHOT-33, international hip outcome tool-33; LEFS, lower extremity functional scale; LLFI, lower limb functional index; OAKHQOL, osteoarthritis knee and hip quality of life questionnaire; WOMAC, Western Ontario and McMaster Universities Osteoarthritis.
The majority of articles were published very recently. One of the adaptations was published in 201522 and 5 in 2014.15–17,19,21 The initial scale adapted into Spanish was the WOMAC, in 2004.18 This scale was adapted into Spanish for the first time in 1999,23 but did not then include the study of psychometric properties and was therefore excluded from our article selection.
All the questionnaires were validated in Spain, except one17 which was validated in Mexico. The number of patients was higher than the recommended 50 for this study type in all adaptations.
In general, the cross-cultural adaptation process of all scales required some minor modifications with respect to the original version. The main findings from assessment of the methodology used for cross-cultural adaptation are analysed in Table 2. Five questionnaires rigorously complied with the 5 steps of recommendations from international guidelines,16,17,19,21,22 the remainder were less strict in this regard. The pilot test was conducted in 6 scales,17–22 but only 221,22 did so with 30 patients.
Assessment of the Methodology Used for the Cross-cultural Adaptation of the Questionnaires.
| Scale | Translation | Summary | Inverse translation | Analysis by expert committee | Pilot test (number of patients) |
|---|---|---|---|---|---|
| LLFI15 | + | + | – | + | 0 |
| LEFS16 | + | + | + | + | 0 |
| AMICAL17 | + | + | + | + | + (10) |
| WOMAC18 | + | + | – | + | + (10) |
| OAKHQOL19 | + | + | + | + | + (17) |
| HKQ20 | + | + | – | ? | + (20) |
| HOS21 | + | + | + | + | + (30) |
| IHOT-3322 | + | + | + | + | + (30) |
+, correctly implemented;?, doubtful; –, incorrectly implemented or not implemented; 0, no information provided as to whether it was implemented or not; AMICAL, Arthrose des Membres Inférieurs et Qualité de vie; HKQ, hip and knee questionnaire; HOS, hip outcome score; IHOT-33, international hip outcome tool-33; LEFS, lower extremity functional scale; LLFI: lower limb functional index; OAKHQOL, osteoarthritis knee and hip quality of life questionnaire; WOMAC: Western Ontario and McMaster Universities Osteoarthritis.
The main psychometric properties analysed in the Spanish versions are shown in Table 3. No study assessed all the metric properties of the new version, In general, the authors’ conclusion regarding each of the adaptations made was that the psychometric properties assessed were acceptable and comparable with those of the original versions and other versions adapted into other languages.
Principal Psychometric Properties Analysed in the Adapted Questionnaires.
| Scale | Internal consistency (Cronbach's α) total | Test-retest reproducibility: number of participants (time between the two assessments) ICC | Tool of comparison: validity (correlation coefficient) | Ceiling/floor effects | Sensitivity | |
|---|---|---|---|---|---|---|
| SE | SRM | |||||
| LLFI15 | 0.91 | – 0.96 (Range 0.93–0.97) | WOMAC: strong (r=0.77) EQ-5D-3L: fairly and inversely correlated (r=–0.62) | – | – | |
| LEFS16 | 0.98 | – 0.998 (CI 95%: 0.996–0.999) | SF-36: functionality (r=0.896); physical role (r=0.800); emotional role (r=0.504); social (r=0.764); mental health (r=0.744); vitality (r=0.760); pain (r=0.903); general health (r=0.657); physical component=0.902); mental component (r=0.824); P<.01 | No/No | 2.3 | 1.9 |
| AMICAL17 | .946 | 65 (72h) 0.979 (CI 95%: 0.961–0.991) | WOMAC: VAS (r=0.737); functional ability (r=0.831); pain (r=–0.742); stiffness (r=–0.649); P<.05 SF-36: physical activity (r=0.709); physical role (r=0.678);mental health (r=0.705); general health (r=0.506); emotional role (r=0.432). In other domains, the correlations were low but significant: pain (r=0.484); social function (r=0.346); social support (r=0.287); P<.05 | – | – | |
| WOMAC18 | Subscale: Pain: 0.71–0.97 Function: 0.64–0.95 | 17 (72h) Subscale: Pain: 0.36–0.76 Function: 0.34–0.52 | WOMAC: pain (r=0.27); function (r=0.77) | – | – | |
| OAKHQOL19 | Range 0.60–0.93 | – Range 0.75– 0.81 | SF-36: moderately correlated with the physical domains (physical function, r=0.58; pain, r=0.64; general health, r=0.41; and PCS, r=0.59) WOMAC: moderately correlated with the function (r=–0.80) and pain (r=–0.69) EQ-5D: r>0.5 | – | – | |
| HKQ20 | 0.864 | Not studied | WOMAC: pain and functionality, r=0.641; stiffness, r=0.533 | No/No | – | |
| HOS21 | –(15 days) SubScale: DLA: .95 (IC 95%: .92–.97) Sport: .94 (CI 95%: .89–.97) | WOMAC: Subscale DLA: pain (r=0.699); stiffness (r=0.667); function (r=0.788) SubScale sport: pain (r=0.607); stiffness (r=0.499); function (r=0.764) | No/yes (for subScale sport) | Subscale: DLA – Sport: – | 1.53 1.27 | |
| IHOT-3322 | Global: 0.98 Subscale: Function: 0.97 Sport: 0.94 Work: 0.89 Social: 0.94 | –(15 days Global: 0.97 (CI 95%: .96–.99) Subscale: Function: 0.95 (CI 95%: .92–.98) Sport: 0.92 (CI 95%: 0.76–0.98) Trabajo: 0.93 (CI 95%:0.83–0.98) Social: .96 (CI 95%: 0.91–0.98) | WOMAC: Subscale functional: pain (r=0.744); stiffness (r=0.687); function (r=0.79) Subscale sport: pain (r=0.526); stiffness (r=0.513); function (r=0.536) Subscale work: pain (r=0.581); stiffness (r=0.544); function (r=0.616) Subscale social: pain (r=0.653); stiffness (r=0.574); function (r=0.658) | Yes/No | – | 1.18 |
The negative values of the correlation coefficients indicate inverse correlation.
AMICAL, Arthrose des Membres Inférieurs et Qualité de vie; DLA, daily life activities; EQ-5D-3L, European Health Questionnaire 5 Dimensions 3 Levels; VAS, visual analogue scale; HKQ, hip and knee questionnaire; HOS, hip outcome score; CI, confidence interval; ICC, intraclass correlation coefficient; IHOT-33, international hip outcome tool-33; LEFS: lower extremity functional scale; LLFI, lower limb functional index; OAKHQOL, osteoarthritis knee and hip quality of life questionnaire; PCS, physical component summary; SRM, standard response mean; SF-36, short form 36 health survey; SE, size effect; WOMAC, Western Ontario and McMaster Universities Osteoarthritis.
Regarding reliability, internal consistency was assessed in all scales. For test-retest reproducibility only in four was time between scales specified17,18,21,22 and of these only in two17,18 was the number of patients to whom it was applied mentioned. One17 of them surpassed the ideal number of over 29 patients recommended for this assessment. The level of agreement was only analysed in two scales.21,22
Total internal consistency in all scales was above 0.7–0.8, sufficient value to guarantee their reliability. The ICC was very good in all cases. The level of agreement was analysed in two questionnaires.21,22 Seijas et al.21 analysed the MDC which was 13.7 for the daily life activities (DLA) subscale and 22.8 for the sports subscales, and the SEM was ±5.1 in DLA and ±8.5 for sports. Ruiz-Ibán et al.22 calculated the MDC and SEM values as 12.5 and 4.66, respectively.
Validity was assessed in all questionnaires. This varied according to the tools of comparison but was generally appropriate. The floor and ceiling effects were analysed in four questionnaires,16,20–22 with the ceiling effect being present in one21 and the floor effect in another.22
Sensitivity was examined in only three scales.16,21,22 In two of them only the SRM,21,22was measured and only in one16 were values for SE and SRM available, which indicated great sensitivity in both cases.
In the AMICAL17 questionnaire the cross-cultural adaptation was carried out in a Latin American country (Mexico). There were no marked cultural differences to hinder the use of the questionnaire in Spain. The introduction of minor changes in some of the words used enable usage. For example, the word “pesero” (cab) could be replaced with “autobús” (bus).
DiscussionOur aim was to systematically review the self-completion questionnaires for hip disability adapted into Spanish by analysing the methodological quality of the cross-cultural adaptations and verifying the psychometric properties of the new version obtained. Whilst reviewing we found eight questionnaires which had been adapted into Spanish.15–22 In all cases the adaptation procedure had been accurately implemented, following international recommendations3–5 and ensuring conceptual equivalence with the original version which had been designed in another language. Maximum rigour was employed for five questionnaires.16,17,19,21,22 The psychometric properties analysed were acceptable and were generally similar to those of the original version and to that of other versions of the scale adapted into other languages. None of the studies assessed all possible psychometric properties but reliability and validity were analysed in all of the questionnaires in different ways.
During the last few decades numerous scales for hip disabilities24–36 have been developed. It is preferable to adapt an already existing questionnaire than create a new one, always checking that the new version maintains the psychometric properties of the original. Adaptation is a more economical process and the use of the same questionnaire makes it easier to make comparisons between different populations. The seven questionnaires adapted into Spanish could easily be used in Latin American countries. However, in some cases it would be necessary to make a few minor changes to some of the words used to adapt them to local parlance in some countries. The same applies to the adapted in Mexico17 for its use in Spain or other Latin American AMICAL questionnaire countries. The fact that in the majority of studies the participants were predominantly female,15,17–20 except in three, does not appear to be an impediment for the questionnaires being used on males.
The eight questionnaires adapted into Spanish have different traits and the choice of one or the other would vary depending on needs and context, which could be either clinical and/or research. To select which questionnaire to use both methodological criteria (psychometric properties) and different practical aspects would need to be considered, such as the time needed to complete the questionnaires and give scores and their usefulness for certain disabilities and/or certain patient groups.
Of the eight questionnaires identified in the review there were three for any lower limb disabilities (LLFI, LEFS y AMICAL),15–17 another three for knee and/or hip disabilities (WOMAC, OAKHQOL y HKQ)18–20 and two exclusively for hip disabilities (HOS y iHOT-33).21,22 The most common used on an international scale are LEFS and WOMAC.
The LEFS questionnaire contains 20 questions. Unlike the WOMAC, discrimination may be made between pain and physical function. It is completed in 2min and scored in 2s. The LLFI questionnaire, containing 25 items has not yet been used much as it is of very recent creation. The AMICAL questionnaire is the only one to specifically assess the patient's quality of life with lower limb arthrosis. Its drawback is that it contains 43 questions and the patient takes around 15min to complete it.
The WOMAC questionnaire is the one most used internationally to assess the functional capacity of patients with knee and/or hip arthrosis and to assess the efficacy of the results of conservative and surgical treatments. It contains 24 items and the patient takes around 5–10min to complete it. Two shorter versions have been made, with just 11 and 14 questions, aimed at obtaining the same information as the original questionnaire but with a shorter administration time. We verified that both versions in Spanish maintained the same psychometric properties as the 24 item version.37–39 These new versions could be used in clinical practice and in research. With regard to negative aspects, the WOMAC scale does not assess aspects relating to quality of life and does not enable any discrimination between which joint is responsible in the case of hip and knee being simultaneously compromised. Scores may be changed by the presence of back pain, alterations in mood and other extra-articular disabilities.40 The OAKHQOL questionnaire is very complete since it includes aspects relating to mental health, social support, personal relations, sexual activity and professional life. The high number of items they contain hinders their use in clinical practice. The HKQ questionnaire consists of 16 questions. Its validation into Spanish was made only in knee arthroplasties, without including patients with hip disabilities. This could be a drawback when applying it to this patient type.
The classic questionnaires designed to assess outcome in older patients with hip arthrosis are less useful in young and active patients with non-arthritic conditions and with greater functional demands. Two adapted questionnaires are available for these patients. The HOS questionnaire contains 28 items and specifically assesses functional aspects. In a recent meta-analysis34 its use was recommended to assess the outcome after hip arthroscopy. The iHOT-33 questionnaire, unlike the HOS questionnaire, assesses emotional, social, employment and lifestyle aspects. There is a shorter version of 12 questions (iHOT-12)41 which could be more viable in clinical practice although it has not yet been validated into Spanish.
The review is particularly relevant because six of the eight adaptations were published during the last two years. As strengths of our review we may highlight, firstly, that both the rigour of the adaptation process of the questionnaire into Spanish and the psychometric properties analysed were examined by two authors. Moreover, the search process was exhaustive, and it is therefore improbable that other published scales adapted into Spanish could be found. Although we selected the most used data bases, it is possible that some studies were not detected since some journals cannot be indexed in these data bases.
To conclude, there are eight available scales for measuring the functional limitation of the hip which were adapted into Spanish, following international recommendations (five with maximum rigour). All had acceptable psychometric properties. Most adaptations (6 out of the 8) had been published in the last two years (from 2014). Several had been designed for the older adult population and others for typical problems seen in younger patients (mainly femoroacetabular impingement). Several specifically focused on functional assessment (shorter and simpler, but valid for standard clinical practice), whilst others covered multiple aspects (emotional, social, employment, etc.), which made them particularly suitable for evaluating complex cases or those with research objectives.
Ethical LiabilitiesProtection of people and animalsThe authors declare that no experiments using human beings or animals have been carried out for this research study.
Data confidentialityThe authors declare they have followed the protocols of their centre of work on patient data publication.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Gómez-Valero S, García-Pérez F, Flórez-García MT, Miangolarra-Page JC. Revisión sistemática de los cuestionarios autocumplimentados adaptados al español para la valoración funcional de pacientes con patología de cadera. Reumatol Clín. 2018;14:372–378.