SAPHO (synovitis, acne, pustulosis, hyperostosis, and osteitis) syndrome is a cluster of osteo-cutaneous manifestations that can lead to serious complications such as thrombosis of the subclavian vein or superior vena cava, mainly in patients with significant inflammatory involvement of the anterior chest wall. The objective of this study was to review the cases published in the medical literature related with the presence of thrombotic complications in patients diagnosed with SAPHO syndrome and to try to determine their possible pathogenic mechanism and risk factors. We analyzed 11 published reports of isolated clinical cases or case series, a total of 144 patients, which described a total of 15 cases of venous thrombosis. The clinical characteristics of these patients, evaluated to determine whether they meet the ASAS criteria for axial and peripheral spondyloarthritis, are analyzed and the need for early diagnosis and treatment is highlighted.
El síndrome SAPHO (sinovitis, acné, pustulosis, hiperostosis y osteítis) comprende un conjunto de manifestaciones cutáneo-osteoarticulares. Se han descrito algunas complicaciones graves que pueden aparecer durante la evolución de la enfermedad, como la trombosis venosa, principalmente en pacientes que desarrollan afectación inflamatoria grave de la pared torácica anterior. El objetivo de la presente revisión fue analizar los casos descritos en la literatura médica relacionados con la presencia de complicaciones trombóticas en pacientes diagnosticados de síndrome SAPHO e intentar establecer los probables factores de riesgo y su posible mecanismo patogénico. Se analizaron 11 artículos publicados de casos clínicos aislados o series de casos, con un total de 144 pacientes, que describen en total 15 casos de trombosis venosa. Se exponen las características clínicas de estos pacientes, se evalúa si cumplen los criterios de clasificación ASAS para espondiloatritis axial y periférica, y se resalta la necesidad de realizar un diagnóstico y tratamiento precoces.
SAPHO syndrome is a cluster of osteo-cutaneous manifestations that appear simultaneously or sequentially along a patient's life. The term SAPHO is an acronym of the most common manifestations: synovitis, acne, pustulosis, hyperostosis, and osteitis. Its etiology is unknown and affects children and young adults, with similar distribution by gender. Most authors classify it under spondyloarthritis. It is probably a reactive arthropathy secondary to infection by a low virulence agent. Involvement of the anterior chest wall may be so pronounced as to cause thoracic outlet syndrome venous with compression of the subclavian vein and superior vena cava.1–3 This vascular compression can lead to thrombosis of the veins in the chest wall outlet due to hyperostosis and/or extrinsic compression by a soft tissue mass in the mediastinum.4
Review of the LiteratureWe conducted a review of the literature using PubMed and using SAPHO syndrome and thrombosis [SAPHO syndrome AND thrombosis] as criteria. We found 11 articles published describing a total of 15 cases of venous thrombosis.3–13 One was a retrospective series of 120 cases, and only describes a case of thrombosis of the subclavian vein.3
ResultsVenous thrombosis as an association/complication of SAPHO syndrome is described in 15 published cases. In 14, thrombosis was located in the subclavian veins, 5 bilaterally. Four of these 14 patients also had obstruction at other levels: 2 in the superior vena cava, one in the jugular vein and one at the level of the right iliac vein.5–7 Coloe et al. describe a patient who presented bilateral iliofemoral obstruction complicated with pulmonary embolism.8
According to the distribution by gender, 10 were male and 5 female. The mean age of patients was 44.6 years. Therefore the duration of both joint as well as skin symptoms exceeded 10 years. Eight patients had cutaneous manifestations, 6 had palmoplantar pustulosis and 2 severe acne.5,6,8,9 Among the osteoarticular manifestations of the 9 patients with involvement of the anterior chest wall (osteochondritis),4,5,7–13 4 cases were also associated with peripheral arthritis (shoulder)4,5,7 and 2 with lumbar spine involvement.5,11,13 The remaining 5 had axial involvement, 4 of the lumbar spine and one at the cervical spine-level. Four of the patients had sacroiliitis (clinical and radiographic).5,6,8,11 Detection of high acute phase reactants (ESR and CRP) in serum samples was constant in virtually all patients, and in nine patients the determination of HLA-B27 was available, resulting positive in 2 cases and negative in the rest (Table 1).
Demographic and Clinical Characteristics of the Analyzed Cases.
| Reference | Age | Gender | Skin M. | T. since disease onset≥10 years | Thrombosis | Sacroiliitis | HLA-B27 |
|---|---|---|---|---|---|---|---|
| Haenel et al.4 | 67 | F | No | — | Basilic, axillary and left subclavian | No | Negative |
| Van Holsbeeck et al.5 | 46 | M | PP | — | Subclavian, cephalic and right jugular | No | Negative |
| Van Holsbeeck et al.5 | 43 | M | PP | — | Bilateral subclavian | Unilateral | Negative |
| Kawabata et al.6 | 42 | F | PP | Yes | Superior vena cava, bilateral subclavian | Bilateral | Positive |
| Legoupil et al.7 | 44 | M | No | Yes | Right iliac | No | Positive |
| Coloe et al.8 | 15 | M | Acne | – | Bilateral iliofemoral | Bilateral | – |
| Lazzarin et al.9 | 48 | F | PP | Yes | Right subclavian | No | Negative |
| Köhler et al.10 | 53 | M | No | Yes | Bilateral subclavian | No | – |
| Köhler et al.10 | 51 | M | No | Yes | Left subclavian | No | – |
| Köhler et al.10 | 44 | M | No | Yes | Bilateral subclavian | No | – |
| Köhler et al.10 | 66 | F | PP | Yes | Bilateral subclavian | No | – |
| Cunningham et al.11 | 45 | M | PP | Yes | Right subclavian | Unilateral | Negative |
| Jirik et al.12 | 17 | M | Acne | Left subclavian | No | Negative | |
| Rosero et al.13 | 56 | M | No | Yes | Left subclavian | No | Negative |
F: female; PP: palmoplantar pustulosis; M: male.
Of the articles analyzed, only 8 patients (53%) met ASAS criteria: 6 for axial spondyloarthritis5,11 and one for peripheral spondyloarthritis.5 Hayem et al.3 described involvement of the dorso-lumbar spine in 40 patients, and sacroiliitis in 48 patients. The presence of HLA-B27 was detected in 11 patients. This data lead them to confirm that the SAPHO syndrome belongs to the group of spondyloarthritis. This publication did not provide sufficient data to analyze how many of these patients met the ASAS criteria for axial spondyloarthritis: chronic low back pain for more than 3 months in patients under 45 years of age plus the presence of positive HLA-B27 or sacroiliitis on imaging and some feature of spondyloarthritis. There was no evidence of peripheral spondyloarthritis, although many of them could be included in these clinical categories.
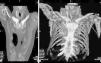
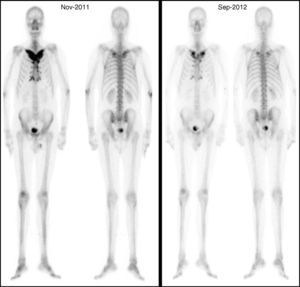
Thrombosis was the initial manifestation in 6 cases. Case number 15 was seen by our service in 2012, at present showing good response to treatment with methotrexate and glucocorticoids as seen in bone scans performed before and after treatment13 (Figs. 1 and 2). Bone scintigraphy was, in this case, very important for the diagnosis and assessment of response to treatment.
CT scan of the chest where clavicular hyperostosis and ankylosis of the sterno-clavicular joint are observed.
On chest radiographs there was evidence of clavicular hyperostosis in 10 patients, 2 of which had a mass in the upper mediastinum.5 8 cases also underwent a computed tomography (CT) where hyperostosis was confirmed, with sclerosis of clavicle and manubrium and, in some cases, further erosions in the sternoclavicular joint, a retromediastinal mass and thrombosis at different levels, as the case already described from our hospital.13 One patient was scanned with MRI in which a mass of soft tissue located in the last lumbar vertebral bodies was appreciated, with obstruction of the right iliac vein.7 Tc99 scintigraphy was performed in 7 cases; there was increased tracer uptake in the clavicle and manubrium sternoclavicular joint (bull's head sign), highly suggestive and almost pathognomonic uptake associated with SAPHO syndrome.
From the therapeutic point of view, most of the patients were treated with nonsteroidal antiinflammatory drugs (NSAIDs). On 2 occasions glucocorticoid was used orally; in one case with severe disease, administration of biological therapy (anti-TNF-alpha)8 was necessary. In most patients, oral anticoagulants were used for 6 months, but no chronic anticoagulation was needed due to the fact that the cause was an extrinsic compression of the vessels and 2 patients needed surgery due to recurrent thrombosis.5,9
DiscussionThe pathogenesis of SAPHO syndrome remains unclear, even accounting for the fact that no conclusive data on the etiopathogenic mechanism of thrombotic complications exists, although it is believed that the most important mechanism is venous compression due to hyperostosis or the mass of surrounding soft tissue. There is also the assumption that a state of systemic inflammation may contribute to the hypercoagulable syndrome. Some authors have suggested that dysfunction of the immune system in SAPHO syndrome may be associated with hyperstimulation of the innate immune response. The increased production of IL-8 and TNF-alpha by neutrophils and decreased IL-10 support this theory. These cytokines appear to play a key role in the recruitment of phagocytic cells to inflammatory sites and in the pathogenesis of osteitis.14 Although some cases accompanied by lupus anticoagulant have been published, antiphospholipid syndrome is not considered to be an associated cause, already infrequent, of the presence of venous thrombosis5 in SAPHO syndrome.
Venous thrombosis as a complication of SAPHO syndrome is rare. After the analysis of published cases, it is not possible to establish predictive risk factors for thrombosis. The vast majority of patients had passed over 10 years since onset of symptoms, 73% were male; there were elevated ESR, CRP, alpha, and gamma globulins. From the radiological point of view, important hyperostosis was observed. Because of the number of patients and lack of comparison with other series of SAPHO syndrome, we cannot propose these as risk factors for the development of thrombosis. Therefore it is necessary to study more deeply this data in the future to be able to identify potential risk factors for thrombosis.
ConclusionVenous thrombosis is a rare complication of SAPHO syndrome, with an unclear pathogenesis. Factors that can contribute to its development are time since disease onset, male gender, elevated acute phase reactants and the degree of hyperostosis. It is believed that hyperostosis or inflammation of adjacent soft tissues may be related to venous compression, in addition, systemic inflammation may contribute to a hypercoagulable state, but there is insufficient data to confirm this hypothesis, so its pathophysiology or its risk factors are currently not entirely clear. However, larger studies are needed to include more complete patient data, investigate possible vascular risk factors and thrombophilia in order to establish that patients with SAPHO syndrome are at risk of thrombosis and preventing data.
Since in some cases thrombosis was the first symptom of the disease, it is necessary to have a high index of suspicion in these patients; SAPHO syndrome should be included in the differential diagnosis of thrombosis/compression of the subclavian vein or the superior vena cava, especially if accompanied by pain of inflammatory characteristics of the anterior chest wall.
Finally, it is important to add that it is essential to make an early diagnosis and treatment onset for SAPHO syndrome to avoid significant long-term complications such as venous thrombosis, which may compromise the patient's life.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of InterestThe authors have no conflict of interest to state.
Please cite this article as: Carranco-Medina TE, Hidalgo-Calleja C, Calero-Paniagua I, Sánchez-González MD, Quesada-Moreno A, Usategui-Martín R, et al. Manifestaciones trombóticas en el síndrome SAPHO. Revisión de la literatura. Reumatol Clin. 2015;11:108–111.