Pulmonary hypertension (PH) associated with systemic sclerosis (SSc) increases morbidity and mortality. Cardiopulmonary comorbidities, as per the 2021 PH consensus, play a role in the choice of therapy between monotherapy and combination therapy.
MethodsA cross-sectional study was conducted in patients with SSc based on the 2013 ACR/EULAR criteria or very early disease (VEDOSS 2011). PH was considered if they met the following criteria: pulmonary artery systolic pressure (PASP)>39mmHg or peak tricuspid regurgitation velocity (PTRV)>3.4m/s, PASP between 33 and 39mmHg or PTRV between 2.9 and 3.4m/s plus two additional findings suggestive of PH. PH was classified as type 2 if LVEF<50% or moderate to severe diastolic dysfunction was present; type 3 if extensive interstitial disease on tomography>20% or forced vital capacity (FVC)<75%; type 4 if abnormalities related to embolism were detected on scintigraphy or tomography. If patients did not meet these criteria, they were classified as type 1 PH. Complete data on cardiopulmonary risk factors and other factors were required. The frequency of these factors in the population and differences between groups based on risk factors were estimated.
ResultsA total of 228 patients were selected. Three had type 2 PH, 24 had type 3, and 40 had type 1 PH, with the majority (75%) having at least one cardiopulmonary risk factor, and 47.5% having more than one. Mild diastolic dysfunction (25%) and hypertension (35%) were the most prevalent. In the type 1 PH group, those with risk factors experienced an increase in the number of years with Raynaud's phenomenon, anticentromere antibodies, and gastrointestinal symptoms (p<0.05).
ConclusionIn patients with PH, 75% have one, and 45% have two or more risk factors.
La hipertensión pulmonar (HP) asociada con esclerosis sistémica aumenta la morbimortalidad. Las comorbilidades cardiopulmonares, del consenso de la HP del 2021 desempeñan un papel en la elección de la terapia entre monoterapia y combinada.
MétodosSe llevó a cabo un estudio transversal en pacientes con esclerosis sistémica según criterios ACR/EULAR 2013 o enfermedad muy temprana (VEDOSS 2011). Se consideró HP si cumplían los siguientes criterios: presión sistólica de la arteria pulmonar>39mmHg o velocidad máxima de regurgitación tricuspídea>3,4m/s, presión sistólica de la arteria pulmonar entre 33 y 39mmHg o velocidad máxima de regurgitación tricuspídea entre 2,9 y 3,4m/s más 2 hallazgos adicionales de HP. Se consideró HP tipo 2 si fracción de eyección del ventrículo izquierdo<50% o disfunción diastólica moderada a grave; HP tipo 3 si enfermedad intersticial extensa en tomografía>20% o capacidad vital forzada<75%; HP tipo 4 si presentaba anomalías en gammagrafía o tomografía relacionadas con embolia. Si no cumplían con lo anterior, se considero HP tipo 1. Debían tener datos completos sobre factores de riesgo cardiopulmonares además de otros. Se estimó la frecuencia de estos factores en la población y las diferencias entre grupos en función de factores de riesgo.
ResultadosSe seleccionaron 228 pacientes. Tres HP tipo 2, 24 tipo 3 y 40 como tipo 1, la mayoría (75%) tenía al menos un factor de riesgo cardiopulmonar y el 47,5% tenía más de uno. La disfunción diastólica leve (25%) y la hipertensión (35%) fueron los más prevalentes. En el grupo HP tipo 1, aquellos con factores de riesgo tuvieron aumento en el número de años con fenómeno de Raynaud, anticuerpos anticentrómero y síntomas gastrointestinales (p<0,05).
ConclusiónEn pacientes con HP, el 75% tiene uno y el 45% 2 o más factores de riesgo.
Pulmonary hypertension (PH) commonly affects patients with systemic sclerosis (SSc) and is associated with significant morbidity and increased mortality, being the second cause of death after interstitial lung involvement.1 PH is a heterogeneous condition, and several different forms can be associated with SSc, including pulmonary arterial hypertension (PAH) resulting from pulmonary arterial vasculopathy, PH due to left heart disease, and PH due to interstitial lung disease.2
The 2013 American College of Rheumatology (ACR)/European League Against Rheumatism (EULAR) criteria3 are the main criteria used to classify systemic sclerosis (SSc); however, early disease has been recognized before skin thickening, which led to the development of parameters for earlier stages of the disease referred to as VEDOSS (very early diagnosis of systemic sclerosis),4,5 when interstitial pulmonary disease, or PH could be present.6,7
All kinds of PH are characterized by a mean pulmonary arterial pressure (mPAP)>20mmHg in right heart catheterization (RHC), according to the 2018 World Symposium on Pulmonary Hypertension.8 RHC is an invasive procedure that demands highly specialized medical services and high costs, making it difficult to perform on every patient. Additionally, it cannot be mandatory in cases of severe lung disease or left heart dysfunction. On the other hand, echocardiography can be used to estimate the prevalence of PH in SSc populations10,11 and classify the likelihood of PH,9 based on pulmonary pressure and other relevant factors. It is also less expensive and simpler to execute.
According to the 2022 European Society of Cardiology (ESC) and the European Respiratory Society (ERS) Guidelines for the diagnosis and Treatment of pulmonary hypertension,14 combination therapy is known to be more effective than monotherapy for simple or composite outcomes12,13; however, they recognized that patients with PAH and cardiopulmonary risk factors related to heart failure with preserved ejection fraction (left heart phenotype) and mild pulmonary disease who still classify as group I PH (cardiopulmonary phenotype) are under-represented in or excluded from trials, and an evidence-based recommendation for this group of patients may not be appropriate because they respond less well, are more likely to discontinue the medication for lack of tolerance, and also have higher mortality.
Considering these factors, patients at risk should be switched to monotherapy before mortality probability categorization, as illustrated in the treatment algorithm,14 rather than receiving combination therapy.
It is not clear how to categorize a patient into this group, despite the fact that recognizing a cardiopulmonary risk phenotype is now essential when making the selection of treatments. Some data has been analyzed using three or more risk factors. Some data have been analyzed using three or more risk factors for the existence of a particular phenotype, such as clinical trial exclusion criteria,12 which is different from the COMPERA registry,15 with only one risk considered, at which 15.8% had a left heart phenotype, 51.6% had a cardiopulmonary phenotype, and only 12.6% had a classic phenotype. There is no information specifically about individuals with autoimmune disorders like systemic sclerosis, who are considered to be a significant subset of the population with PH for whom significant adjustments in treatment approaches will be necessary.
The purpose of this investigation is to determine the prevalence of cardiopulmonary risk factors in a population of patients with systemic sclerosis and a high likelihood of pulmonary hypertension.
MethodsA cross-sectional, analytical, observational study was conducted in patients with established scleroderma diagnosed by 2013 ACR/EULAR criteria or with early disease according to 2011 VEDOSS criteria who presented with pulmonary hypertension of any type. All patients undergo an annual echocardiogram as part of the screening strategy proposed by the European Society of Cardiology (ESC) and the European Respiratory Society (ERS). This strategy is the most commonly used, considering the difficulty of access and the delay involved in a later diagnosis through additional tests such as pro BNP and carbon monoxide diffusion. Consequently, based on the echocardiographic findings and the likelihood of pulmonary hypertension, patients are selected for invasive tests
For this purpose, the databases of patients seen in a rheumatology department over a period of three years were analyzed. Patients were included in the early disease group if they did not have skin involvement due to skin thickening.
The main objective was to determine the characteristics of pulmonary hypertension of any type according to the cardiopulmonary and pulmonary risk factors defined in the latest consensus for the diagnosis and treatment of pulmonary hypertension in 2022.14 The specific objectives were to compare whether there was any difference in some clinical or paraclinical characteristics of the disease between groups with or without risk factors.
Patients were considered to have PH if they met any of the following criteria: Pulmonary artery systolic pressure (PASP)>39mmHg or peak tricuspid regurgitation velocity>3.4m/s, PASP between 33 and 39mmHg or peak tricuspid regurgitation velocity between 2.9 and 3.4m/s, with two additional findings of pulmonary hypertension in the echocardiography according to the European guidelines for the diagnosis and treatment of pulmonary hypertension,14 and therefore considered of high probability.
A patient was considered to have a high probability of type 2 pulmonary hypertension if he presented echocardiographic findings of systolic dysfunction due to a left ventricular ejection fraction less than 50% or moderate to severe diastolic dysfunction reported by the echocardiographer.
A patient was considered to have a high probability of type 3 pulmonary hypertension if he had chest high-resolution computed tomography (HRCT) findings of extensive interstitial lung disease greater than 20% or forced vital capacity (FVC)<75%.
A patient was considered to have a high probability of type 4 pulmonary hypertension if he presented abnormalities in pulmonary ventilation and perfusion scintigraphy or thoracic angiography with findings related to pulmonary embolism.
Patients who do not meet the criteria for possible types 2, 3, or 4 pulmonary hypertension are considered to have a high probability of having type 1 PH as the main mechanism of the disease.
Patients should have complete data on cardiopulmonary risk factors mentioned in the latest European guidelines for the diagnosis and treatment of pulmonary hypertension by 2022.14 Cardiovascular risk factors include obesity (body mass index>29.9), arterial hypertension (HT), diabetes mellitus (DM), and coronary heart disease. Pulmonary risk factors include signs of mild interstitial lung disease, which we consider to be less than 20% extension, and an adjusted diffusion capacity of carbon monoxide (DLCO)<45%.
In addition to this, data were obtained for other factors taking into account the intrinsic relationship with heart disease: atrial fibrillation, dyslipidemia, echocardiographic evidence of mild diastolic dysfunction, left ventricular hypertrophy, and chronic kidney disease, although these were not part of the factors categorizing patients with a cardio-pulmonary phenotype, their occurrence frequency is merely described.
Regarding pulmonary factors, all patients should have data on pulmonary disease typification obtained either by tomography, spirometry, or DLCO.
For the descriptive analysis, measures of frequency, central tendency, and dispersion will be used according to the type of variable. For the analysis of the differences in risk factors and clinical characteristics between groups, the Chi2 test and logistic regression will be used according to the nature of the variables. Statistical analysis will be performed in the STATA 17 program. A value of p less than 0.05 was considered statistically significant. The present study meets the requirements stipulated by the Ministry of Health of Colombia and has been approved by an ethics committee.
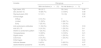
ResultsWe identified 245 patients with a systemic sclerosis diagnosis in the databases; however, 17 of these patients did not have an echocardiographic report in their medical history and were therefore excluded. The characteristics of the population are presented in Table 1. All patients presented Raynaud's phenomenon upon admission. For those who exhibited puffy fingers, there is insufficient data in the records to clarify whether this was the first manifestation of the disease or not.
Characteristics of the population.
| Variable | |
|---|---|
| Clinical characteristics | |
| Skin involvement (%) | |
| Early/sine scleroderma | 28.5 |
| Limited | 52.3 |
| Diffuse | 19 |
| Years of Raynaud (SD) | 10.2 (8.4) |
| Puffy fingers (%) | 29 |
| Rodnan skin score (SD) | 9.6 (9.8) |
| Digital ulcers (%) | 23.8 |
| Calcinosis (%) | 21.8 |
| Telangiectasias (%) | 71 |
| Arthralgia/arthritis (%) | 55 |
| Dyspepsia (%) | 72 |
| Dyspnea | 74.5 |
| Immunological | |
| Auto antibodies | |
| Centromere (%) | 64 |
| SCL-70 (%) | 9.5 |
| ANAS-no centromere | 48.5% |
| Capillaroscopy n (19) | |
| Normal (%) | 10.5 |
| Early (%) | 15.7 |
| Active (%) | 58 |
| Late (%) | 15.8 |
| Treatment | |
| Methotrexate (%) | 41 |
| Cyclophosphamide (%) | 30 |
| Mycophenolate mofetil (%) | 16 |
| Azathioprine (%) | 6.8 |
| Rituximab (%) | 4.5 |
| Nifedipine (%) | 75 |
SD: standard deviation, ANAS: antinuclear antibodies.
Echocardiography revealed that 67 (29.3%) of the 228 remaining patients met the criteria for a high probability of pulmonary hypertension. 61 (91%) had a PASP greater than 39mmHg (mean 53mmHg) or a peak tricuspid regurgitation velocity higher than 3.4m/s. There were no differences in these measurements among the different subsequently classified PH groups (p=0.14).
Only 10 patients had their peak tricuspid regurgitation velocity measured, and two of them did not report PASP. Ten patients who underwent cardiac catheterization confirmed the presence of pulmonary hypertension, all individuals exhibited medium pulmonary artery pressures exceeding 22, pulmonary resistances surpassing 3 Wood units, and capillary wedge pressures below 15mmHg, indicative of type 1 pulmonary hypertension.
There were no reports of moderate to severe diastolic dysfunction among the 67 patients, but three were diagnosed with clear left heart disease because of a left ventricular ejection fraction below 50%. Among them, none had a known history of coronary artery disease. It's important to note that no left heart catheterization was performed on any patient. However, data on ventricular contractility disorders were analyzed, revealing abnormalities in two patients, who also exhibited significant pulmonary involvement and were included in the group classified as Type 3 pulmonary hypertension.
Regarding the possibility of group 3 PH, tomography demonstrated pulmonary intestinal involvement in 33 patients (49%), and an extension of greater than 20% in 16 of these patients. 50 patients underwent spirometry, and 12 of them reported an FVC less than 75% of what was predicted. In a study of carbon monoxide diffusion capacity in 31 patients, 19 (61%) had an adjusted value of less than 80%, while only 3 (all with extensive interstitial lung disease) had a value of less than 45%. On the basis of the previous information, it was determined that 22 patients (32%) had extensive pulmonary involvement from interstitial disease or an FVC alteration and were therefore classified as group 3 PHT. Only 1 patient was found to have extensive pulmonary disease and a depressed LVEF; this patient was included in Group 2; and 1 patient was found to have findings in pulmonary ventilation and perfusion gramagraphy compatible with chronic embolic disease; this patient also had extensive interstitial lung disease and was included in Group 3 PH; as well as 2 patients with a severe COPD diagnosis without interstitial compromise in tomography and oxygen requirement, for a total of 24 patients.
After identifying patients with a high probability of PHT from groups 2, 3, and 4, 40 patients remain in group 1. Table 2 describes the clinical characteristics of this last cohort.
Description of the patients with group 1 PH. n=40.
| Variable | n (%) |
|---|---|
| Cardiac risk factors | |
| HT | 14 (35%) |
| Obesity | 3 (7.5%) |
| Diabetes mellitus | 4 (10%) |
| Atrial fibrillation | 1 (2.5%) |
| Coronary artery disease | 1 (2.5%) |
| Dyslipidemia | 4 (10%) |
| CKD | 1 (2.5%) |
| Ventricular hypertrophy | 8 (20%) |
| Diastolic dysfunction | 10 (25%) |
| Pulmonary risk factors | |
| Mild interstitial lung disease | 13 (32.5%) |
| DLCO adj<45% | 1 (2.5%) |
| Mild OSAS | 6 (15%) |
| Cardiac factors only | 16 (40%) |
| Pulmonary factors only | 5 (12.5%) |
| Both risk groups | 11 (27.5%) |
| No risk factors | 8 (25%) |
| Two or more risk factors | 19 (47.5%) |
HT: hypertension, CKD: chronic kidney disease, DLCO adj: adjusted diffusion capacity of carbon monoxide, OSAS: obstructive sleep apnea syndrome.
We identified a substantial occurrence of moderate diastolic ventricular dysfunction in 25% of the patients, with hypertension being the predominant risk factor in 35%. A significant majority (75%) of patients exhibited at least one cardiopulmonary risk factor, and nearly half (47.5%) presented with multiple risk factors
The differences between the groups with and without risk factors in patients with highly probable group 1 PH are explained in Table 3. Those with risk factors had a statistically significant increase in the number of years with Raynaud's phenomenon, anti-centromere antibodies, and gastrointestinal symptoms (p<0.05). A higher frequency of digital ulcers was also seen without cases in the group without risk factors (p=0.06), but this difference was not statistically significant.
Differences between groups with or without risk factors in patients with highly probable group 1 PHT.
| Variable | Risk group | p | |
|---|---|---|---|
| With risk factors (n=32) | No risk factors (n=8) | ||
| Age (mean, SD) | 62.2 (10.8) | 61.3 (10.8) | 0.67 |
| Sex (women %) | 31 (97%) | 8 (100%) | 0.61 |
| Raynaud years (SD) | 12.4 (8.1) | 4.5 (5.5) | 0.01 |
| Clinical stage | 0.8 | ||
| Diffuse | 3 (9.5%) | 1 (12.5%) | |
| Limited | 17 (53%) | 4 (50%) | |
| Early | 12 (37.5%) | 3 (37.5%) | |
| Anti centromeric antibodies | 24 (75%) | 5 (62.5%) | 0.47 |
| Anti SCL-70 | 2 (6.2%) | 0 | 0.47 |
| ANAS no centromeric pattern | 12 (66.6%) | 6 (33.3%) | 0.05 |
| Telangiectasias | 24 (77.4%) | 4 (50%) | 0.12 |
| Digital ulcers | 10 (32.2%) | 0 | 0.06 |
| Calcinosis | 9 (28%) | 1 (12.5%) | 0.36 |
| Fingers edema | 13 (59%) | 5 (62%) | 0.86 |
| Articular disease | 16 (50%) | 5 (62.5%) | 0.95 |
| Gastrointestinal symptoms | 24 (75%) | 3 (37.5%) | 0.04 |
SD: standard deviation, ANAS: antinuclear antibodies.
Only 12.6% of the patients with highly probable group 3 PH had no risk factors, and 79% of them had two or more. Table 4 summarizes the characteristics of those in this group. For patients with highly probable PHT in Group 3, differences between the groups with and without risk factors are presented in Table 5, showing statistically significant differences restricted to puffy fingers (p=0.03).
Description of patients with group 3 PH. n=24.
| Variable | Frequency |
|---|---|
| Cardiac risk factors | |
| HT | 10 (41.6%) |
| Obesity | 1 (4.2%) |
| Diabetes mellitus | 2 (8.3%) |
| Atrial fibrillation | 1 (4.2%) |
| Coronary artery disease | 2 (8.4%) |
| Dyslipidemia | 3 (12.6%) |
| CKD | 3 (12.6%) |
| Ventricular hypertrophy | 2 (8.4%) |
| Diastolic dysfunction | 6 (25%) |
| No cardiovascular risk factors | 3 (12.6%) |
| Two or more risk factors | 19 (79%) |
HT: hypertension, CKD: chronic kidney disease.
Differences between groups with or without risk factors in patients with highly probable group 3 PH.
| Variable | Risk group | p | |
|---|---|---|---|
| With risk factors (n=21) | No risk factors (n=3) | ||
| Age (mean, SD) | 58 (12.7) | 52 (14.4) | 0.45 |
| Sex (women %) | 18 (85.7%) | 3 (100%) | 0.48 |
| Raynaud years (SD) | 9.1 (9.1) | 10.3 (9) | 0.82 |
| Clinical stage | 0.76 | ||
| Diffuse | 3 (14.3%) | 0 | |
| Limited | 11 (52%) | 2 (66.7%) | |
| Early | 7 (33.3%) | 1 (33.3%) | |
| Anti-centromeric antibodies | 11 (52.3%) | 1 (33.3%) | 0.53 |
| Anti SCL-70 | 3 (14.3%) | 1 (33.3%) | 0.4 |
| ANAS no centromeric pattern | 7 (33.3%) | 1 (33.3%) | 0.9 |
| Telangiectasias | 13 (65%) | 3 (100%) | 0.21 |
| Digital ulcers | 4 (19%) | 1 (33.3%) | 0.5 |
| Calcinosis | 3 (14.3%) | 1 (33.3%) | 0.4 |
| Puffy fingers | 11 (52.3%) | 0 | 0.03 |
| Articular disease | 9 (43%) | 5 (62.5%) | 0.57 |
| Gastrointestinal symptoms | 16 (76%) | 3 (100%) | 0.34 |
SD: standard deviation, ANAS: antinuclear antibodies.
This research is relevant because it describes a population of patients with systemic sclerosis and pulmonary hypertension of heterogeneous causes and the frequency of cardiovascular or pulmonary risk factors, which has not been described since the last guideline in 2022 was realized.
Estimates of both the incidence and prevalence of PH for patients with SSc differ depending on the population studied, the diagnostic methods used (echocardiography vs. right heart catheterization), and the criteria used to define cases of PH. By using echocardiography to diagnose PH based on a pulmonary artery systolic pressure (PASP) of ≥40mmHg, prevalence has been reported to be 28–32 percent in patients with SSc,11,12 comparable to our study with 29.3% for all causes of PH. When confirmed by RHC, the prevalence of WHO Group I PAH has been estimated to be 8–12 percent13, lower than the 17.5% presented now.
It was observed that one out of three patients had a form of early manifestation of the disease without evident cutaneous fibrosis on clinical examination, which makes it essential to establish the recommendation of early screening for pulmonary hypertension in patients with systemic sclerosis, especially those with early stages of the disease.
Similar to other studies,6,10–12 a heterogeneous distribution of pulmonary hypertension causes has been established, with 32% of the patients having extensive interstitial lung disease or impaired functional vital capacity and being classified as group 3 pulmonary hypertension, 3 patients with clear systolic heart disease, one with a high likelihood of chronic embolic disease, and finally 40 patients (59.7%) classified as group 1 pulmonary hypertension. As in the multicenter international registry PHAROS by Hinchcliff et al.,10 a wide variety of pulmonary hypertension causes have been identified in our study. In particular, the PHAROS registry is a multicenter registry that included 237 patients, the majority of whom were Caucasians, with right cardiac catheterization-confirmed pulmonary hypertension. In this research, 69% met the criteria for group 1 pulmonary hypertension, 10% met the criteria for group 2 pulmonary hypertension, and 21% were classified as group 3 pulmonary hypertension due to the presence of significant interstitial lung disease without left ventricular diastolic dysfunction.10 Our study confirms, as does the aforementioned publication, that patients with systemic sclerosis and pulmonary hypertension do not represent a homogeneous group in which there is only one cause of pulmonary hypertension but that it can be of mixed origin or have the concomitant presence of one or more causes.
The high prevalence of interstitial lung disease and diastolic dysfunction of the right ventricle found in this study might have implications for the modification or selection of treatment, such as the use of immunosuppressive therapy in the context of systemic sclerosis-related interstitial lung disease. In 128 patients with and without interstitial lung disease and pulmonary arterial hypertension diagnosed through right catheterization and followed prospectively, Chauvelot et al. discovered that interstitial lung disease is associated with a worse prognosis, increased mortality, and a poor therapeutic response.6
Currently, the cardiopulmonary risk phenotype in patients with pulmonary arterial hypertension is recognized to be of primary relevance.14,15 Current recommendations based on the sixth World Symposium on Pulmonary Hypertension recommend initiating treatment for pulmonary hypertension based on risk stratification.15 In the group of PAH patients studied in this article, 75% have one risk factor and 45% have two or more risk factors; therefore, the majority would not go for combination therapy but rather a therapy with a single drug, as this population is not well represented in the studies that served as the basis for the recommendations.16 We believe that the correct classification and stratification of cardiopulmonary risk in patients with pulmonary hypertension due to systemic sclerosis is crucial because it implies significant treatment modifications.17
Concerning patients with highly probable group 1 pulmonary hypertension, it was found that patients with risk factors had a statistically significant difference in the number of years affected by Raynaud's phenomenon, the frequency of anti-centromere antibodies, and the frequency of gastrointestinal symptoms, In this group of patients, the entire spectrum of the disease is included, encompassing both limited and diffuse cutaneous varieties, confirming that this complication affects a significant proportion. The above also has a high biological plausibility considering that Raynaud's phenomenon, which is an essential manifestation of vasculopathy in patients with systemic sclerosis, can be translated in the short and medium term into the appearance of pulmonary arterial hypertension, which is probably related to the development of increased vascular resistance by proliferation and vascular thickening18; a high frequency of digital ulcers was also observed, which is likely related to the development of increased vascular resistance by proliferation and vascular thickening; however, this difference did not reach statistical significance.
Patients with finger edema had a greater involvement of group 3 pulmonary arterial hypertension with the presence of risk factors, which corresponds to a novel description of the possible association between this clinical finding and the appearance of pulmonary arterial hypertension in this category.19 Finger edema is associated with a greater degree of inflammatory involvement of the connective tissue and interstitial lung disease, which may be correlated with the onset of group 3 hypertension.19,20 In 2012, Manetti et al.19 identified a correlation between matrix metalloproteinase 12 (MMP-12) expression and inflammation, fibrosis, and vascular tissue degradation.
The present study has limitations, the first of which is that the data obtained from the patients came from a single center; the second is that the data obtained by echocardiography could not be compared to the current diagnostic standard for pulmonary hypertension, which is right heart catheterization, even in patients with group I pulmonary hypertension, for whom this study is the gold standard; and the third limitation is the absence of prospective follow-up. A further limitation of the study is the current difficulty in classifying a patient with scleroderma at an early stage of the disease and the fact that this classification process is now being validated in international studies. Despite the absence of right heart catheterization, we believe that the present study has value in that it provides a clinical, demographic, serologic, and clinical description as well as a description of echocardiographic and hemodynamic characteristics of a condition of relevance in the context of systemic sclerosis patients.
FundingThis work has not received any funding.
Conflict of interestsThe authors declare that they have no conflict of interest.