Sarcoidosis is an inflammatory disease with unknown cause characterized by non-caseating granuloma formations. It may present with bilateral hilar lymphadenopathy, skin lesions, the involvement of eye and symptoms on the locomotor system. Gouty arthritis is an autoinflammatory disease characterized by hyperuricemia, recurrent arthritis attacks and the deposition of monosodium urate crystals in the joints and the surrounding tissues. We reported the coexistence of sarcoidosis and gouty arthritis in this paper.
La sarcoidosis es una enfermedad inflamatoria con causa desconocida caracterizada por formaciones de granulomas no caseificantes. Puede presentarse con linfadenopatía hiliar bilateral, lesiones cutáneas, afectación del ojo y síntomas en el sistema locomotor. La artritis gotosa es una enfermedad autoinflamatoria que se caracteriza por hiperuricemia, ataques recurrentes de artritis y la depósito de cristales de urato monosódico en las articulaciones y los tejidos circundantes. Presentamos la coexistencia de sarcoidosis y artritis gotosa en este trabajo.
Sarcoidosis is an inflammatory disease with unknown cause characterized by non-caseating granuloma formations. It may present with bilateral hilar lymphadenopathy, skin lesions, the involvement of eye and symptoms on the locomotor system.1
Gouty arthritis is an autoinflammatory disease which characterized by hyperuricemia, recurrent arthritis attacks and the deposition of monosodium urate crystals in the joints and surrounding tissues.2 Although the most common involvement is first MTP joints but it also may affect ankles, knees and shoulder joints. Usually it has been seen in the men and postmenopausal women and increases with increasing age.3
Although etiopathogenesis of sarcoidosis and gouty arthritis are different, some similar features are available (self-limiting recurrent arthritis attacks, good response to NSAIDs). While the inflammasome complex has an important role in the pathogenesis of the gouty arthritis, sarcoidosis are discussed will be also an autoinflammatory disease.4 Association of the gouty arthritis and sarcoidosis has been never reported in the literature and our case is the first in this regard.
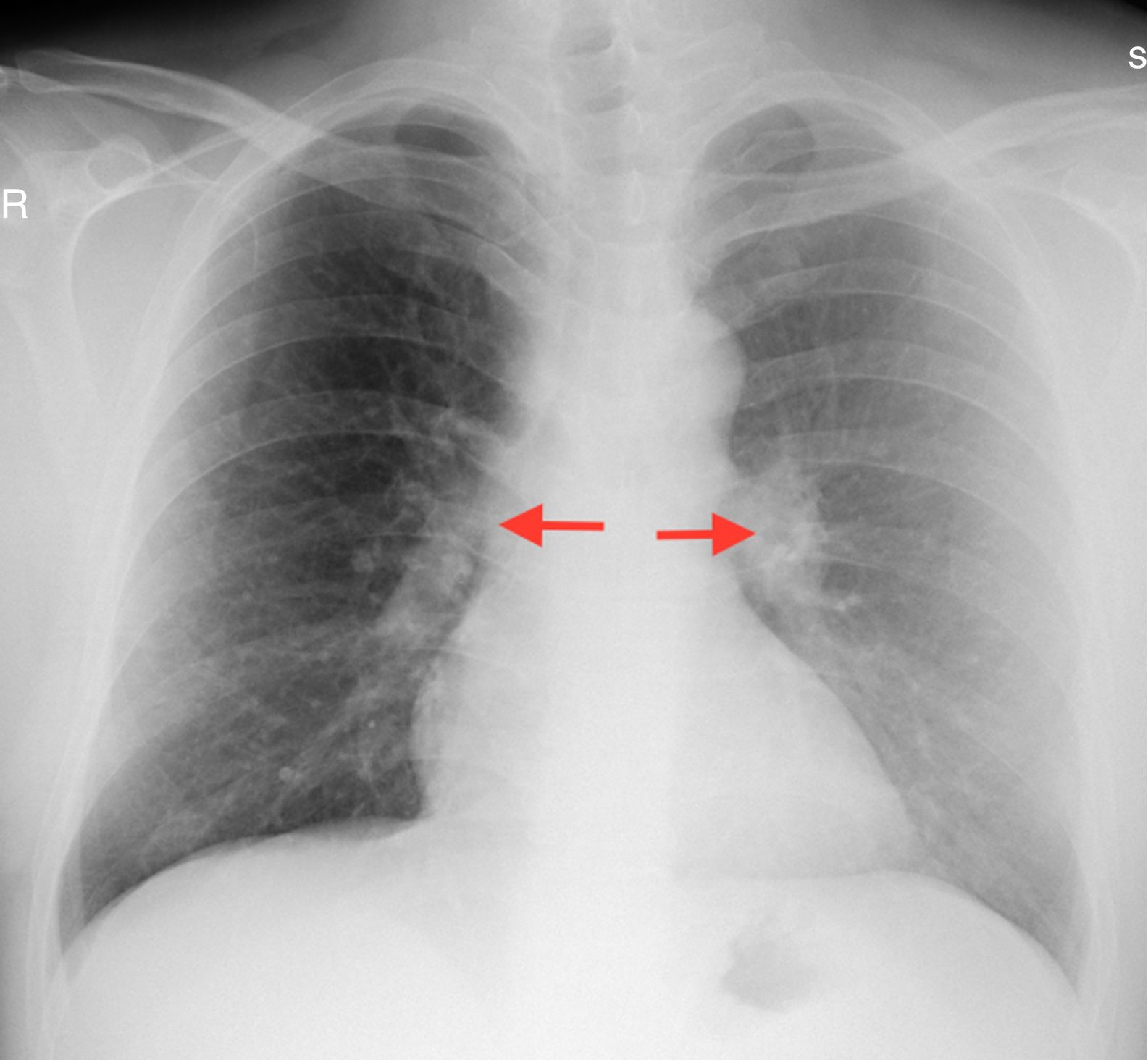
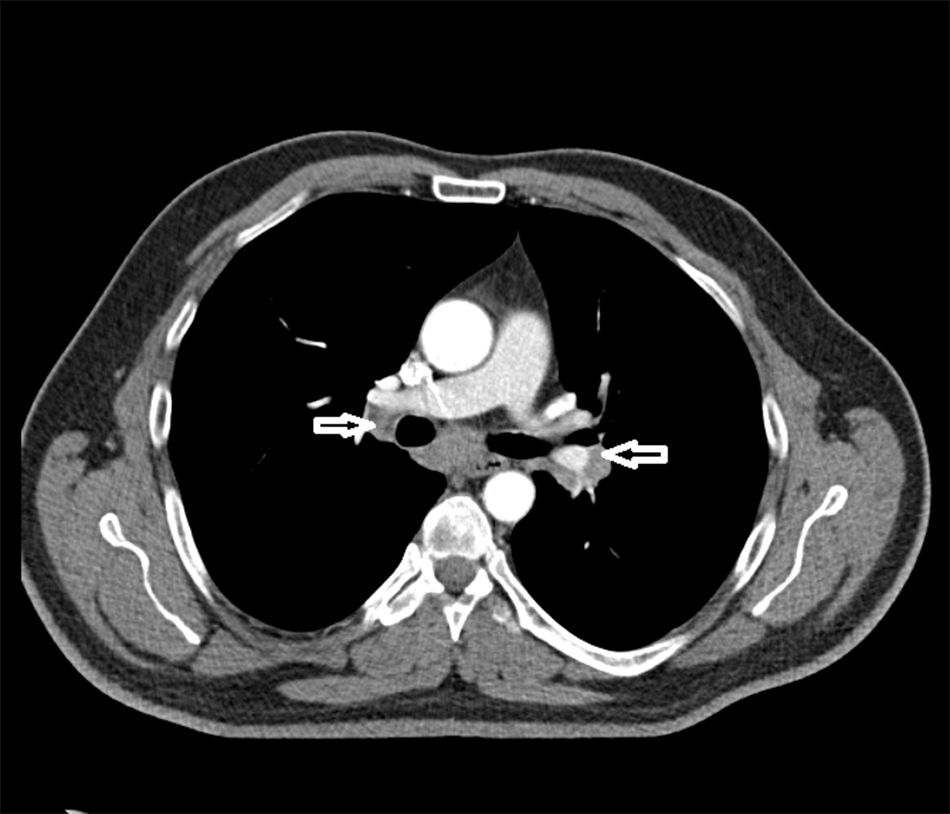
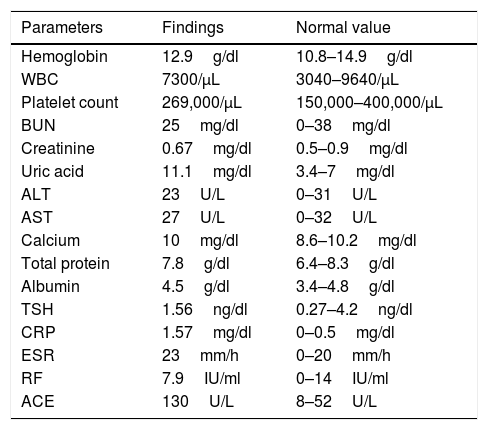
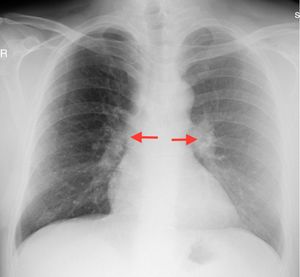
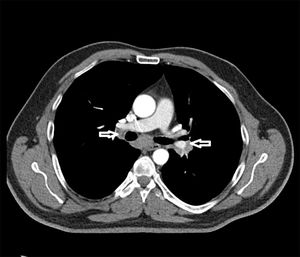
Case Report45 years old male patient diagnosed and follow-up with sarcoidosis applied to our clinic because of pain and swelling of the both ankle joints and swelling, redness and tenderness of the left first MTP joint. During examination, the patient described that previously had similar attacks in first MTP joints. Patient's physical examination showed; sensitivity of both ankle joints and swelling, redness and reduced range of motion of left first MTP joint. On laboratory tests; the acute phase reactants, serum uric acid and serum angiotensin converting enzyme (ACE) level were high (Table 1). On radiological examinations; there is no pathology on the radiograph of the ankle and toes except soft tissue swelling. Chest radiography showed enlargement in both hilar area (Fig. 1) while thorax CT showed bilateral hilar lymphadenopathy (Fig. 2). Abdominal ultrasound was normal. Serological tests was performed, negative results for rheumatoid factor (RF), antinuclear antibody (ANA), anti-cyclic citrullinated peptide antibody (anti-CCP Ab), anti-neutrophil cytoplasmic antibody (ANCA), anti-dsDNA were determined. Hepatitis markers (HBV, HCV, HIV) were normal. Monosodium urate (MSU) crystals were showed in the fluid analysis of the joint puncture. He has diagnosed with gouty arthritis and sarcoidosis according to clinical, laboratory and radiologic evaluations. Treatment with low-dose corticosteroids (prednisolone 4mg/day) and colchicine were initiated. One month later the patient complaints and laboratory findings were regressed. Six month later the radiological regression was observed on the control torax CT.
Laboratory Results of the Patient.
| Parameters | Findings | Normal value |
|---|---|---|
| Hemoglobin | 12.9g/dl | 10.8–14.9g/dl |
| WBC | 7300/μL | 3040–9640/μL |
| Platelet count | 269,000/μL | 150,000–400,000/μL |
| BUN | 25mg/dl | 0–38mg/dl |
| Creatinine | 0.67mg/dl | 0.5–0.9mg/dl |
| Uric acid | 11.1mg/dl | 3.4–7mg/dl |
| ALT | 23U/L | 0–31U/L |
| AST | 27U/L | 0–32U/L |
| Calcium | 10mg/dl | 8.6–10.2mg/dl |
| Total protein | 7.8g/dl | 6.4–8.3g/dl |
| Albumin | 4.5g/dl | 3.4–4.8g/dl |
| TSH | 1.56ng/dl | 0.27–4.2ng/dl |
| CRP | 1.57mg/dl | 0–0.5mg/dl |
| ESR | 23mm/h | 0–20mm/h |
| RF | 7.9IU/ml | 0–14IU/ml |
| ACE | 130U/L | 8–52U/L |
Abbreviations: WBC, white blood cells; BUN, blood urea nitrogen; ALT, alanine aminotransferase; AST, aspartate aminotransferase; TSH, thyroid stimulating hormone; CRP, C-reactive protein; ESR, erythrocyte sedimentation rate; RF, rheumatoid factor; ACE, angiotensin converting enzyme; BUN, blood urea nitrogen.
We diagnosed our patient with gouty arthritis because of the episodic form of attacks, the involvement of the first MTP joint which is a very typical for podagra and history of similar attacks previously. Also we determined the MSU crystals in the synovial fluid analysis which support the exact diagnosis. The joint involvement in the sarcoidosis may be seen in 10%–25% of cases. It affects most often the ankle joint, but knee, wrist, and metacarpophalangeal joints can also be involved.5 Acute gouty arthritis occurs as monoarthritis in 70% of patients and usually affects the first MTP joint.6 It can be confused with erysipelas and/or with lymphangitis because of the redness in the joints. Arthritis episodes regressed spontaneously in nearly one week or response well to colchicine treatment.7 Sarcoid arthritis and gouty arthritis may coexist as in our case, but sometimes acute sarcoid arthritis can also mimic gouty arthritis. This coexistence may be purely coincidental and/or related to a common etiopathogenesis. Gouty arthritis is an autoinflammatory disease, which is associated with inflammasome complex. However, there are hypothesis supporting that sarcoidosis may be autoinflammatory disease as well as gouty arthritis.8 Hyperuricemia is a important finding in both diseases and sometimes lead to confusion in the true diagnosis. In sarcoidosis patients hyperuricemia is probably due to the defects of urate metabolism. The presence of the phagocytosed monosodium urate crystals in the synovial fluid is important for the diagnosis of acute gouty arthritis.
In conclusion, we report herein a case with sarcoidosis coexist with gouty arthritis. Both diseases may have similar clinical manifestations and exact diagnosis is important for prognosis and treatment. Factors such as prevalence data, absence of genetic relationship and response to treatment support the theory of coexistence rather than of common pathogenesis. Multicentric studies that may shed light on this subject are needed.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of InterestThe authors declare that they have no conflict of interest.