Sarcoidosis is a chronic inflammatory disease with unknown etiology, characterized by non-caseating granuloma formation. Extrapulmonary involvement is usually seen in locomotor system, skin, lymph nodes, eyes and liver, but could be in any organ.1 Sarcoid involvement of the endocrine glands has rarely been observed.2 The incidence of thyroid autoimmune disease has been reported in patients with sarcoidosis in various studies, but comorbidity of Graves’ disease (GD) is not common. Comorbidity of sarcoidosis and GD has been described in this paper.
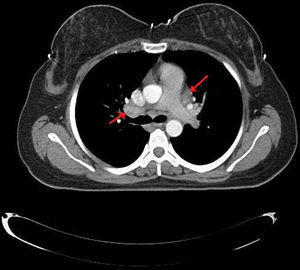
Case presentationA 35-year-old female patient was admitted to our Rheumatology clinic with complaints of pain and swelling in the ankle joint, morning stiffness, fatigue, dry cough, and palpitations. Physical examination revealed findings related with right ankle arthritis, growth and tenderness of the thyroid gland in palpation and tachycardia in cardiac auscultation. As for thyroid function tests; we determined FT3: 14.27pg/ml (normal 2.0–4.4pg/ml), FT4: 5.25ng/dl (normal 0.93–1.7ng/dl), TSH: 0.01ng/dl (normal 0.27–4.2ng/dl), anti-thyroglobulin: 164.7IU/ml (normal 0–115IU/ml), anti-TPO: 7.10IU/ml (normal 0–34IU/ml), TSH receptor antibody: 12.77IU/L (normal<1.22IU/L). Serum ACE level was found as 89 (normal <35). In the serological tests; ANA, ANCA, anti-CCP, RF were found to be negative. Thoracic CT revealed mediastinal and bilateral hilar lymphadenopathy (Fig. 1). The chest disease specialist was contacted, endobronchial ultrasound (EBUS) guided biopsy was performed. Histopathological evaluation showed non-caseating granulomas, thus sarcoidosis was considered in the patient. Thyroid ultrasonography showed the increased size of the thyroid gland, with heterogeneous and coarse parenchyma, which appeared to be related with Graves’ disease. Diffusely increased uptake of radioactive iodine was found in thyroid scintigraphy. The patient was diagnosed with sarcoidosis and Graves’ disease based on clinical, laboratory, radiological and histological data. Moderate dose of a corticosteroid (40mg/day) and propylthiouracil 3×1/day were initiated to the patient. At the 6th month of clinical follow-up, thyroid function tests were observed to be normalized, palpitations and complaints of locomotor system were found to be decreased. Control thorax CT showed significant regression in terms of mediastinal and hilar lymphadenopathy.
DiscussionSarcoidosis is a multisystemic, chronic granulomatous disease with unknown etiology, characterized by non-caseating granuloma formation. Sarcoid involvement of the thyroid gland has been detectedupon autopsy or fine needle aspiration biopsy and thyroidectomy.3 Graves’ disease is an autoimmune disease in which activated T and B cells can cause intrathyroidal lymphocytic infiltrations.4 Graves’ disease was shown in a case of sarcoidosis, although hyperthyroidism is considered rare.5 On the other hand, Graves’ disease in patients with sarcoidosis may be simply coincidental. Goiter, subacute thyroiditis and thyroid cancer have been reported among other thyroid disorders accompanying sarcoidosis.6 In a Swedish study, significantly elevated levels of antithyroglobulin autoantibodies have been reported in patients with sarcoidosis.7 Nakamura et al. have reported that the prevalence of sarcoidosis related with Hashimoto's thyroiditis was 3–11%, much more common than other thyroid diseases.8 In another study, antithyroglobulin autoantibodies were significantly higher in patients with sarcoidosis, but the basic thyroid function tests were in the normal range.9 However, comorbidity of sarcoidosis of the thyroid gland and Graves’ disease has rarely been reported.10,11 Karlish and McGregor have reported that hyperthyroidism developed in 6 patients with sarcoidosis but long-acting thyroid stimulating antibodies could not be detected.12
As a result, based on clinical, radiological and histopathological examinations, we hereby report the comorbidity of Graves’ disease and sarcoidosis in our patient. Since both are chronic and inflammatory diseases, this suggests that they may have a common etiopathogenesis and/or it may be just a coincidence. Further studies on this topic are required.