The association between dermatomyositis (DM) and neoplasm has been widely described, especially in elder patients; this entity can be associated with many different types of tumours, more frequently lung, ovary, and gastric cancers. There is no clear association with central nervous system tumours. We present the case of a 64-year-old woman diagnosed simultaneously of DM with a difficult clinical control and a meningioma, being the course of the two illnesses linked. The activity of the DM was controlled after the meningioma was removed.
La asociación entre la dermatomiositis (DM) y las neoplasias ha sido ampliamente descrita, especialmente en pacientes de edad avanzada; esta entidad puede estar asociada con diferentes tipos de tumores, especialmente con cáncer de pulmón, ovario y estómago. No existe una clara asociación con tumores en el sistema nervioso. Se presenta el caso de una mujer de 64 años a la que se diagnosticó simultáneamente DM de difícil control clínico y un meningioma, estando el curso de ambas enfermedades vinculadas. La actividad de la DM fue controlada tras la extracción del meningioma.
The link between DM and malignancies has been clarified.1 The reported rate of malignant diseases in DM has varied from 6 to 60%, with most large population-based cohort studies reporting a rate of 20–25%.2 The most common cancers are those of the ovaries, gastrointestinal tract, lung, breast, and non-Hodgkin lymphomas.3–5 A review of the literature revealed only two cases of meningioma in patients with DM.6,7
Case reportA 64-year-old woman was admitted to the hospital because of cutaneous rash and muscle weakness. She had been well until three months before; she noted weakness in her legs, while climbing stairs, and in her arms. The physical examination revealed a violaceous periorbital oedema. There were areas of erythema over the proximal and distal interphalangeal joints. Neurological examination revealed bilateral symmetric muscle weakness affecting the shoulders and hip girdle muscles, with strength assessed at 3 of 5 bilaterally. The patient could not stand up from a sitting position. The deep-tendon reflexes were normal and symmetric in arms and legs. The rest of the examination did not reveal abnormalities.
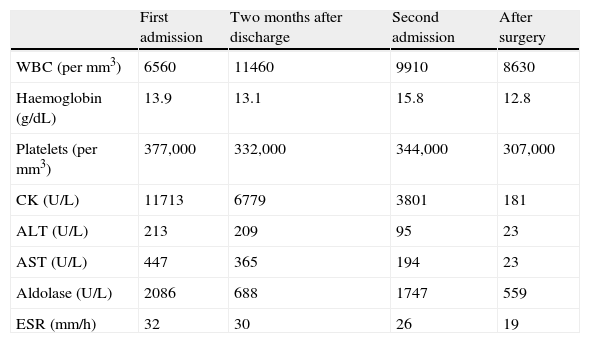
General laboratory investigations are shown in Table 1. The results of urinalysis were normal. An antinuclear-antibody test was positive at 1:1560 in a homogeneous pattern; anti-double stranded DNA, anti-ENA, anti Jo-1 antibodies and ANCA were negative. Radiographs of the chest and ultrasonography of the abdomen were normal. A barium study of the oesophagus, stomach, and duodenum only showed decreased motility in the proximal oesophagus. The electromyography showed profuse denervation activity (fibrillations and positive waves) in all the muscles explored, especially in proximal muscles of upper limbs. Polyphasic motor unit, low amplitude and average duration, high-frequency complex potential abnormalities, consistent with myositis. Histological examination of a biopsy from deltoid muscle demonstrated necrosis of types I and II muscle fibres, phagocytosis, regeneration with basophilia, and atrophy in a perifascicular distribution. Treatment with prednisone (60mg/day) was started with subjective improvement in muscle strength and dysphagia. The patient was discharged from hospital, however, with inability to stand up from a sitting position without help. Following clinical improvement, the dosage of prednisone was slowly tapered during the successive months to a daily maintenance dose of 10mg/day; azathioprine was added early to save corticosteroids, however, muscle strength was not totally recovered.
Laboratory tests.
| First admission | Two months after discharge | Second admission | After surgery | |
| WBC (per mm3) | 6560 | 11460 | 9910 | 8630 |
| Haemoglobin (g/dL) | 13.9 | 13.1 | 15.8 | 12.8 |
| Platelets (per mm3) | 377,000 | 332,000 | 344,000 | 307,000 |
| CK (U/L) | 11713 | 6779 | 3801 | 181 |
| ALT (U/L) | 213 | 209 | 95 | 23 |
| AST (U/L) | 447 | 365 | 194 | 23 |
| Aldolase (U/L) | 2086 | 688 | 1747 | 559 |
| ESR (mm/h) | 32 | 30 | 26 | 19 |
WBC: white blood cells; ALT: alanine-aminotransferase; AST: aspartate-aminotransferase; CK: creatine-kinase; ESR: erythrocyte sedimentation rate.
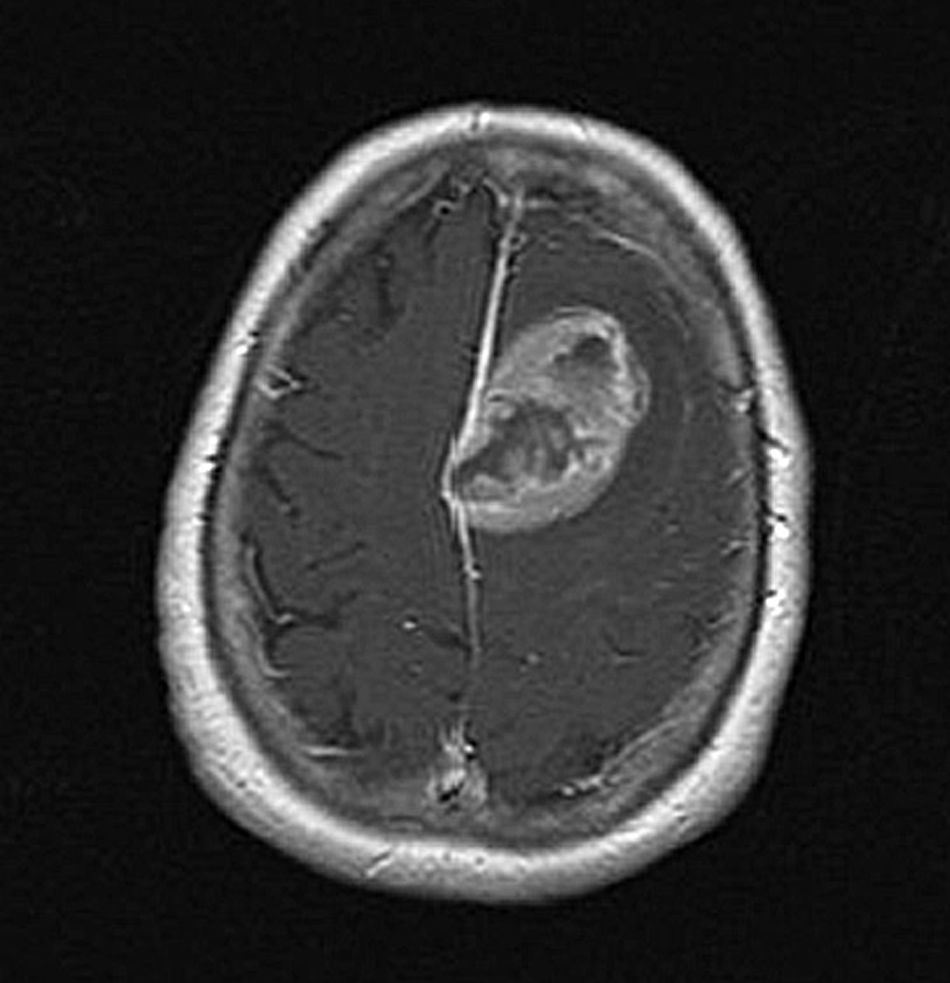
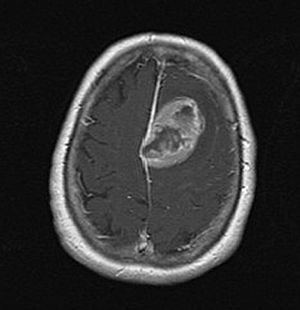
Ten months after the onset of the disease, a flare requiring hospitalisation appeared. The laboratory test results at that point are listed in Table 1. The electromyography showed a severe myopathic pattern. All tumoral markers were negative; chest, abdomen and pelvic scanner only showed renal litiasis. Consequently, the dose of prednisone was increased to 60mg/day without any clinical or biochemical improvement. The patient was treated with three bolus of methylprednisolone (1g/day) but her muscle strength did not increase. Three weeks after the admission, the patient developed right facial central paresis, right arm hyperreflexia, and disartria. MRI (Fig. 1) revealed the presence of a left frontal mass that was removed. The histology showed a fibroblastic type meningioma. After the surgical removal of the tumour, the patient improved dramatically and the muscle enzyme levels returned to normality. The patient continued her treatment with methotrexate (10mg weekly) and prednisone (10mg/day), being asymptomatic so far.
DiscussionThe association between DM and cancer has been recognized for many years; several studies in large populations have shown that patients with DM have a risk of cancer three to six times higher than the general population.1,2,4 Generalized cancer screening is now recommended for all patients with inflammatory myositis, especially for those who are at increased risk such as older patients, those suffering dermatomyositis rather than polymyositis, cases with evidence of capillary damage detected by muscle biopsy, dermatomyositis complicated with cutaneous necrosis of the trunk, presence of cutaneous leukocytoclastic vasculitis, elevated erythrocyte sedimentation rate, presence of antinuclear antibodies, and in patients with weight loss.8,9 Malignant diseases may occur before the onset of DM, concurrently or after the onset of the symptoms. In addition, the DM might follow the course of the malignant disease (a paraneoplasic course) or may follow its own course independently of the treatment of the tumour. Studies showing benefits of cancer surgery on DM and those showing no link have been reported.1,6
About 15% of adults with DM have been found to develop a tumour. Meningioma also has a frequency of 13–26% among the various intracraneal tumours affecting the general population.10 However, despite the fact of the relatively high incidence of meningioma, the combination of this tumour and DM has been described in two reports.6,7 There is not even a described association between primary brain tumours and DM.
Our report does not prove the association between these two entities, but the patient's improvement after the removal of meningioma and the difficulty to control her disease activity previously suggest that these two entities might be associated in this case.
ConclusionThe association between dermatomyositis (DM) and neoplasms has been widely described, but there is no clear association with central nervous system tumours. In this paper, we show a not previously described case of meningioma in a patient with DM.
Conflict of interestThe authors have no conflict of interest to declare.