Magnetic resonance imaging (MRI) sensitivity and specificity seem to be less studied in enthesitis-related arthritis (ERA).
We aimed to determine the ability of sacroiliac MRI to diagnose ERA patients.
Materials and methodsWe conducted a retrospective study including 44 patients with juvenile idiopathic arthritis (JIA). Each patient had a sacroiliac joint MRI. We divided patients into two groups: G1 patients with ERA and G2 patients with non-ERA subtype.
ResultsERA was noted in 61% of the cases. Sacroiliac joints were painful in 15 patients (34%). MRI was normal in 25 patients (57%) (G1:11 versus G2:14) and showed bone marrow edema in the sacroiliac joints in 19 patients (34%) (G1=16 versus G2=3, p=0.005).
Sacroiliac joints MRI's sensitivity and specificity in the ERA diagnosis were 61.54% and 82.35%, respectively. Positive and negative predictive values were 84.21% and 58.33%, respectively. Furthermore, sacroiliac joint pain in the clinical examination was able to predict sacroiliac bone edema in MRI with an odds ratio of 6.8 (95% CI 1.68–28.09; p=0.006).
ConclusionOur study showed that sacroiliac joint MRI has good specificity and positive predictive value in the diagnosis of ERA patients among JIA patients. This underlines the usefulness of sacroiliac joint MRI in the early diagnosis of ERA patients.
La sensibilidad y especificidad de la resonancia magnética parecen estar menos estudiadas en la artritis relacionada con entesitis (ERA).
Nuestro objetivo era determinar la capacidad de la resonancia magnética de la articulación sacroilíaca para diagnosticar pacientes con ERA.
Materiales y métodosRealizamos un estudio retrospectivo que incluyó a 44 pacientes con artritis idiopática juvenil (AIJ). A cada paciente se le realizó una resonancia magnética de la articulación sacroilíaca. Dividimos a los pacientes en dos grupos: G1: pacientes con ERA y G2: pacientes con subtipo no ERA.
ResultadosSe observó ERA en 61% de los casos. Las articulaciones sacroilíacas resultaron dolorosas en 15 pacientes (34%). La resonancia magnética fue normal en 25 pacientes (57%) (G1:11 vs. G2:14) y mostró edema de médula ósea en las articulaciones sacroilíacas en 19 pacientes (34%) (G1=16 vs. G2=3, p=0,005).
La sensibilidad y especificidad de la resonancia magnética de articulaciones sacroilíacas en el diagnóstico de ERA fueron de 61,54 y 82,35%, respectivamente. Los valores predictivos positivos y negativos fueron 84,21 y 58,33%, respectivamente. Además, el dolor en la articulación sacroilíaca en el examen clínico fue capaz de predecir el edema del hueso sacroilíaco en la resonancia magnética con un odds ratio de 6,8 (IC 95%: 1,68 a 28,09; p=0,006).
ConclusiónNuestro estudio demostró que la resonancia magnética de la articulación sacroilíaca tiene buena especificidad y valor predictivo positivo en el diagnóstico de pacientes con ERA entre pacientes con AIJ. Esto subraya la utilidad de la resonancia magnética de la articulación sacroilíaca en el diagnóstico temprano de pacientes con ERA.
Juvenile idiopathic arthritis (JIA) is a wide-ranging group of diseases affecting children under the age of 16 years.1 Its prevalence varies between 0.07 and 4.01 per 1000 children.2 Enthesitis-related arthritis (ERA) is one of the JIA subtypes. It accounts for 20% of JIA children.3 Boys are more affected by this rheumatism.4 Like adult spondyloarthritis, a genetic predisposition by Human Leukocyte Antigen B27 (HLA-B27) was noted in 50–80% of ERA patients.5–7
This disease manifests by enthesitis and arthritis, occurring predominantly in the lower limbs.8 Hip involvement is the most severe articular involvement in ERA and could lead to an important functional impairment.9,10
The axial skeleton is also involved, but contrary to adults spondyloarthritis occurs in only 30% of children within 15 months of diagnosis and was often asymptomatic.8,11–13
Despite the progress in the treatment of JIA, ERA seems to have a poorer prognosis and worse health status outcomes than the other JIA subtypes.14,15 Besides, severe extra-articular manifestations, such as anterior uveitis are not rare in ERA patients.16 Hence, it is important to diagnose this disease early. Unfortunately, the diagnosis of ERA is not always obvious or easy. According to the International League of Associations for Rheumatology (ILAR) classification ERA diagnosis based on only clinical and laboratory findings.17 Yet, these criteria do not allow the diagnosis of all the ERA patients, especially with axial involvement.18 Recently, the European League Against Rheumatism (EULAR)-Pediatric Rheumatology European Society (PReS) task force has proposed a consensus-based recommendation on the use of imaging in the JIA diagnosis.19
According to this evidence, magnetic resonance imaging (MRI) of sacroiliac joints has shown increasing interest in the ERA diagnosis.18 However, unlike the adult data, the value of MRI to detect abnormalities in children remains challenging.
There is little information on the value of this imaging in the ERA diagnosis and even less in patients with silent axial involvement.
Thus, we aimed to determine the ability of sacroiliac joints MRI to diagnose ERA patients and study the predictive factors of the presence of MRI inflammatory lesions.
Materials and methodsPatientsWe conducted a retrospective study including consecutive patients followed for JIA, recruited from the outpatient clinic of the pediatric rheumatology department. We divided the included patients into two groups using the ILAR 2001 criteria17: G1 including ERA patients and G2 including other JIA subtypes (oligo articular, poly articular rheumatoid factor (+) or (−), undifferentiated form, and systemic JIA).
Inclusion criteriaWe included patients fulfilling the ILAR 2001 criteria.17 ILAR defines JIA as chronic arthritis (≥6 weeks) with no known cause occurring in children before the age of 16 years old.17 JIA is categorized into seven subtypes based on the number of active joints, extra-articular manifestations, and serology recognized in the first 6 months of disease presentation.17 All the included patients underwent the SI MRI.
We also checked that all the patients were not receiving non-steroidal anti-inflammatory drugs (NSAIDs) or receiving biological disease modifying anti-rheumatic drugs (bDMARDs) 15 days before performing the MRI scan.
Clinical assessmentDemographic and clinical data of the patients, including age, gender, and body mass index (BMI) were collected. The following JIA characteristics were also collected: age at disease onset, disease duration, extra-articular manifestations (uveitis and psoriasis), and therapeutic management (NSAIDs, conventional synthetic DMARDs (csDMARDs), and bDMARDs).
Disease activity was assessed using the Juvenile Arthritis Disease Activity Score using C-reactive protein in 10 joints (JADAS-CRP-10)20 for all the patients, and the Juvenile Spondyloarthritis Disease Activity score (JSpADA) for ERA patients.21,22
Biological assessmentErythrocyte sedimentation rate (ESR) and CRP were measured. A normal CRP was defined as less than 6mg/L, however ESR was considered as normal if the value was under Age/2 in boys and Age+10/2 in girls.
Magnetic resonance imaging assessmentAll the patients had a pelvic MRI. MRI sequences included T1-weighted sequence, a water-sensitive sequence (short tau inversion recovery (STIR)), and a T2-weighted fat-saturated (FS) sequence. The Outcome Measures Rheumatoid Arthritis Clinical (OMERACT) recommendations (OMERACT) pediatric JAMRIS (Juvenile Idiopathic Arthritis MRI Score) scoring system was used for the interpretation of the MRI lesions.23
Bone marrow edema (BME) was defined as the presence of hyper intense signal on both T2-weighted FS and STIR sequences.24
The MRI interpretation was performed by a board-certified radiologist trained in pediatric musculoskeletal imaging.
Statistical analysisStatistical analysis was performed using the Statistical Package for Social Sciences (SPSS) software version 25. We used descriptive statistics to study the characteristics of the population. Quantitative variables were tested for normal distribution using the Kolmogorov–Smirnov test. We calculated the median and variance of data with no Gaussian distribution and the mean with standard deviation in quantitative variables with normal curve.
A Student's t-test was used for normally distributed groups and Mann–Whitney U test was used for non-normally distributed groups to compare continuous variables between the groups. We also performed t-tests to compare continuous variables and Chi-square test to assess the association between two categorical variables. Correlations were assessed using Pearson and Spearman's methods depending on data distribution. We calculated the sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of MRI to diagnose G1 from G2. Statistical significance was defined by a p-value ≤0.05.
Ethical considerationsOur study was conducted according to the Helsinki Declaration. The study was approved by the ethics committee of the hospital. Verbal consent was approved for each participant after explaining the aims of the study.
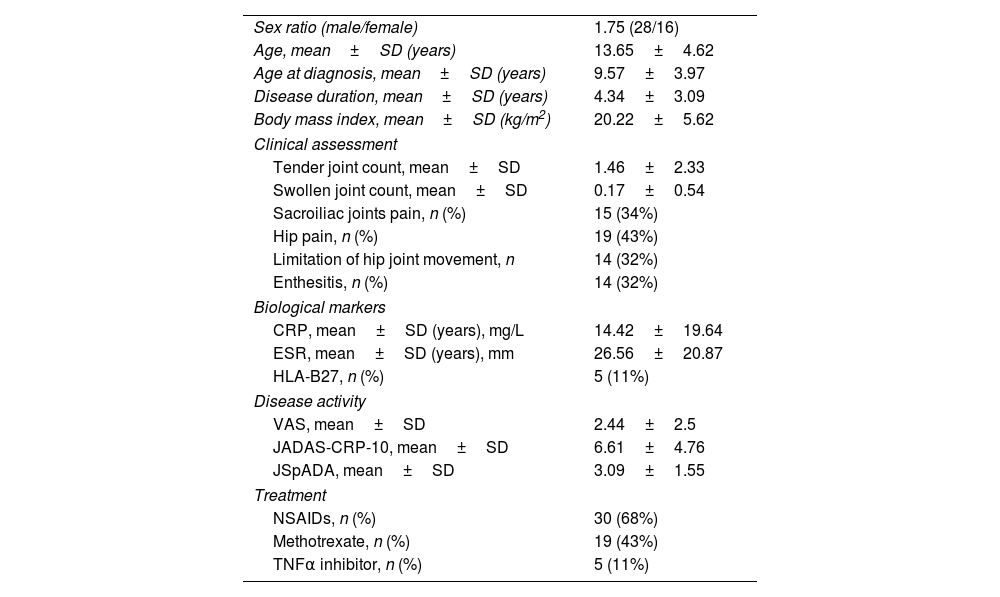
ResultsDemographic, clinical, and biological characteristics of patientsWe included 44 patients. ERA was noted in 61% of the cases (n=27). Other JIA subtypes (n=17, 39%) were: oligoarticular in 6 cases (14%), polyarticular in 5 cases (11%), psoriatic arthritis and undifferentiated JIA in 3 cases (7%) each. Patient characteristics are summarized in Table 1. The comparison between G1 and G2 characteristics is summarized in Table 2.
Characteristics of the population studied.
| Sex ratio (male/female) | 1.75 (28/16) |
| Age, mean±SD (years) | 13.65±4.62 |
| Age at diagnosis, mean±SD (years) | 9.57±3.97 |
| Disease duration, mean±SD (years) | 4.34±3.09 |
| Body mass index, mean±SD (kg/m2) | 20.22±5.62 |
| Clinical assessment | |
| Tender joint count, mean±SD | 1.46±2.33 |
| Swollen joint count, mean±SD | 0.17±0.54 |
| Sacroiliac joints pain, n (%) | 15 (34%) |
| Hip pain, n (%) | 19 (43%) |
| Limitation of hip joint movement, n | 14 (32%) |
| Enthesitis, n (%) | 14 (32%) |
| Biological markers | |
| CRP, mean±SD (years), mg/L | 14.42±19.64 |
| ESR, mean±SD (years), mm | 26.56±20.87 |
| HLA-B27, n (%) | 5 (11%) |
| Disease activity | |
| VAS, mean±SD | 2.44±2.5 |
| JADAS-CRP-10, mean±SD | 6.61±4.76 |
| JSpADA, mean±SD | 3.09±1.55 |
| Treatment | |
| NSAIDs, n (%) | 30 (68%) |
| Methotrexate, n (%) | 19 (43%) |
| TNFα inhibitor, n (%) | 5 (11%) |
SD: standard deviation; ESR: erythrocyte sedimentation rate; CRP: C-reactive protein; n: number; NR: normal range; HLA-B27: Human Leukocyte Antigen B27; JADAS: Juvenile Arthritis Disease Activity Score; JSpADA: Juvenile Spondyloarthritis Disease Activity score; VAS: Visual Analog Scale; NSAIDs: non-steroidal anti-inflammatory drugs; TNFα: tumor necrosis factor α.
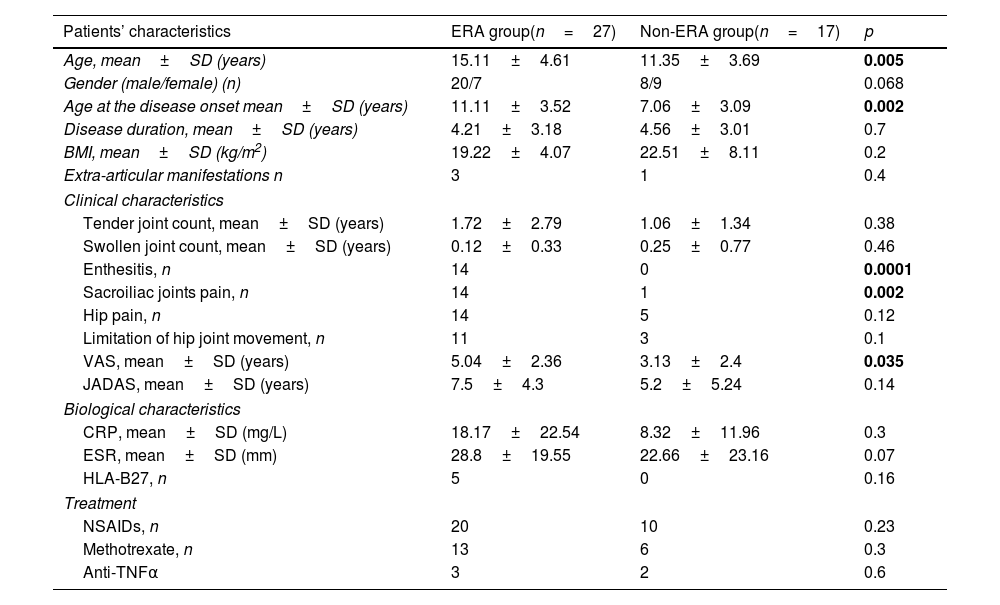
Comparison between ERA patients and non-ERA patients’ characteristics.
| Patients’ characteristics | ERA group(n=27) | Non-ERA group(n=17) | p |
|---|---|---|---|
| Age, mean±SD (years) | 15.11±4.61 | 11.35±3.69 | 0.005 |
| Gender (male/female) (n) | 20/7 | 8/9 | 0.068 |
| Age at the disease onset mean±SD (years) | 11.11±3.52 | 7.06±3.09 | 0.002 |
| Disease duration, mean±SD (years) | 4.21±3.18 | 4.56±3.01 | 0.7 |
| BMI, mean±SD (kg/m2) | 19.22±4.07 | 22.51±8.11 | 0.2 |
| Extra-articular manifestations n | 3 | 1 | 0.4 |
| Clinical characteristics | |||
| Tender joint count, mean±SD (years) | 1.72±2.79 | 1.06±1.34 | 0.38 |
| Swollen joint count, mean±SD (years) | 0.12±0.33 | 0.25±0.77 | 0.46 |
| Enthesitis, n | 14 | 0 | 0.0001 |
| Sacroiliac joints pain, n | 14 | 1 | 0.002 |
| Hip pain, n | 14 | 5 | 0.12 |
| Limitation of hip joint movement, n | 11 | 3 | 0.1 |
| VAS, mean±SD (years) | 5.04±2.36 | 3.13±2.4 | 0.035 |
| JADAS, mean±SD (years) | 7.5±4.3 | 5.2±5.24 | 0.14 |
| Biological characteristics | |||
| CRP, mean±SD (mg/L) | 18.17±22.54 | 8.32±11.96 | 0.3 |
| ESR, mean±SD (mm) | 28.8±19.55 | 22.66±23.16 | 0.07 |
| HLA-B27, n | 5 | 0 | 0.16 |
| Treatment | |||
| NSAIDs, n | 20 | 10 | 0.23 |
| Methotrexate, n | 13 | 6 | 0.3 |
| Anti-TNFα | 3 | 2 | 0.6 |
SD: standard deviation; ESR: erythrocyte sedimentation rate; CRP: C-reactive protein; n: number; NR: normal range; HLA-B27: Human Leukocyte Antigen B27; JADAS: Juvenile Arthritis Disease Activity Score; VAS: Visual Analog Scale; NSAIDs: non-steroidal anti-inflammatory drugs; TNFα: tumor necrosis factor α; p: probability value.
p-values ≤0.05 are in bold.
MRI showed BME in the sacroiliac joints in 19 patients (34%): G1=16 (84%) versus G2=3 (16%), p=0.005.
Erosions and irregularities of sacroiliac joints were noted in 4 ERA patients (9%). Intra-articular effusion of sacroiliac joints was noted in one oligo articular patient. Spinal MRI was performed in four children. It showed BME in vertebral corners in 3 patients (7%). These patients had a final ERA diagnosis.
Furthermore, hip lesions on MRI were noted in 26 patients (59%): G1=17 (65%) versus G2=9 (35%), p=0.21. These lesions were: synovitis in 39% (n=17), subchondral BME in 27% (n=12), intra-articular effusion in 27% (n=12), joint space narrowing 14% of the cases (n=6), and enthesitis in 7% (n=3).
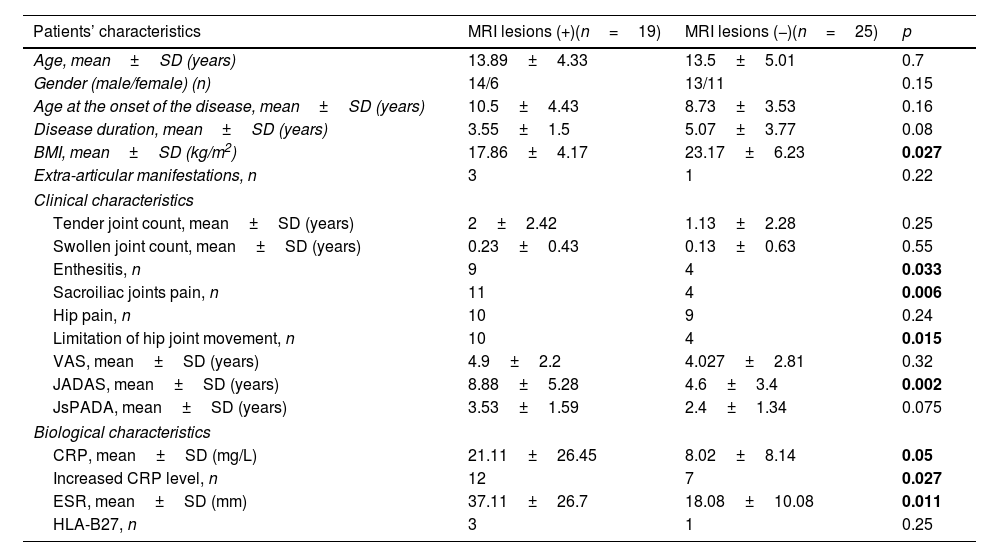
Associations between sacroiliac joints MRI lesions and JIA characteristicsAs shown in Table 3, sacroiliac joints MRI lesions were associated with the following parameters: clinical enthesitis, hip joint limitation, increased CRP level, higher ESR, higher JADAS, and lower body mass index (BMI).
Association between sacroiliac joints MRI lesions and JIA characteristics.
| Patients’ characteristics | MRI lesions (+)(n=19) | MRI lesions (−)(n=25) | p |
|---|---|---|---|
| Age, mean±SD (years) | 13.89±4.33 | 13.5±5.01 | 0.7 |
| Gender (male/female) (n) | 14/6 | 13/11 | 0.15 |
| Age at the onset of the disease, mean±SD (years) | 10.5±4.43 | 8.73±3.53 | 0.16 |
| Disease duration, mean±SD (years) | 3.55±1.5 | 5.07±3.77 | 0.08 |
| BMI, mean±SD (kg/m2) | 17.86±4.17 | 23.17±6.23 | 0.027 |
| Extra-articular manifestations, n | 3 | 1 | 0.22 |
| Clinical characteristics | |||
| Tender joint count, mean±SD (years) | 2±2.42 | 1.13±2.28 | 0.25 |
| Swollen joint count, mean±SD (years) | 0.23±0.43 | 0.13±0.63 | 0.55 |
| Enthesitis, n | 9 | 4 | 0.033 |
| Sacroiliac joints pain, n | 11 | 4 | 0.006 |
| Hip pain, n | 10 | 9 | 0.24 |
| Limitation of hip joint movement, n | 10 | 4 | 0.015 |
| VAS, mean±SD (years) | 4.9±2.2 | 4.027±2.81 | 0.32 |
| JADAS, mean±SD (years) | 8.88±5.28 | 4.6±3.4 | 0.002 |
| JsPADA, mean±SD (years) | 3.53±1.59 | 2.4±1.34 | 0.075 |
| Biological characteristics | |||
| CRP, mean±SD (mg/L) | 21.11±26.45 | 8.02±8.14 | 0.05 |
| Increased CRP level, n | 12 | 7 | 0.027 |
| ESR, mean±SD (mm) | 37.11±26.7 | 18.08±10.08 | 0.011 |
| HLA-B27, n | 3 | 1 | 0.25 |
SD: standard deviation; (+): presence; (−): absence; n: number; ESR: erythrocyte sedimentation rate; CRP: C-reactive protein; HLA-B27: Human Leukocyte Antigen B27; JADAS: Juvenile Arthritis Disease Activity Score; JSpADA: Juvenile Spondyloarthritis Disease Activity score; VAS: Visual Analog Scale; p: probability value.
p-values ≤0.05 are in bold.
Furthermore, sacroiliac joint pain in the clinical examination was able to predict sacroiliac bone edema in MRI with an odds ratio of 6.8 (95% CI 1.68–28.09; p=0.006).
Diagnostic value of MRI in the diagnosis of ERAFourteen patients (51.8%) with ERA had a sacroiliac pain in clinical exam. Sixteen (59.25%) had SI MRI lesions. These lesions were BME in all patients. Painful SI in clinical examination, positive SI MRI, and presence of BME were suggestive of ERA diagnosis.
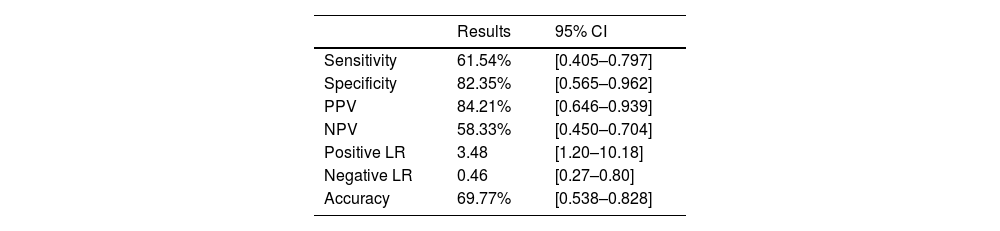
The sensitivity, specificity, positive predictive value, and negative predictive of the sacroiliac joints MRI lesions (BME and/or erosions) in the diagnosis of ERA are represented in Table 4.
Sensitivity, specificity, positive predictive value, and negative predictive of the sacroiliac joints. Magnetic resonance imaging lesions (bone marrow edema and/or erosions) in the diagnosis of enthesitis-related arthritis.
| Results | 95% CI | |
|---|---|---|
| Sensitivity | 61.54% | [0.405–0.797] |
| Specificity | 82.35% | [0.565–0.962] |
| PPV | 84.21% | [0.646–0.939] |
| NPV | 58.33% | [0.450–0.704] |
| Positive LR | 3.48 | [1.20–10.18] |
| Negative LR | 0.46 | [0.27–0.80] |
| Accuracy | 69.77% | [0.538–0.828] |
CI: confidence interval; PPV: positive predictive value; NPV: negative predictive value; LR: likelihood ratio.
Sacroiliitis in MRI is frequent in ERA patients. Its prevalence varies between 20% and 88% of the patients in the literature.11,25–27 In our study, the ERA patients had a positive SI MRI scan and a painful SI in clinical examination in 59.2% (n=16) and 51.8% (n=14), respectively.
Many authors demonstrated a discrepancy between physical examination and MRI lesions in JIA. In a recent study conducted by Demir et al. including 57 ERA patients, authors showed that among the patients without axial symptoms (n=30, 53%) had MRI abnormalities (n=23, 77%) (inflammatory or erosive lesions).28 Likewise, Weiss et al. demonstrated that the positive and negative predictive value of low back pain and clinical examination were not good at detection of sacroilitiis.27 Even if most patients were asymptomatic, almost all had structural damage at the sacroiliac joints MRI.27 In a retrospective study including 160 ERA patients, authors noted that only 25% of the patients with sacroiliitis on the MRI were symptomatic.11 In our study, we found that sacroiliac joint pain in the clinical examination predicted sacroiliac bone edema in MRI with an odds ratio of 6.8. This result could be explained by the relatively long diagnosis delay in our patients. Besides, spondyloarthritis seem to be more severe in north African patients.29
Interestingly, we found that sensitivity and specificity of the sacroiliac joints MRI in the diagnosis of ERA were 61.54% and 82.35%, respectively. Positive predictive value was also good. Comparing our result with adults, the sensitivity and specificity were higher than our findings.8 This disagreement was also seen with a previous ERA study in which SI BME has a low sensitivity of 42%, but very high specificity of 96%.30 In fact, while the BME, capsulitis, ankylosis and erosions had also high specificity, the synovial enhancement and the radiologist's global diagnostic impression had the highest sensitivity for ERA diagnosis.30
Nevertheless, the MRI of SI value varied according to the definition used. According to the ASAS criteria, sacroiliac MRI is considered as “positive” if BME is present on at least two sections in the typical subchondral or peri-articular areas.24 Other MRI features presenting active inflammation are not sufficient for a “positive” MRI examination according to the criteria.
ASAS definition was extrapolated in children,31 but it is not yet valid in this population because of the lack of consideration for age-related maturational changes. As shown in the Herregods et al. study, the sensitivity and the specificity were different when the radiologist applied the ASAS definition or the global diagnosis impression.31
Recently, the MRI in JIA working group of Outcome Measures in Rheumatology and Clinical Trials (OMERACT) published the Atlas of MRI in SI joints illustrating the growth-related changes and different features of inflammation and structural damage.23
Certainly this reference will improve the sensitivity and the specificity of this tool to diagnose earlier and with more accuracy features of sacroiliac involvement even in asymptomatic patient.
Recently, Guo et al. highlighted the importance of classifying ERA into two distinctive disease subtypes, axial and peripheral forms, like adult spondyloarthritis. The authors found sacroiliitis in all 57 patients with axial ERA, and 31.58% of patients had asymptomatic inflammation in the sacroiliac joint, as demonstrated on MRI. They suggested that axial ERA was misdiagnosed for a long time due the lack of use of systematic imaging to detect axial inflammation.32
This result raises the question of whether the ILAR 2001 classification criteria,17 which use axial skeleton symptoms (sacroiliac joints pain and low back pain) in the diagnosis of ERA, are able to diagnose all ERA patients? And if the Pediatric Rheumatology International Trials Organization (PRINTO) JIA classification criteria,33 in which sacroilitiis on imaging is a major criterion, are more suitable in these patients?
Even if both of the classification criteria were shown to have great specificity,34,35 sacroiliac joints MRI should be helpful in the early diagnosis of ERA patients especially in litigious cases.
Secondly, we noted that sacroiliac joints MRI lesions were associated with clinical active enthesitis, hip joint limitation, increased CRP level, higher ESR, higher JADAS, and lower BMI. Similarly, Guo et al. showed that JIA patients who had axial involvement, tended to be older, have a longer delay in diagnosis, and exhibit significantly higher levels of inflammatory markers.32
Other studies showed that older age at the onset of ERA, female gender, the number of active joints, number of active enthesitis, HLA-B27 positivity, and increased CRP level were associated with the presence of sacroilitiis in MRI.27,36–38 These findings supported that positive sacroiliitis reflects an active and severe disease and should have an important implication in the therapeutic approach of ERA. Thus, the axial phenotype of ERA may require more aggressive treatments than the peripheral phenotype to prevent progressive damage.32
It is known that conventional synthetic DMARDs were not effective in axial involvement which requires escalating to biological treatment in NSAID refractory children.39
In sum, and despite the small number of patients and a retrospective design of our study, we can conclude that MRI of sacroiliac joints has a high specificity to detect axial involvement and should be considered in all children with peripheral enthesitis or arthritis even if asymptomatic in order to recognize the ERA diagnosis and adapt promptly the therapeutic strategy. However, MRI would be problematic since the interpretation would vary by the level of experience of the MRI reader, and the availability of this expensive tool, especially in the low incomes county. There is another limitation in our study, which is the diagnosis delay of ERA. This could be explained by the fact that this disease is not well known and the patients are late referred.
Another obstacle in MRI use, is the need for sedation in some children and the scan time.
ConclusionOur study showed that sacroiliac joints MRI has a good specificity and positive predictive value in the diagnosis of ERA patients among JIA patients. We also noted an association between MRI lesions and inflammatory biomarkers and disease activity. This underlines the usefulness of sacroiliac joints MRI in the early diagnosis and the follow-up of ERA patients.
Ethical approvalThis study was approved by the ethics committee of the Hospital.
Authors’ contributionsDr. Hanene Ferjani: methodology and writing – review & editing; Dr. Lobna Kharrat: roles/writing – original draft; Dr. Dorra Ben Nessib: data curation and formal analysis; Dr. Dhia Kaffel: data analysis; Dr. Kaouther Maatallah: visualization & conceptualization; Dr. Wafa Hamdi: supervision & validation.
FundingThe authors declare that they have no funding for the research.
Conflict of interestsNone declared.