We present a case of subglottic stenosis (SGS) in a young patient with positive ANCA but a wrong diagnosis of Wegener granulomatosis (WG). Instead, she was diagnosed as having laryngopharyngeal reflux (LPR).
Pitfalls of ANCA testing in this scenario, the route to diagnosis of LPR and the contribution of this entity to subglottic stenosis (SGS) in WG are discussed. Caution when interpreting ANCA results is mandatory to avoid improper management.
Presentamos un caso de estenosis subglótica (ESG) en una paciente joven con ANCA positivos, pero un diagnóstico erróneo de granulomatosis de Wegener (GW). El caso correspondió a reflujo laringofaríngeo (RLF). Se discuten los falsos positivos de la prueba de ANCA, la ruta diagnóstica del RLF y la contribución de esta entidad a la ESG en GW. Debe tenerse precaución en la interpretación de ANCA para evitar el tratamiento inapropiado.
Subglottic stenosis (SGS) in Wegener granulomatosis (WG) occurs in 10%-15% of patients.1 The presence of ANCA in defined clinical settings can be taken as proof to establish the diagnosis. However, misinterpretation when other more common causes of SGS are present can occur. SGS with positive ANCA testing needs exclusion of LPR as cause or contributing factor.
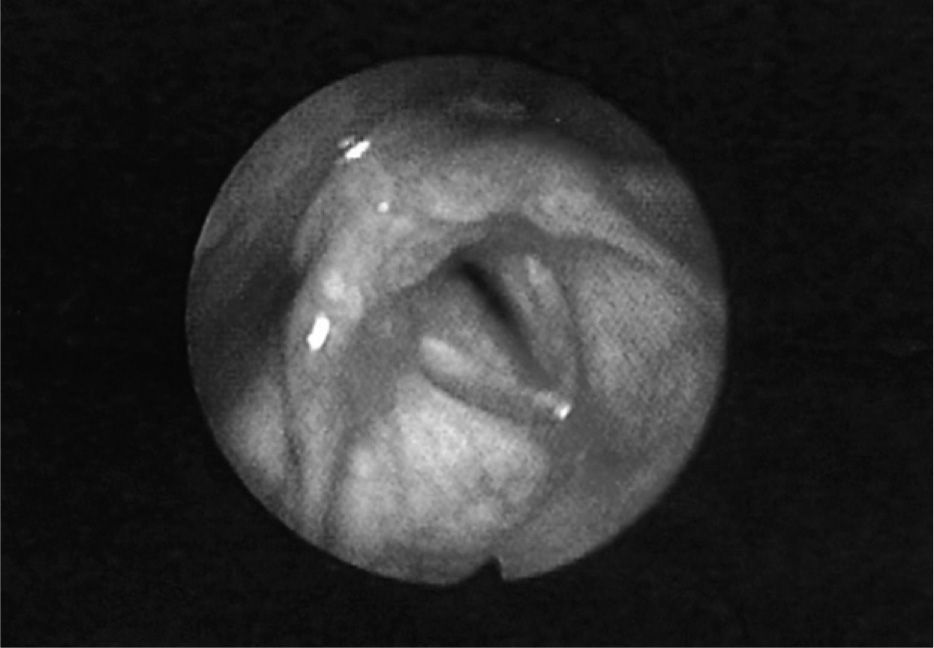
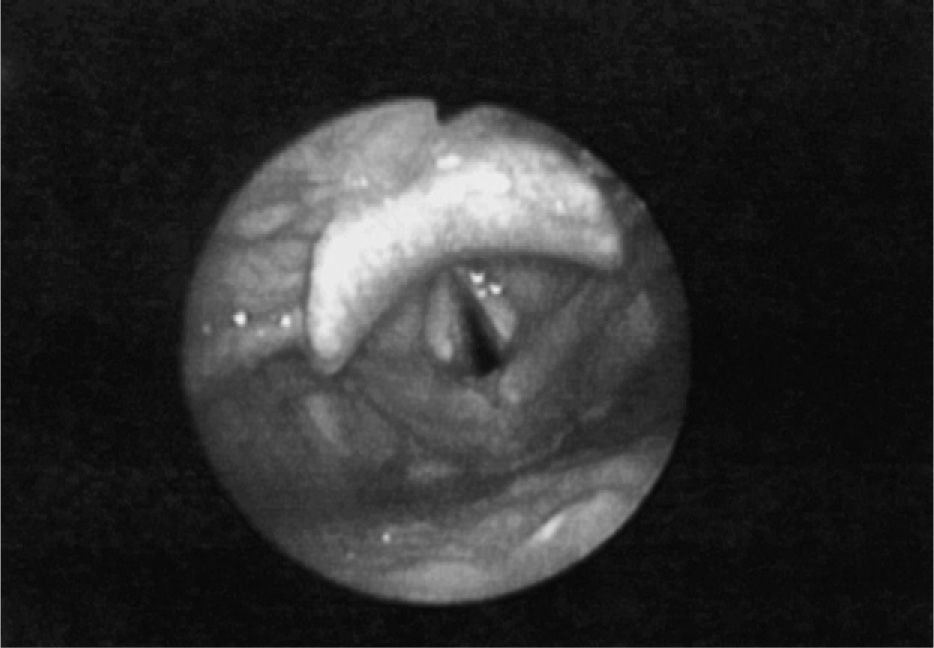
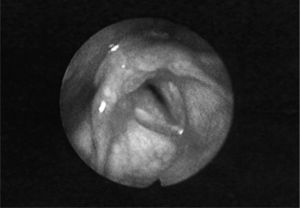
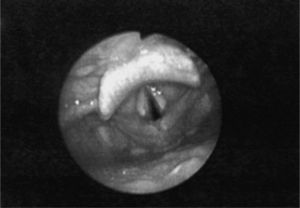
Case reportA 15-year-old woman presented in December 2000 with repetitive upper airway infections and sinusitis. She developed dysphonia, chronic cough, stridor, and frequent dyspnea episodes. ANCA were ordered and positive at a 1:20 dilution by indirect immunofluorescence (IIF) with a cytoplasmic pattern. She was referred to a rheumatologist who started deflazacort (in decreasing doses for one year) and trimethoprim/sulfamethoxazole (TMP-SMZ). Each time steroids were decreased, symptoms returned. In one exacerbation, she had hoarseness and 88% oxygen saturation. Other organ involvement was absent. She was referred to us in January 2003. At that time, all paraclinical studies were normal or negative. A nasofibrolaryngoscopy showed severe inflammatory changes (Figure 1). Evaluation of the distal airway by direct laryngoscopy and flexible bronchoscopy showed no additional pathology. A subglottic tissue biopsy demonstrated nonspecific acute and chronic inflammation with no granulomas or vasculitis. ANCA testing with IIF and ELISA against myeloperoxidase and proteinase-3 was twice negative. An oesophageal manometry showed incompetent lower oesophagic sphincter and 100% relaxation. The 24-hour oesophageal pH confirmed atypical extraoesophageal reflux disease. She had 83 episodes of proximal reflux, 4 of them over 15 minutes, and pH <4.0 for 83 total minutes. The DeMeester score was 23.6 (normal <14.7). During the study she did not record gastrooesophageal symptoms. She was given omeprazole 40mg bid and domperidone 10mg qid. A new nasofibrolaryngoscopy showed improvement (Figure 2). Under treatment for gastrooesophagic reflux disease (GERD) a new study showed absent proximal reflux episodes of >3 minutes, total time of reflux decreasing to 33 minutes. The DeMeester score was 11. She is currently asymptomatic and no new episodes of dyspnea or sinusitis have occurred for more than 6 years.
GERD is a common disease in general population.2 When severe and persistent it can lead to LPR, which in consequence can cause “idiopathic” SGS.3 However, symptoms are not recalled by a subtantial percentage of adult patients.4 To accurately diagnose LPR a modified four-port pH measurement is advised.5 In 1 study, LPR may have contributed to persistent disease in patients with SGS due to WG.3 Our case emphasizes the notion that SGS can have LPR as cause or important collaborative factor.
A panel of experts has recommended that ANCA be performed in cases of unexplained SGS.6 However, although upper airway involvement can be present in 70% as part of the initial manifestations of WG,7 a false positive ANCA result can lead to pitfalls as observed. In a study performed in a general hospital in the UK, McLaren et al8 showed that routine ANCA testing by IIF ordered in different Internal Medicine departments (other than Rheumatology) yielded a low positive predicted value, making them a tool of poor return when not properly indicated. As in many of their cases, the IIF ANCA was a false positive. Their retrieval increased when both IIF and ELISA were performed. Our case clearly underlines the need to perform both methods to detect ANCA (IIF and ELISA) as proposed by the results of the EC/BCR study.9 Also, that in doubtful cases of WG with borderline ANCA testing, histological confirmation of the suspected vasculitides is necessary when the procedure is feasible.
In young or adult patients presenting with a clinical picture compatible with SGS, LPR must be sought even in absence of GERD symptoms. In such cases, a single, isolated positive ANCA test result, especially if done with only one method cannot be taken as proof of WG. This can lead to serious consequences due to the morbidity associated with treatment.10 Moreover, in cases of WG, GERD can still be present and contribute to the symptoms resembling SGS.3 The case provides an important lesson regarding SGS with ANCA positive testing, in where awareness of other causes of SGS is needed. The atypical presentation of the laryngopharyngeal disease, plus the improvement seen with previous steroid and TMP-SMZ treatment during acute dyspnea events further contributed to the impression of WG. Reconsideration of the diagnosis and the mechanism that caused the laryngeal disease led us to term this case as one of WG going backwards.
ANCA testing must be interpreted with caution in patients presenting with SGS as the latter can be due to more common and less severe diseases. As there are individuals who do not recall a history of previous grastrointestinal symptoms this needs special consideration. Practical points about this case are:
- 1.
SGS can occur as complication of asymptomatic LPR.
- 2.
In patients with SGS and positive ANCA, exclusion of LPR as cause or contributing factor is needed.
- 3.
A combined ANCA test using IIF and ELISA is mandatory when an ANCA-associated vasculitides is suspected. Results need to be weighted against the pretest probability of having a true ANCA-associated disease.