We read very attentively the letter by Moreno-Martinez et al.,1 who describe a case of pelvic osteoid osteoma (OO), in which the clinical signs and symptoms were compatible with sacroiliitis. We would like to report another OO that developed in knee, that suggested a diagnosis of juvenile psoriatic arthritis (JPA).
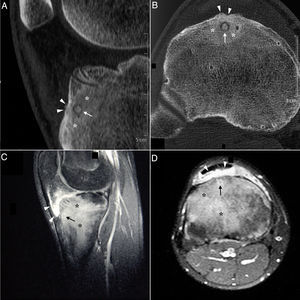
A 15-year-old boy presented with an 8-month history of mechanical pain in right knee. It would be intermittent at first and later become continuous, making it difficult for him to walk, and swelling was observed in that area. The treatment consisted of nonsteroidal anti-inflammatory drugs (NSAID), initially ibuprofen, which was replaced by diclofenac, but there was no improvement. He had no history of injury, fever or constitutional symptoms, or manifestations affecting any other peripheral or axial joint or enthesitis. He had been diagnosed with guttate psoriasis at the age of 10 years, with occasional episodes until he was 13, and was treated with topical glucocorticoids; however, he had no family history of psoriasis, psoriatic arthritis, ankylosing spondylitis or inflammatory bowel disease. Physical examination revealed muscle atrophy in distal thigh and swelling in right infrapatellar region, which was warm, and he had a limitation in last few degrees of flexion, but with no signs of joint effusion. The results of laboratory tests, including biochemical analyses, complete blood count and acute-phase reactants (erythrocyte sedimentation rate 6mm/h, C-reactive protein 2.31mg/dL) were normal. Human leukocyte antigen (HLA) typing revealed the presence of Cw6, DR4 and DQ8 haplotypes, but not B27, and the patient was negative for rheumatoid factor and antinuclear antibodies. Plain radiography of the knees showed a sclerotic area in the upper third of right tibia (Fig. 1A and B), which, according to computed tomography (CT), corresponded to an osteolytic lesion measuring 5mm in diameter in anterior tibial tuberosity, with a “nidus” formed by an ossified matrix, compatible with OO (Fig. 2B and C), with extensive sclerosis of the medullary bone and a solid periosteal reaction in the adjacent cortical bone. Magnetic resonance revealed intense contrast uptake in and around the lesion, as well as in the surrounding bone edema and the Hoffa fat pad (Fig. 2C and D). Bone scintigraphy disclosed hyperemia and a focal increase in the osteogenic response in the proximal epiphysis of right tibia, with no other significant changes. The patient underwent CT-guided radiofrequency ablation, and the pain disappeared a few days after the procedure, and he recovered complete mobility 1 month later, although he had mild persistent muscle atrophy.
Sagittal (A) and axial (B) computed tomography images of right knee showing an osteolytic lesion in the subendosteal region of the anterior tibial tuberosity, with a “nidus” formed by ossified matrix, compatible with osteoid osteoma (arrow), encircled by extensive sclerosis of the surrounding medullary bone (asterisks) and a solid periosteal reaction in the adjacent cortical bone (arrowheads). Post-gadolinium sagittal (C) and axial (D) T1-weighted spectral presaturation with inversion recovery (STIR) magnetic resonance images revealed perilesional contrast uptake in the form of a ring (arrow), and in surrounding bone edema (asterisks) and Hoffa fat pad (arrowheads).
Osteoid osteoma is a relatively common, benign bone neoplasm that constitutes between 10% and 12% of benign bone tumors. It usually develops between the ages of 10 and 20 years (although it has been reported in smaller children), and the ratio of males-to-females is 2–3:1.2,3 It most often affects the lower limbs, and is located in the femur and tibia in 50% to 60% of the cases, with a predilection for cortical bone, involving the diaphysis, the metaphysis or, rarely, the epiphysis.4 Nocturnal pain is predominant, and if it is not related to physical activity, becomes more severe during rest and is relieved by salicylates or NSAID, it is highly suggestive of OO2–4; however, when its location is juxta- or intra-articular, its presentation may be atypical and mimic other disorders, like oligoarticular juvenile idiopathic arthritis (JIA), and can be accompanied by limping, muscle atrophy, synovitis, contractures and dysmetria of the lower limbs.2,3,5–8 This leads to a delay in the diagnosis, que is usually more than 6 months and ranges between 13.8 and 28 months.9 In our patient, the diagnosis that was initially proposed was JPA, a category of the classification of the International League of Associations for Rheumatology (ILAR) for JIA, defined as arthritis in a patient under 16 years of age, with a duration of at least 6 weeks, associated with psoriasis or with 2 of the following characteristics: dactylitis, nail pitting, onycholysis or psoriasis in a first-degree relative.10 However, the swelling observed actually corresponded to inflammatory changes in the adjacent infrapatellar fat pad (“Hoffitis”), rather than being a sign of synovitis. As the radiographic findings may also be atypical or the “nidus” not be clearly evident, CT is the best technique for detecting it in these cases.7–9 Thus, OO should be taken into account in the differential diagnosis of a long history of pain in a single joint, especially in children and adolescents with knee pain or monoarthritis with atypical features and/or a poor response to treatment.5,7,9
Please cite this article as: Boteanu AL, Sifuentes-Giraldo WA, Antón-Pagés F, Gámir-Gámir ML. Osteoma osteoide de rodilla simulando artritis psoriásica juvenil. Reumatol Clín. 2017;13:240–242.