Patients with rheumatoid arthritis (RA) complain that weather conditions aggravate their symptoms. We investigated the short-term effects of weather conditions on worsening of RA and determined possible seasonal fluctuations.
MethodsWe conducted a case-crossover study in Madrid, Spain. Daily cases of RA flares were collected from the emergency room of a tertiary level hospital between 2004 and 2007.
Results245 RA patients who visited the emergency room 306 times due to RA related complaints as the main diagnostic reason were included in the study. Patients from 50 to 65 years old were 16% more likely to present a flare with lower mean temperatures.
ConclusionsOur results support the belief that weather influences rheumatic pain in middle aged patients.
Los pacientes con artritis reumatoide (AR) se quejan de que las condiciones meteorológicas empeoran sus síntomas. Este estudio trata de ver los efectos a corto plazo de las condiciones climáticas en empeoramiento sintomático en pacientes con AR y determinar posibles fluctuaciones estacionales.
MétodosSe realizó un estudio de casos cruzados en Madrid, España. Los casos diarios de empeoramiento de la AR se obtuvieron de la sala de urgencias de un hospital terciario entre 2004 y 2007.
Resultados245 pacientes con AR con 306 visitas a urgencias con AR como diagnostico principal se incluyeron en el estudio. Los pacientes de 50 a 65 años tuvieron un 16% más de probabilidades de presentar empeoramiento sintomático de la AR con una menor temperatura media.
ConclusionesNuestros resultados apoyan la creencia de que el clima influye en el dolor reumático de los pacientes con mediana edad.
Patients with rheumatic conditions often complain that certain meteorological conditions aggravate their disease symptoms.1–3 However, studies on influence of weather conditions1,3–8 have reported conflicting results, most related to rheumatoid arthritis patients (RA). Some studies indicated that weather conditions do not influence the symptoms of arthritis,2,3 whereas others found an influence related to low temperature, high atmospheric pressure, and high humidity.1,4,9 Moreover, some authors found a seasonal effect6,7 but others did not.5,8 Thus, scientific evidence on the effects of atmospheric factors on rheumatic diseases is sparse and non-conclusive. Discrepancies could be related to the diverse climatic conditions from each geographic area studied and also due to the different methodologies used.
To our knowledge no study has previously been conducted in our setting for these rheumatic disorders. Our objective is to investigate the short-term effects of weather conditions on the acute worsening in rheumatic patients due to RA related conditions and also to determine possible seasonal fluctuations.
MethodsThis study was conducted in the city of Madrid, Spain, with a Mediterranean continental climate very influenced by urban conditions. Winters are cold, with mean temperatures below 10°C with frequent frosts at night and occasional snowfalls. Summers are warm with mean temperatures over 20°C.
Daily cases of RA worsening, were defined as those patients who come to the emergency room, were attended by a rheumatologist of Hospital Clínico San Carlos, and were diagnosed with RA as the main cause reflected in the ICD code (10th revision), from 1st January 2004 until 31st December 2007. The Hospital Clínico San Carlos is a tertiary hospital, covering a population over 500,000 inhabitants. For all cases we also collected age, gender, and disability index.10
The study was approved by the HCSC Ethics Committee.
As weather conditions we measured: Daily mean, maximum and minimum temperatures (in °C), relative humidity (%), pressure (hPA), rain (mm), hours of sun, and cloud cover (octas) were obtained from the European Climate Assessment & Dataset (ECA&D).11
The association of weather conditions with daily RA worsening was investigated using a case-crossover design,12 which uses the day on which the RA aggravation occurs as a case day. Exposure on case days is compared with exposure on days on which the RA worsening does not occur (control days). A time-stratified approach was selecting control days from the same day of the week, month, and year as case days. This minimise bias from time-trends and other time-varying confounders.13 Short-term effects of weather variables on daily cases, from the same day up to one-week lag, were estimated using conditional logistic regression.
ResultsA total of 245 patients with 306 RA visits to the emergency room due to RA as the main diagnostic reason during the study period were included. Most were women (71%), with a mean age of 63.6±16.4 years. Two thirds were attended at least twice in the emergency room due to RA worsening, with some level of disability (90% with a Rosser index less than 0.990). During the study period weather conditions were on average: 14.6°C of temperature (ranging from −5 to 39), 54% of relative humidity (15–96), 1.018hPA of pressure (904–1408), 111mm of rain (0–420), 8.3h of sun (1–14), and 3.2 octas of cloud cover (0–8).
Statistical significant (p<0.05) association with RA worsening was only found for daily mean temperature, with a lagged effect of 1 day, in middle age patients from 50 to 65 years old (Table 1). These were 16% more likely to present symptomatic deterioration of RA, with lower mean temperature (OR=0.86, 95% CI=[0.78–0.96] for an increase of 1°C). Both, men and women, showed similar risk estimates with mean temperature. No other weather conditions were statistically associated with the need of RA patients to bee attended in the emergency room due to RA related conditions.
Odds ratio (OR), and 95% confidence interval (95% CI), of daily RA worsening for an increase of 1°C of daily mean temperature (for a 1-day lag), by age group.
| n* | (%) | OR | 95% CI | p | |
| Age group | |||||
| <50 years | 60 | (20.0) | 0.999 | (0.909–1.098) | 0.986 |
| 50–65 years | 73 | (23.5) | 0.868 | (0.783–0.962) | 0.007 |
| >65 years | 173 | (56.5) | 1.035 | (0.979–1.095) | 0.223 |
| Total | 306 | (100) | 0.993 | (0.952–1.037) | 0.776 |
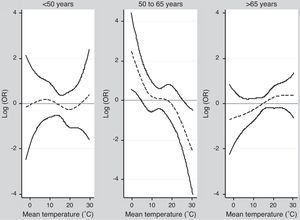
To evaluate seasonal variations mean temperature was fitted in the conditional logistic regression model using a cubic spline, with 3 degrees of freedom (Fig. 1). Significant effects were only found in the most extreme ranges of mean temperature for middle age people, being 15% and 20% more likely of RA worsening with mean temperatures below 10°C (OR=0.83, 95% CI=[0.69–0.99]) and above 20°C (OR=0.82, 95% CI=[0.66–0.99]).
DiscussionThere is a popular belief that rheumatic conditions are particularly sensitive to fluctuations of weather. We have found associations with meteorological conditions (specifically with temperature), and RA related problems in the subgroup of middle age patients.
The failure to find associations with other age groups could be explained because age itself is a risk factor for disability, thus elderly could have in general more difficulty to go to the emergency room by themselves. Moreover, rheumatic pain is frequently considered to be a natural part of the aging process. Otherwise, the younger may have problems to miss work using other ways rather than emergency room to control their RA symptoms.
Previous studies in similar settings have also found that mean temperature is related with rheumatic disorders.1,4,9 Nevertheless, we did not find associations with other weather variables, as atmospheric pressure or relative humidity, probably due to Madrid has a Mediterranean continental climate much dryer and less humid than other cities studied.1,4,9
We found that the strongest effects of daily mean temperature on RA worsening were found below 10°C and above 20°C, meanwhile no statistical association was observed between 10 and 20°C. This could reflect the possible seasonal distribution of RA symptomatic deterioration with higher incidence in winter and summer. Additionally, between 10 and 20°C the thermal sensation and small changes probably are better tolerated than in the others, where we subjectively feel cooler or warmer.
It is important to note that in our setting, RA patients receive long-term monitoring, with self-education in the management of pain and small flares. They are encourage to contact us when they have some kind of medical problem, either by telephone or by medical appointments in 24–48h. When they have the need to go to the emergency room is often a due to a disabling pain or significant inflammatory activity. With the data available we cannot specify the main cause of RA symptomatic deterioration.
The main contribution of our study is the methodological approach using a case-crossover design, a common study design to assess for short-term effects of environmental factors on health.13,14 Moreover, our RA patients were well represented, 70% women in their sixties.15
The explanation of the influence of temperature on rheumatic diseases is not clear enough. It is known that cold unleash some diseases such as Raynaud phenomenon or crioglobulinemia, both closely related to rheumatic diseases. Maybe muscles also play a role in relation to flares or pain in RA patients and cold weather, due to coldness stiffens muscles around the joints, and this might worsen the arthritis symptoms.
In conclusion, our results support that weather conditions, essentially daily mean temperature, may be influencing in RA patients.
Ethical considerationsProtection of human and animal subjects. The authors declare that the procedures followed were in accordance with the regulations of the responsible Clinical Research Ethics Committee and in accordance with those of the World Medical Association and the Helsinki Declaration.Confidentiality of data. The authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.Right to privacy and informed consent. The authors declare that no patient data appears in this article.
Conflict of interestAuthors declare that they have no conflict of interest.