To analyse current status, control and impact of RA on patients’ lives as well as the management of RA symptoms.
MethodsA structured anonymous online questionnaire was designed and sent to patients with RA, aged 18 years or above living in Spain. Participants were invited though different strategies: 1) ConArtritis and related patients associations; 2) Patients participating in the platform www.in-pacient.es; 3) Links from ConArtritis website and open social networks. Sociodemographic and clinical variables, as well as others related to the objectives were collected. A descriptive analysis was performed.
ResultsWe analysed 882 RA patients, 89% women, with a median age of 52 years, 31.9% disease duration <5 years. They reported a mean pain and patient global disease score (0−10) of 5.1 and 4.9 respectively. The rate of patients with many difficulties or inability to perform daily tasks varied from 6.4% to 49.2%. Based on the activity index 56.8% of patients reported high activity. We found a great or severe impact on the emotional well-being in 31.5% of patients, and of 29.2% in the workplace or academic setting. A total of 87.9% are taking some medication for RA, and 17.3% are little/not satisfied with them. In addition, 67.1% take conventional synthetic disease modifying drugs (DMARDs), and 45.9% biological therapies including biosimilars and small molecules.
ConclusionsThe current impact of RA on patients’ daily lives remains very high. A significant number of patients are not taking DMARDs (conventional synthetic and/or biologics) despite high activity.
Analizar el estado, control, impacto y manejo actual de la artritis reumatoide (AR) según los pacientes.
MétodosEncuesta para la que se envió un cuestionario estructurado, anónimo, en formato electrónico a pacientes adultos con AR residentes en España, a través de 1) ConArtritis o sus asociaciones; 2) Pacientes de la plataforma www.in-pacient.es; 3) Vínculos desde la página web de ConArtritis y redes sociales abiertas. Se recogieron variables sociodemográficas y clínicas, y otras relacionadas con los objetivos propuestos. Se realizó un análisis descriptivo.
ResultadosAnalizamos 882 pacientes, 89% mujeres, con una edad mediana de 52 años, 31,9% AR < 5 años de evolución. El dolor y la valoración global de la enfermedad actuales medios (0-10) fueron de 5,1 y 4,9 respectivamente. El porcentaje de pacientes con muchas dificultades o imposibilidad para realizar tareas cotidianas varió del 6,4% al 49,2%. En base al índice de actividad el 56,8% de los pacientes presenta alta actividad. Los pacientes refieren mucho impacto o impacto grave del 31,5% a nivel emocional, o del 29,2% en el ámbito laboral o académico. El 87,9% sigue algún tratamiento para la AR, y el 17,3% está poco/nada satisfecho con el mismo. El 67,1% toma fármacos modificadores de la enfermedad (FAME) sintéticos convencionales, y el 45,9% terapias biológicas incluyendo biosimilares y pequeñas moléculas.
ConclusionesEl impacto actual de la AR en la vida del paciente sigue siendo muy alto. Un porcentaje significativo de pacientes no sigue un tratamiento con FAME (sintéticos convencionales y/o biológicos) a pesar de su actividad.
Rheumatoid arthritis (RA) is a chronic inflammatory disease with a prevalence in Spain of approximately 1%.1,2 It has great impact on patients, society and the social and healthcare systems.3
In recent years a change has occurred in the management paradigm of this disease which has led to positive changes in patient prognosis. The appearance of innovative therapies, early diagnosis and an aggressive, systematic and comprehensive approach has achieved optimisation of many parameters related to RA, including mortality, disability and quality of life.4–7
Despite these great advances, there are still many uncovered or unresolved issues which require further investigation. Among them is fatigue, pain, sleep and everything relating to the psychological/emotional area.8–11 For example, it has been reported that up to 38.8% of patients with RA may present with severe fatigue12 and for 61% sleep quality is bad,13 and it has been published that restrictions in social participation are associated with changes in the psychological status of these patients.
Furthermore, this change of paradigm in RA has also involved another series of changes, which include greater leading role of the patient in decision-making.5 Many guidelines therefore recommend taking informed and shared decisions between physicians and patients.5 It is important to bear in mind the patients’ viewpoint regarding their experience, priorities, objectives and expectations of the disease, which is often different from that of their doctor.14 For example, for many patients, their everyday well-being depends on different elements, depending on the moment. For many, during the day, pain, fatigue, depression or facing up to the disease are all highly relevant. At night, however, pain, problems with sleep or sexual dissatisfaction are the most important issues. However, the medical focus centres more on objective events which are specifically assessed on the day of consultation. We also need to consider how the disease impacts other areas of the patients’ lives and their opinion on everything surrounding RA. A survey conducted with almost 4000 patients from various European countries15 has shown that 47% of them stopped carrying out certain activities and almost 30% of them stopped working or changed jobs due to their RA. Regarding treatments, over 50% of patients would like to be able to choose between more drugs and 15% were concerned about all treatment options being exhausted.15
Despite the relevance of having data relating to patient experience and opinion regarding their disease and treatments, the information available in Spain is currently very scarce. As a result, the National Arthritis Coordinator, the ConArthritis patient association, suggested carrying out a survey to collect RA patients’ opinion on the status, impact and current management of their disease. The intention was for any collected information to help healthcare professionals take decisions and to guide future projects of the association.
MethodsThis project was promoted by ConArthritis. A survey was conducted aimed at patients with RA, in full compliance with the principles established in the Declaration of Helsinki, referring to medical research in human beings, in its latest version, and in keeping with the regulations applicable on good clinical practice. The project was approved by the CEIC of the Hospital of Elda in Alicante.
Design, survey launch and data acquisition (see Appendix B additional material). Firstly, a multidisciplinary group of rheumatologists, patients and methodologists analysed the current state of RA management and selected the critical points of the same to be assessed in the survey. With this information, a closed and structured questionnaire was designed (lasting 18 min), in electronic format, to be responded to by patients with RA, who were over 18 years of age and resident in Spain. It was available from 7th October 2019 until 9th December 2019. The following recruitment sources were used: 1) members associated with ConArthritis or their associations with an invitation by electronic mail or publication on social mean (Facebook, Instagram, LinkedIn, Tweeter); 2) patient participants on the platform www.in-pacient.es through direct invitation within the platform and 3) links from the web site of ConArthritis and open social networks. Prior to sending, a group of 5 patients with RA from ConArthritis, using a small pilot study, assessed the questionnaire and generated the final questionnaire with their suggestions.
Variables. The following variables were collected: 1) Membership or non-membership to a patient association; 2) sociodemographics (age, sex); 3) clinical and disease-related variables: including age at diagnosis of RA; duration of RA; treatments including analgesics, anti-inflammatories, glucocorticoids and synthetic and biologic disease-modifying anti-rheumatic drugs (DMARDS), including biosimilars and JAKs inhibitors; the presence of comorbidity in treatment; pain (scale of 0 [none] to 10 [maximum pain]); overall patient evaluation of the disease (OPA, scale 0 very good-10 very bad); perception of disease control (totally, good, somewhat controlled, not controlled or badly controlled); current impact of RA (none, a bit, quite a lot, a lot, severe impact) on an emotional, cognitive, academic, social, family and other levels; the need for help with daily activities (yes/no); concern for the future scale 0 (not concerned at all)-10 (extremely concerned); degree of impact of symptoms (joint inflammation, morning stiffness, pain, fatigue) on the patient’s life 1 (great impact)-10 (no impact); symptoms in the last month (joint inflammation, morning stiffness, pain, fatigue); impact of symptoms in the last month 0 (none) to 10 (the highest impact); control of symptoms in the last month scale of 0 (very well managed) to 10 (very badly or not managed at all); strategies for managing symptoms; 4) variables on the doctor-patient relationship (understanding scale 1 nil-5 very high, asking about your everyday limitations, coinciding with the objectives suggested by the doctor, consensual to the treatment decisions), and 6) taken from RAPID3 except for questions on opening taps, walking 3 km and taking part in games and sports, which were replaced with going up and down stairs, carrying out occupational tasks and driving. Questions asked were modified to adapt to current life conditions, as they were regularly carried out.
An RA activity index based on the sum of the average score of the RAPID3, pain and OPA (scale 0–30) was made. The result was classified into: remission (0–3), low activity (4–6), moderate activity (7–12), high activity (13–30). It was decided that RAPID3 should be used for good correlation with objective variables like DAS28.
Statistical analysis. Data analysis was performed using the statistical programme Stata 12© (Stata Corporation, College Station, TX, U.S.A.). A descriptive analysis of data was made, together with bivariate analysis. For comparisons, the Student’s t test and Mann–Whitney U test was used for continuous variables and the Chi squared test for categorical variables. Quantitative variables were described using means ± standard deviation and qualitative variables with frequencies and percentages. The overall sample was analysed and the analysis of subgroups in RA of high activity in keeping with the activity index and in RA of recent onset (≤2 years of evolution).
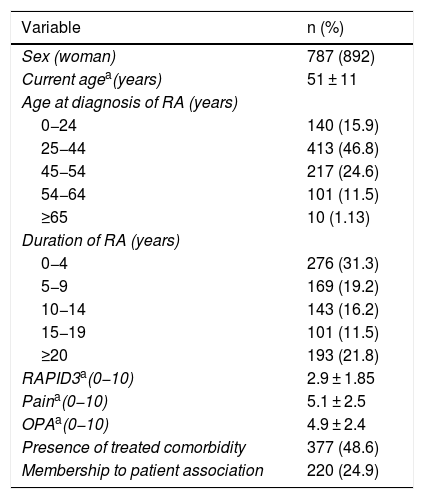
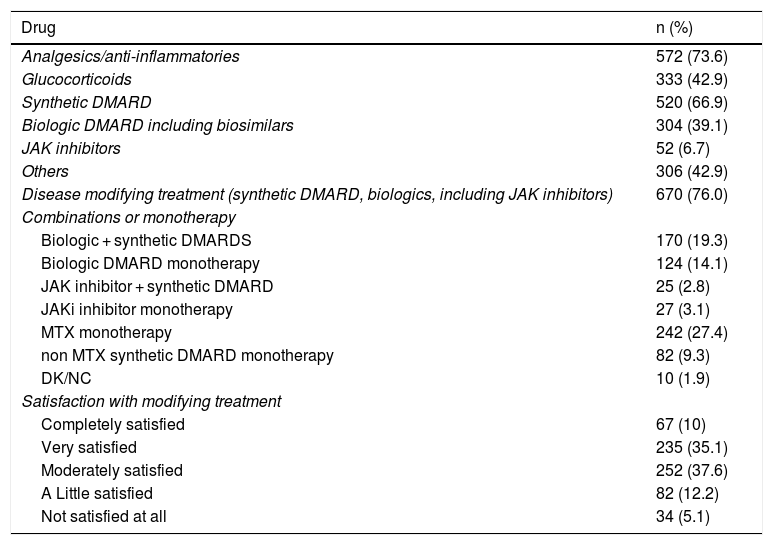
ResultsGlobal sampleWe analysed 882 patients, 89.2% women, with a mean age of 51 ± 11 years and a mean age at diagnosis of RA of 38 ± 14 years. 31.9% presented with RA of at least 5 years evolution and 75.1% of the same did not belong to a patient association (Table 1). With regard to 24.9% (n = 220) of RA patients belonging to a patient association, they presented with a mean age of 50 years, a mean age at diagnosis of 34 years and RAPID3 scores on pain, fatigue and OPA of 3.1 ± 1.8, 4.9 ± 2.6, 5.5 ± 2.7 and 4.8 ± 2.5, respectively. Regarding treatments, 73.6% of the respondents took analgesics/anti-inflammatories, 42.9% glucocorticoids, 66.9% synthetic conventional SMARDS and 39.1% biologic DMARDS including biosimilars (Table 2). Forty five per cent stated they were completely or very satisfied with the treatment with DMARDS (conventional synthetic and biologics). By pharmacological groups, the percentage of patients who were completely or highly satisfied with them varied from 40.9% with analgesics or anti-inflammatory to 32% with glucocorticoids, 42.6% with the synthetic conventional DMARDS and 50.5% with biologic DMARDS including biosimilars. However, 41.8% would prefer to stop taking methotrexate immediately.
Baseline characteristics of patients included in the AR 2020 survey.
| Variable | n (%) |
|---|---|
| Sex (woman) | 787 (892) |
| Current agea(years) | 51 ± 11 |
| Age at diagnosis of RA (years) | |
| 0−24 | 140 (15.9) |
| 25−44 | 413 (46.8) |
| 45−54 | 217 (24.6) |
| 54−64 | 101 (11.5) |
| ≥65 | 10 (1.13) |
| Duration of RA (years) | |
| 0−4 | 276 (31.3) |
| 5−9 | 169 (19.2) |
| 10−14 | 143 (16.2) |
| 15−19 | 101 (11.5) |
| ≥20 | 193 (21.8) |
| RAPID3a(0−10) | 2.9 ± 1.85 |
| Paina(0−10) | 5.1 ± 2.5 |
| OPAa(0−10) | 4.9 ± 2.4 |
| Presence of treated comorbidity | 377 (48.6) |
| Membership to patient association | 220 (24.9) |
OPA: overall patient assessment of the disease; RA: rheumatoid arthritis.
Results are expressed as numbers and percentages (%) unless otherwise indicated.
Current treatments administered to patients in AR 2020 survey.
| Drug | n (%) |
|---|---|
| Analgesics/anti-inflammatories | 572 (73.6) |
| Glucocorticoids | 333 (42.9) |
| Synthetic DMARD | 520 (66.9) |
| Biologic DMARD including biosimilars | 304 (39.1) |
| JAK inhibitors | 52 (6.7) |
| Others | 306 (42.9) |
| Disease modifying treatment (synthetic DMARD, biologics, including JAK inhibitors) | 670 (76.0) |
| Combinations or monotherapy | |
| Biologic + synthetic DMARDS | 170 (19.3) |
| Biologic DMARD monotherapy | 124 (14.1) |
| JAK inhibitor + synthetic DMARD | 25 (2.8) |
| JAKi inhibitor monotherapy | 27 (3.1) |
| MTX monotherapy | 242 (27.4) |
| non MTX synthetic DMARD monotherapy | 82 (9.3) |
| DK/NC | 10 (1.9) |
| Satisfaction with modifying treatment | |
| Completely satisfied | 67 (10) |
| Very satisfied | 235 (35.1) |
| Moderately satisfied | 252 (37.6) |
| A Little satisfied | 82 (12.2) |
| Not satisfied at all | 34 (5.1) |
DMARD: disease-modifying anti-rheumatic drug; DK/NC: don’t know, no comment; JAK: janus kinase; JAki: janus kinase inhibitors; MTX: methotrexate; RA: rheumatoid arthritis.
Results are expressed as numbers and percentages (%) unless otherwise indicated.
The pain and OPA means reported were 5.1 and 4.9, respectively. Based on the activity index, 8.3% of patients were in remission, 6.5% with low activity, 28.5% with moderate activity and 56.8% with high activity. However, according to the perception of patients, for 12.5% of them their RA was totally controlled, for 43, 5% well controlled, for 29.6% somewhat controlled and for 14.4% not controlled or only a little controlled.
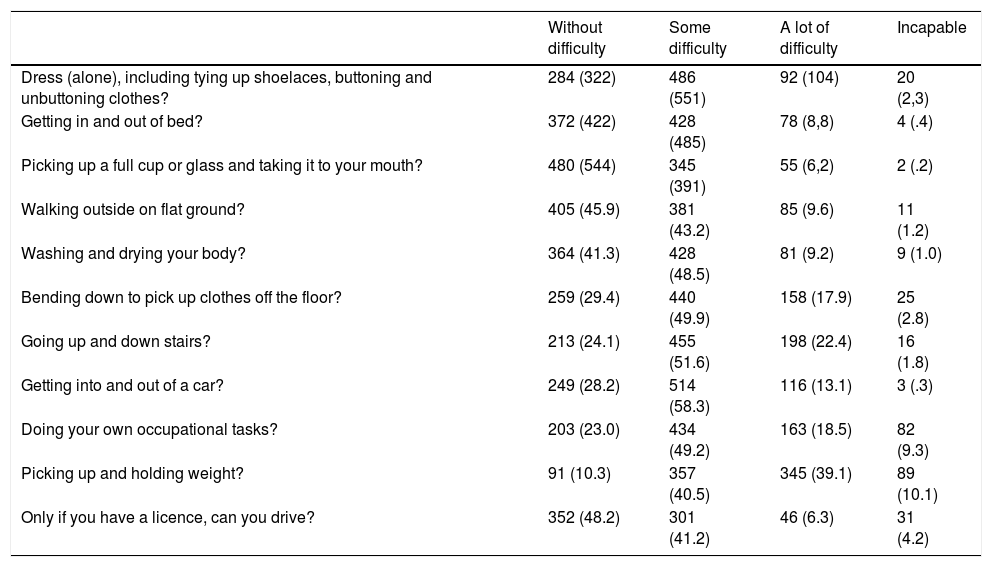
In the overall sample, on analysing through items of the RAPID 3 (Table 3), we highlighted that for 49.2% of patients picking up weights was impossible to do or they had great difficulty doing it. The same occurred for going up and down stairs for 44.2%.
Result from the variables included in RAPID3.
| Without difficulty | Some difficulty | A lot of difficulty | Incapable | |
|---|---|---|---|---|
| Dress (alone), including tying up shoelaces, buttoning and unbuttoning clothes? | 284 (322) | 486 (551) | 92 (104) | 20 (2,3) |
| Getting in and out of bed? | 372 (422) | 428 (485) | 78 (8,8) | 4 (.4) |
| Picking up a full cup or glass and taking it to your mouth? | 480 (544) | 345 (391) | 55 (6,2) | 2 (.2) |
| Walking outside on flat ground? | 405 (45.9) | 381 (43.2) | 85 (9.6) | 11 (1.2) |
| Washing and drying your body? | 364 (41.3) | 428 (48.5) | 81 (9.2) | 9 (1.0) |
| Bending down to pick up clothes off the floor? | 259 (29.4) | 440 (49.9) | 158 (17.9) | 25 (2.8) |
| Going up and down stairs? | 213 (24.1) | 455 (51.6) | 198 (22.4) | 16 (1.8) |
| Getting into and out of a car? | 249 (28.2) | 514 (58.3) | 116 (13.1) | 3 (.3) |
| Doing your own occupational tasks? | 203 (23.0) | 434 (49.2) | 163 (18.5) | 82 (9.3) |
| Picking up and holding weight? | 91 (10.3) | 357 (40.5) | 345 (39.1) | 89 (10.1) |
| Only if you have a licence, can you drive? | 352 (48.2) | 301 (41.2) | 46 (6.3) | 31 (4.2) |
Results are expressed as numbers and percentages (%) unless otherwise indicated.
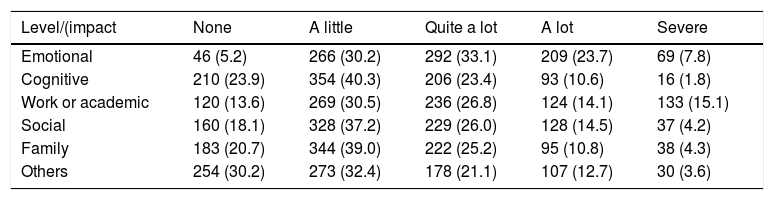
Equally, 31.5% of patients stated their RA had a great or severe impact on their emotional state, 124% on their cognitive state, 29.2% on their employment or academic environment, 187% on their social life and 15.1% on their family environment (Table 4). Also, 42.2% referred to the need for help from another person to carry out daily activities.
Impact of RA on difference aspects of the patient’s life.
| Level/(impact | None | A little | Quite a lot | A lot | Severe |
|---|---|---|---|---|---|
| Emotional | 46 (5.2) | 266 (30.2) | 292 (33.1) | 209 (23.7) | 69 (7.8) |
| Cognitive | 210 (23.9) | 354 (40.3) | 206 (23.4) | 93 (10.6) | 16 (1.8) |
| Work or academic | 120 (13.6) | 269 (30.5) | 236 (26.8) | 124 (14.1) | 133 (15.1) |
| Social | 160 (18.1) | 328 (37.2) | 229 (26.0) | 128 (14.5) | 37 (4.2) |
| Family | 183 (20.7) | 344 (39.0) | 222 (25.2) | 95 (10.8) | 38 (4.3) |
| Others | 254 (30.2) | 273 (32.4) | 178 (21.1) | 107 (12.7) | 30 (3.6) |
RA: rheumatoid arthritis.
Results are expressed as numbers and percentages (%) unless otherwise indicated.
However, we found that 56% of respondents had concerns for the future which were higher than 8 (scale 0−10). The mean age of these patients we 49 ± 11 years and their RA had a mean duration of 12 ± 11 years.
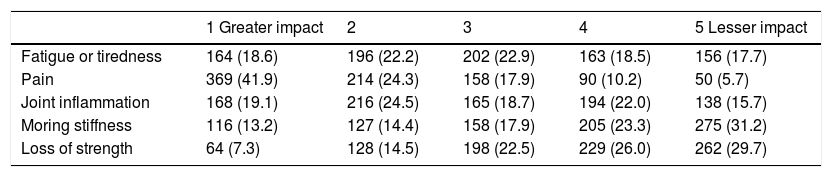
For 41.9% of patients, pain was the most impacting symptom in their life (score 1 on the scale), followed by fatigue and inflammation (19.1% and 18.6% of score 1, respectively (Table 5).
Degree of impact in everyday of the following RA symptoms.
| 1 Greater impact | 2 | 3 | 4 | 5 Lesser impact | |
|---|---|---|---|---|---|
| Fatigue or tiredness | 164 (18.6) | 196 (22.2) | 202 (22.9) | 163 (18.5) | 156 (17.7) |
| Pain | 369 (41.9) | 214 (24.3) | 158 (17.9) | 90 (10.2) | 50 (5.7) |
| Joint inflammation | 168 (19.1) | 216 (24.5) | 165 (18.7) | 194 (22.0) | 138 (15.7) |
| Moring stiffness | 116 (13.2) | 127 (14.4) | 158 (17.9) | 205 (23.3) | 275 (31.2) |
| Loss of strength | 64 (7.3) | 128 (14.5) | 198 (22.5) | 229 (26.0) | 262 (29.7) |
RA: rheumatoid arthritis.
Results are expressed as numbers and percentages (%) unless otherwise indicated.
On being asked about their situation in the last month, 74.4% described the presence of joint inflammation and 67% of morning stiffness. The impact of symptoms during this time varied (scale 0−10) from 5.5 ± 2.3 for fatigue to 5.1 ± 2.6 for pain, 5.7 ± 2.1 for inflammation and 5.4 ± 2.4 for morning stiffness.
However, regarding management of symptoms in general, a mean score was obtained (scale de 0−10) of 4.3–5.3, depending on the symptom. The most commonly used control strategies were taking medication and ceasing to do certain activities.
Finally, regarding the doctor-patient relationship, 60% stated there was a good/very good understanding, 63.4% that their doctors asked them about their daily limitations. For 73% their objectives coincided with those of their doctors and 69% agreed with the treatment decisions. They also underlined that only 100 patients (12.5%) were aware of all the alternative treatments for RA.
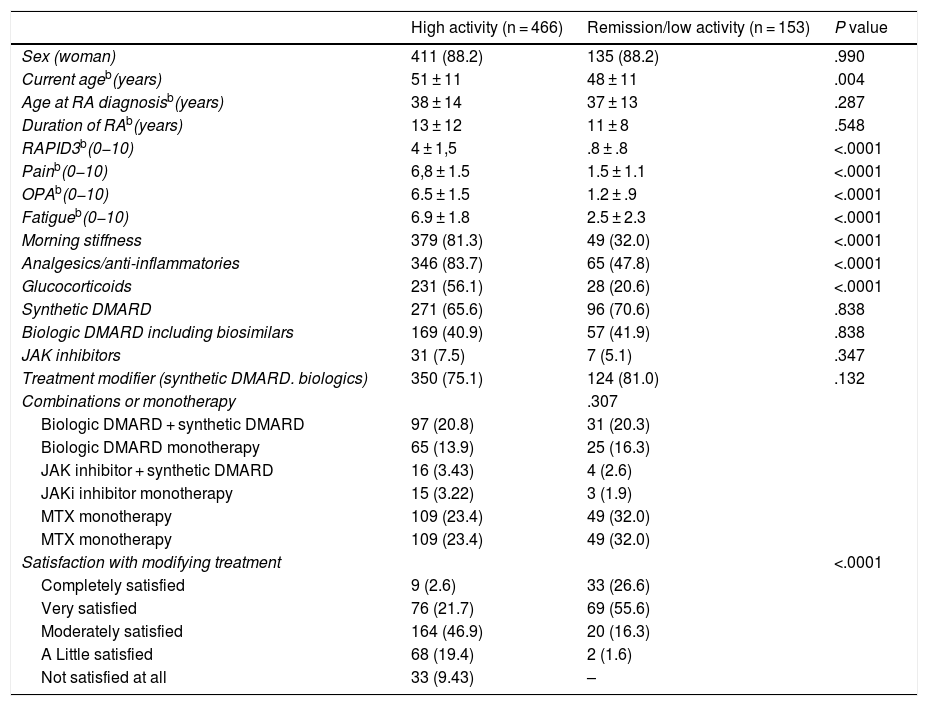
Patient subgroupsTable 6 describes and compares the main characteristics presented, based on the activity index, the RA with high activity and the RA with low activity or remission. With regard to those with high activity, most of these patients were women with a RA of long evolution, where (as we expected) pain levels (mean 6.8 ± 1.5) and fatigue levels (mean 6.9 ± 1.8) were high. Regarding the impact of symptoms, 42.9% referred to great or severe emotional level impact, 20.2% to cognitive level, 46.1% to the employment or academic environment, 30% to social level and 22.7% to family level. However, we would highlight that almost 25% of them said they would not follow a treatment with DMARDS (synthetic or biological). In relation to treatments, 83.7% of these patient subgroups took analgesics or anti-inflammatories, 40.9% were treated with biologic DMARDS and 33.7% with a synthetic DMARD in monotherapy. With regard to satisfaction with treatments, 28.9% were not at all or little satisfied with them. When comparing this group with patients with low activity or remission RA, we see that the latter are significantly lower in age, have a lower impact in variables such as RAPID3, pain or fatigue and the more satisfied with disease modifying treatments (Table 6). However, there were no differences between groups in the percentages of patients with synthetic and biologic DMARDS.
Main characteristics of the patients with high levels of activity included in the RA 2020 survey.a.
| High activity (n = 466) | Remission/low activity (n = 153) | P value | |
|---|---|---|---|
| Sex (woman) | 411 (88.2) | 135 (88.2) | .990 |
| Current ageb(years) | 51 ± 11 | 48 ± 11 | .004 |
| Age at RA diagnosisb(years) | 38 ± 14 | 37 ± 13 | .287 |
| Duration of RAb(years) | 13 ± 12 | 11 ± 8 | .548 |
| RAPID3b(0−10) | 4 ± 1,5 | .8 ± .8 | <.0001 |
| Painb(0−10) | 6,8 ± 1.5 | 1.5 ± 1.1 | <.0001 |
| OPAb(0−10) | 6.5 ± 1.5 | 1.2 ± .9 | <.0001 |
| Fatigueb(0−10) | 6.9 ± 1.8 | 2.5 ± 2.3 | <.0001 |
| Morning stiffness | 379 (81.3) | 49 (32.0) | <.0001 |
| Analgesics/anti-inflammatories | 346 (83.7) | 65 (47.8) | <.0001 |
| Glucocorticoids | 231 (56.1) | 28 (20.6) | <.0001 |
| Synthetic DMARD | 271 (65.6) | 96 (70.6) | .838 |
| Biologic DMARD including biosimilars | 169 (40.9) | 57 (41.9) | .838 |
| JAK inhibitors | 31 (7.5) | 7 (5.1) | .347 |
| Treatment modifier (synthetic DMARD. biologics) | 350 (75.1) | 124 (81.0) | .132 |
| Combinations or monotherapy | .307 | ||
| Biologic DMARD + synthetic DMARD | 97 (20.8) | 31 (20.3) | |
| Biologic DMARD monotherapy | 65 (13.9) | 25 (16.3) | |
| JAK inhibitor + synthetic DMARD | 16 (3.43) | 4 (2.6) | |
| JAKi inhibitor monotherapy | 15 (3.22) | 3 (1.9) | |
| MTX monotherapy | 109 (23.4) | 49 (32.0) | |
| MTX monotherapy | 109 (23.4) | 49 (32.0) | |
| Satisfaction with modifying treatment | <.0001 | ||
| Completely satisfied | 9 (2.6) | 33 (26.6) | |
| Very satisfied | 76 (21.7) | 69 (55.6) | |
| Moderately satisfied | 164 (46.9) | 20 (16.3) | |
| A Little satisfied | 68 (19.4) | 2 (1.6) | |
| Not satisfied at all | 33 (9.43) | – |
DMARD: disease-modifying anti-rheumatic drug; JAK: janus kinase; MTX: methotrexate; OPA: overall patient assessment of the disease; RA: rheumatoid arthritis.
Results are expressed as numbers and percentages (%) unless otherwise indicated.
A RA activity index was created based on the sum of the average RAPID3, pain and OPA (scale 0–30) score. The result was classified in: remission (0–3), low activity (4–6), moderate activity (7–12), high activity (13–30). The result referring to the 466 patients of the “high activity” are contained in the table.
On the other hand, a total of 176 patients (19.9%) presented with an RA of recent onset (≤ 2 years of evolution). 89.2% were women, with a mean age of 49 ± 10 years. The mean of the RAPID 3 was 2.81 ± 1.78, that of pain was 5.08 ± 2.49, that of fatigue 5.72 ± 2.45 and that of OPA was 5.12 ± 2.44. In this subgroup of patients, the highest impact appears in the emotional area, which is severe or very high for 35.8% of patients, followed by the employment area, where the impact is severe or very high in 25% of them. Regarding treatment, 69% were being treated with a synthetic conventional or biological DMARD. We would highlight that over 50% have a synthetic conventional DMARD in monotherapy and that 9%, biological therapy (monotherapy or combination).
Finally, we should say that the most satisfied patients, compared with those who were not at all or were little satisfied, were considerably older, 50 years vs. 47 years (P = .003), presented with an RA of greater evolution than 12 years vs. 9 years (P < .001) and had a lower impact on variables such as RAPID3 (P < .001), pain (P < .001), fatigue (P < .001) and OPA (P < .001).
DiscussionThe results of this survey indicate that although advances in the approach to RA have brought about highly positive improvements in recent years, the impact of the disease continues being high for many patients. We would highlight the high impact certain symptoms such as fatigue, pain, morning stiffness and changes to functional ability continue to have on the everyday lives of patients. In our study it was also brought to our attention that somewhat over half of the patients surveyed presented with an active disease, for which almost a quarter of patients are without treatment with conventional synthetic DMARDs or biologics and also that very few patients are aware of the existing treatment alternatives.
To obtain these data we carried out a broad national survey which included a very high number of patients from all geographical areas of Spain, whose socio-demographic and clinical characteristics are fairly similar to those reported in observational studies in Spain, although some details should be qualified.16 The mean age on diagnosis and the mean current age could be lower than those regularly reported. This may be due both to the fact that both in ConArthritis and the in-patient platform there are young patients (or their parents) and many of the studies on prevalence/frequency and RA characteristics are focused on rheumatology services which cater for adult but not paediatric patients. Also, young people have better control of new technologies with the result that in our survey this subgroup could have been somewhat over-represented. Equally, the percentage of women is also higher than that normally reported in RA. Women are usually more cooperative regarding this type of initiative, and the percentage of them in our sample is higher than that established for RA.
At present, the healthcare model for chronic diseases such as RA includes patient-centred holistic care. If the patient is the centre of the healthcare system, it is important to know how they are experiencing their disease, what their opinion is regarding everything about RA itself and what their objectives and priorities are.17,18 In this context, aspects such as patient empowerment, active involvement in disease management or the taking of shared decisions become highly relevant.19,20 For all of this, many clinical practice guidelines define the final purpose of care for the RA patient as optimization of their quality of life and to achieve this aim, they recommend a series of guidelines or recommendations for taking clinical decisions. In addition to the assessment of objective parameters such as inflammation or structural damage, these guidelines consider patient opinion, uncovered needs, expectations and preferences.5
As we have described, one of the objectives of this survey was to analyse RA patients’ current experience so as to help shared decision-making to take place. Within the aspects assessed, we focused on those which, although always present, are in the current context where they are becoming of greater importance, either because others have been resolved or because everything relating to the patient is increasingly more relevant. Among them is pain, fatigue, morning stiffness and altered function. We have stated that the impact of these is very higher, at a similar level and even in some cases higher than that provoked by joint inflammation. Moreover, most of these variables are patient reported outcomes (PRO), which are subjective but have been reported by different studies to have a good correlation with objective variables,21–23 as well as reflecting the patient’s experience.
Another important finding is the high percentage of patients with high disease activity, assessed with an index based on RAPID3. We would also underline that in this subgroup of patients, up to a quarter of them state they have not been in treatment with a DMARD (synthetic or biologic) and many of them are not satisfied with their treatment. Since this was a self-completion questionnaire we cannot rule out a certain degree of under-scoring. Data from the EmAR II24,25 study indicate that the percentage of patients currently being treated with DMARDs is higher, although it does not cover the total patients. Furthermore, this study also showed that the use of conventional synthetic DMARDs during the previous 2 years as fewer than 50% in almost half of the sample. The DAS28 mean of patients included in the EmAR II was 3.5. On comparing the characteristics of patients with high activity to those in remission or with low activity, we found that those with high activity were considerably older, had a worse impact in PRO and were less satisfied with the disease-modifying treatment. It was also observed that not all rheumatologists are following the treatment strategies that have been proven to be effective for addressing RA.26 All of the above indicates that we should continue working towards maximum implementation in our daily practice and thus improve the clinical situation of the patients. We believe it is very important to increase knowledge in implementation methodology, and to improve doctor-patient communication to reverse this situation.
With regard to the relationship between the doctor and the patient, although results in general suggest there is a good relationship between them, we found data that suggested there was room for improvement in some areas. For example, in the taking of shared decisions where all available treatment options were covered. We therefore believe it is important to follow all published recommendations.27
We also should comment on a series of limitations for this project. In the first place, its design. In the survey there may be a selection bias, making those patients who have more active or more severe diseases more ready to respond to it. Similarly, since they have used an on-line platform it is possible that some patients have no access to Internet or that due to their age or other conditioning factors they are non-users of new technologies. However, bearing in mind such a broad sample had been reached, and its characteristics, we trust that it would be fairly representative. Furthermore, most responses are subjective, and it is therefore always important to contextualize them. We also used a modified version of RAPID3 which adapts better to current conditions but which, is however, in itself not validated.
To sum up, in our current context, where we practice a holistic, early and aggressive approach with a wide and effective therapeutic arsenal, the impact (physical, emotional and social-occupational) impact of RA continues to be very high. We have shown that a large percentage of patients with RA continue presenting with a high disease activity with great impact in the PRO and who are not very satisfied with their treatment. For this reason we must continue working on RA management to optimise this situation.
FinancingThe AR2020 project was financed by the ConArthritis patient association.
Conflict of interestsEL received fees for research from Abbvie, Roche, Sanofi, BMS, Pfizer, Astellas, Celgene, Gebro, Lilly, Novartis, UCB, MSD. The other authors have no conflict of interests to declare.
We would like of offer our enormous thanks to all patients who participated in the survey, and to Dr. María Jesús García de Yébenes, for her contribution to the statistical analysis.
Please cite this article as: Alcaide L, Torralba AI, Eusamio Serre J, García Cotarelo C, Loza E, Sivera F. Estado, control, impacto y manejo actual de la artritis reumatoide según los pacientes: encuesta nacional AR 2020. Reumatol Clin. 2021. https://doi.org/10.1016/j.reuma.2020.10.006