Calciphylaxis has been defined as tissue sensitivity to calcification, described mainly in patients with chronic renal insufficiency, renal transplant, or parathyroid dysfunction. There are few cases described in patients with rheumatoid arthritis that do not suffer from renal failure or hyperparathyroidism. Another case is presented of calciphylaxis in a woman with inactive rheumatoid arthritis.
La calcifilaxis ha sido definida como una sensibilidad a la calcificación de los tejidos, descrita primariamente en pacientes con insuficiencia renal crónica, trasplante renal o disfunción de glándulas paratiroides. Existen pocos casos descritos de pacientes con artritis reumatoide, sin insuficiencia renal, ni disfunción paratiroidea. Nosotros presentamos otro caso en una mujer con artritis reumatoide inactiva.
Calciphylaxis has been defined as a sensitivity to tissue calcification affecting small and medium-sized vessels, especially of the skin, and causing necrosis.1 This rare phenomenon has been reported predominantly in obese women, and in association with chronic kidney disease, dialysis (in 90% of the cases), renal transplantation, parathyroid dysfunction, primary hyperparathyroidism, lymphoma, leukemia and multiple myeloma.2–5 The data on its association with rheumatoid arthritis in the absence of renal failure and hyperparathyroidism are limited.1,6–9
Objective: To report a case of calciphylaxis in a patient with inactive rheumatoid arthritis without renal failure or hyperparathyroidism.
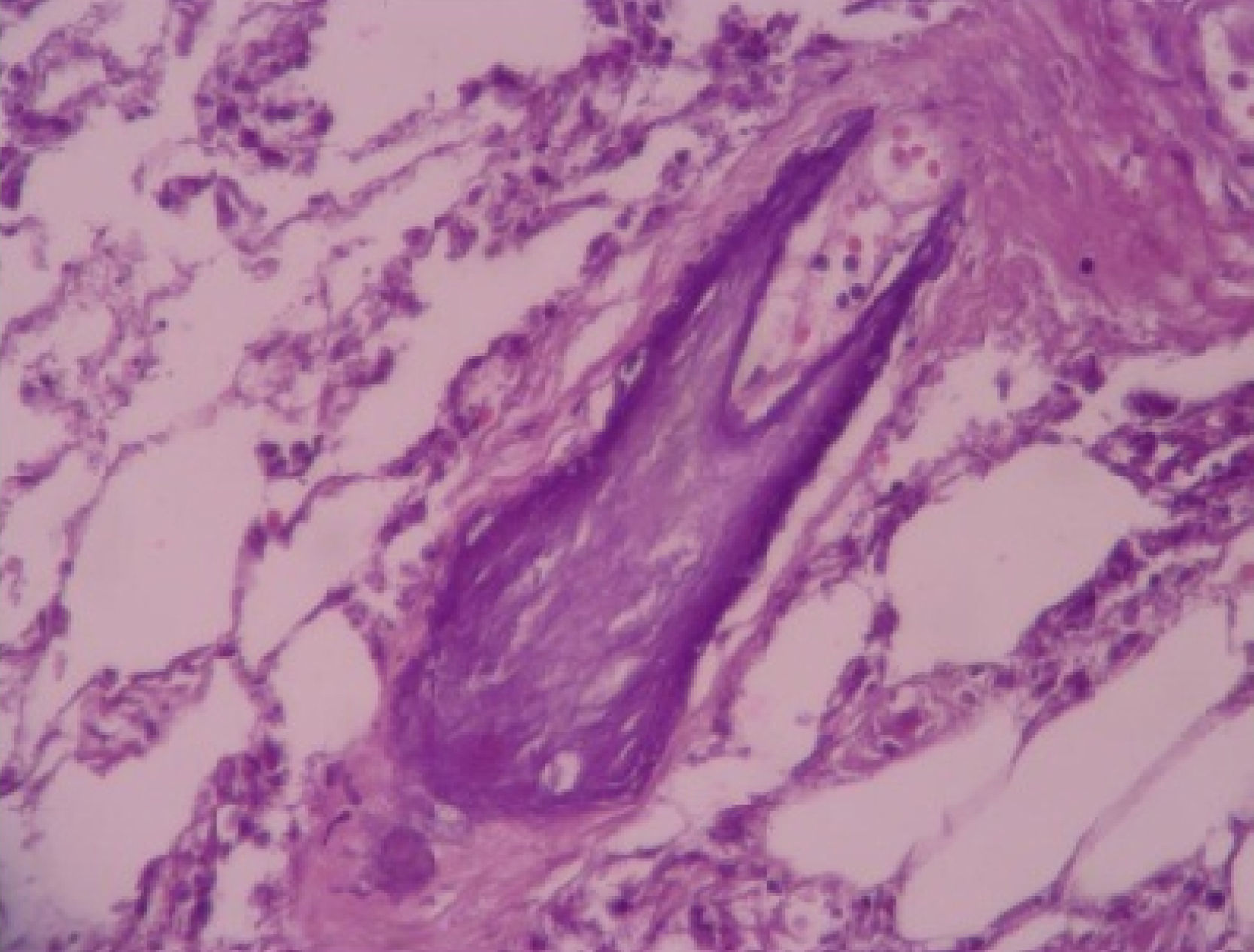
Case ReportThe patient was a 52-year-old woman who presented with a 5-year history of seropositive rheumatoid arthritis (1987 American College of Rheumatology criteria), but no evidence of erosive or nodular disease. She had been hospitalized in 2011 for necrotic, erythematous, vesicular lesions on her left leg, and physical examination revealed necrotic eschars on that leg (Fig. 1). Aside from inactive rheumatoid arthritis, the remaining findings were normal.
At the time of admission, the patient was receiving the following treatment: methotrexate 15mg/week, leflunomide 20mg/day, prednisone 4mg/day, folic acid 1mg/day and calcium+vitamin D. Laboratory tests showed normal serum calcium and phosphate levels, and blood culture, urine culture and serological tests for hepatitis B and C virus were negative. There was nothing abnormal on chest radiography, and color Doppler imaging of her left leg, performed twice, ruled out the presence of arterial or venous thrombosis.
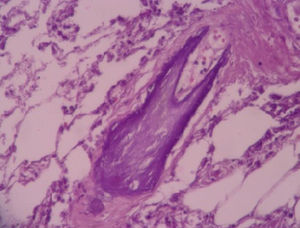
A biopsy of skin from the anterior aspect of the left leg revealed vascular mural calcification and luminal thrombosis, findings consistent with calciphylaxis (Fig. 2). Cultures of the biopsy specimen ruled out the presence of fungi, mycobacteria and other microorganisms.
The patient responded favorably to local treatment and general care and, at the time of this writing, had had no recurrences.
DiscussionCalciphylaxis should be considered a vascular disease, with intimal proliferation and fibrosis, associated with generalized or localized calcium deposition, together with inflammation and sclerosis.1 In contrast to calcinosis or calcified metastases, which can also be found in patients with renal failure or collagen vascular diseases, calciphylaxis is associated with endovascular fibrosis, ischemia and thrombosis.10
The true syndrome of calciphylaxis is characterized by its development in 3 phases: (1) sensitization produced by calcium mobilizing agents, such as vitamin D and parathyroid hormone, or interventions like bilateral nephrectomy; (2) the critical period of latency between sensitization and the induction of calciphylaxis; and (3) the action of induction agents which, when applied locally, produce a response in the skin or connective tissue (local calciphylaxis) but, if administered parenterally, trigger responses in different organs.11
There are 2 patterns of clinical distribution: central, the more common, affecting the trunk, with a mortality rate of 86%, and peripheral, which affects the limbs and penis, with a mortality of 32%.1,12 The distribution of the lesions in our patient was peripheral, and she had inactive rheumatoid arthritis, in the absence of renal failure or hypercalcemia. However, she was being medicated with sensitizers, such as calcium and vitamin D, and inducers, like glucocorticoids and methotrexate. Thrombosis was ruled out as the cause of the lesions, as were hepatitis B and C viruses. The biopsy did not reveal the typical thrombus found in antiphospholipid syndrome. The presence of multiple calcifications in the walls of small and medium-sized vessels was conclusive for the diagnosis.
In these patients, the rate of mortality due to sepsis is high. Treatment consists of local care of the wounds, correction of the internal medium and adequate hydration and nutrition.12
Nonuremic calciphylaxis associated with other connective tissue diseases is rare; in fact, there have been only 2 reported cases of calciphylaxis and giant cell arteritis.13
Given that calciphylaxis is one of the mimickers of vasculitis, it should be considered in the differential diagnosis of vasculitis, cholesterol crystal embolization, atrial myxoma, amyloidosis, endocarditis, cocaine-induced skin necrosis, warfarin-induced skin necrosis, Buerger's disease, panniculitis, angiotropic lymphoma, antiphospholipid syndrome, hypereosinophilic syndrome, levamisole-induced vasculitis, Degos disease and thrombocytopenic thrombotic purpura, among other causes of skin necrosis.14,15 As 5 similar cases have been described in the literature,1,6–8 one of which was reported by our group,9 we stress the importance of considering this diagnosis as a possible complication in rheumatoid arthritis and differentiating it from other causes of skin necrosis.
Although calciphylaxis is more frequent in patients with renal failure undergoing dialysis and/or disorders of calcium and phosphorus metabolism, the report of this disease in 5 patients with rheumatoid arthritis, some of whom did not have renal failure or conditions affecting calcium and phosphorus metabolism, alerts us to the need to take this entity into account in patients with rheumatoid arthritis and necrotic skin lesions. In view of the poor outcome of these patients, diagnosis and prompt initiation of treatment are essential.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingThe authors have received no funding of any type for the work involved in this study.
Conflicts of InterestThe authors declare they have no conflicts of interest.
Please cite this article as: Ortiz A, Roverano S, Gallo J, Henares E, Eletti M, Paira S. Calcifilaxis asociada a artritis reumatoide: comunicación de otro caso. Reumatol Clin. 2016;12:158–160.