Leukocytoclastic vasculitis is the most common cause of cutaneous vasculitis in clinical practice. Its causes are various, among which are certain infections. We report the case of a man (28 years old) who debuted with vasculitic lesions in inferior members compatibles leukocytoclastic vasculitis on pathology. The study of causation is the presence of a positive urethral discharge to Ureaplasma urealyticum, dramatically improving lesions after treatment thereof.
La vasculitis leucocitoclástica es la causa más frecuente de vasculitis cutánea en la práctica clínica. Sus causas son diversas, entre las que se encuentran ciertas infecciones.
Presentamos el caso de un varón de 28 años que debuta con lesiones vasculíticas en miembros inferiores, compatibles con una vasculitis leucocitoclástica en la anatomía patológica. En el estudio de causalidad se encuentra la presencia de un exudado uretral positivo a Ureaplasma urealyticum, mejorando drásticamente las lesiones tras el tratamiento del mismo.
Cutaneous vasculitides are inflammatory disorders affecting the wall of the vessels of the skin. There can be a number of causes (drug exposure, infection, neoplastic disease or systemic inflammatory disease),1 and skin involvement may be its only manifestation.
Leukocytoclastic vasculitis is the most frequent cause of cutaneous vasculitis found in clinical practice.1 On occasion, it can be associated with constitutional symptoms, and thus be confused with systemic diseases and certain conditions like mycoplasma.1
Ureaplasma, which belongs to the same family as Mycoplasma, is associated, in adults, with genital infections like nongonococcal urethritis.2
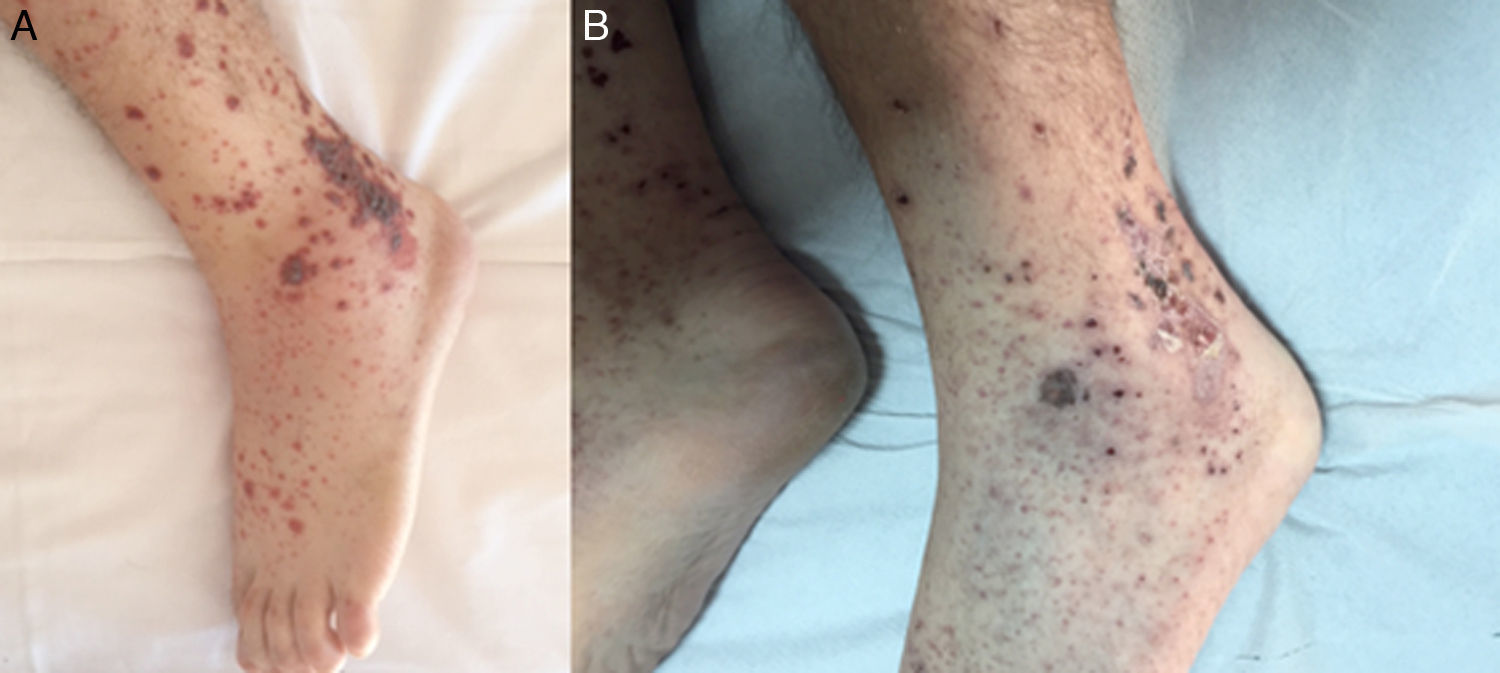
Clinical ObservationWe present the case of a 28-year-old man who had no significant previous medical history. He presented at the emergency service with lesions in the skin on lower limbs and trunk that did not disappear when pressed by a finger. The patient had no other systemic symptoms. He did not have fever or signs of infection anywhere else, except certain genital symptoms that were not well defined. He denied the use of drugs, sexual risk behavior and the consumption of any type of medication. He had arthralgia but not arthritis and, on the level of the skin, he had flat, erythematous, nonpruritic lesions, together with other bullous lesions (Fig. 1). He underwent a skin biopsy which revealed leukocytoclastic vasculitis (perivascular inflammatory infiltrate with predominance of neutrophils, and nuclear dust, fibrinoid degeneration and extravasated red blood cells; subepidermal blisters with hemorrhagic and pustular content and focal epidermal necrosis). The analytical study, which involved acute-phase reactants, complete blood count and biochemical and immunological data, was normal. A urine culture was negative, as were serological tests for the hepatotropic viruses. Colonies of Ureaplasma urealyticum were identified in the urethral exudate. At admission, treatment was begun with prednisone (30mg/day) and a nonsteroidal anti-inflammatory drug (ibuprofen at 600mg every 8h). This was followed by clinical improvement; however, it did not persist until antibiotic therapy was initiated with doxycycline, in accordance with antibiogram indications for Ureaplasma. Steroids were discontinued after 1 month and, 6 months later, the patient was asymptomatic without treatment.
DiscussionLeukocytoclastic vasculitis is the most common cutaneous vasculitis. Although in 50% of the cases, the cause is usually idiopathic, the histopathological diagnosis enabled by biopsy should be established as soon as possible to rule out other possibilities such as systemic, neoplastic or infectious diseases.1,3–5 Nevertheless, the term “leukocytoclastic vasculitis” does not specify the exact diagnosis.4,5 In sexually active patients, we cannot forget that sexually transmitted diseases, which include Ureaplasma infection, can be asymptomatic and are related to a wide variety of pathological settings, one of which is leukocytoclastic vasculitis.2
With regard to the treatment of leukocytoclastic vasculitis, the first situation that should be treated is the triggering factor,1Ureaplasma infection in our patient, leaving immunosuppressive therapy for cases that are refractory or in which the involvement is severe.3
ConclusionsThere are many factors that can be associated with leukocytoclastic vasculitis as triggers of the disease.
Infections are a frequent cause of cutaneous vasculitis and joint involvement.
There are infections in which the symptoms are less evident that should be taken into account in the examination of our patients, because there may be a causal relationship.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of InterestThe authors declare they have no conflicts of interest.
Please cite this article as: Moreno Martínez MJ, Palma Sánchez D, Peñas Martínez E, Haro Martínez A, Mayor González M. Vasculitis leucocitoclástica e infección. A propósito de un caso. Reumatol Clin. 2017;13:297–298.