The aseptic displacement of a prosthesis is one of the most common complications of orthopedic surgery; sometimes patients require reintervention.
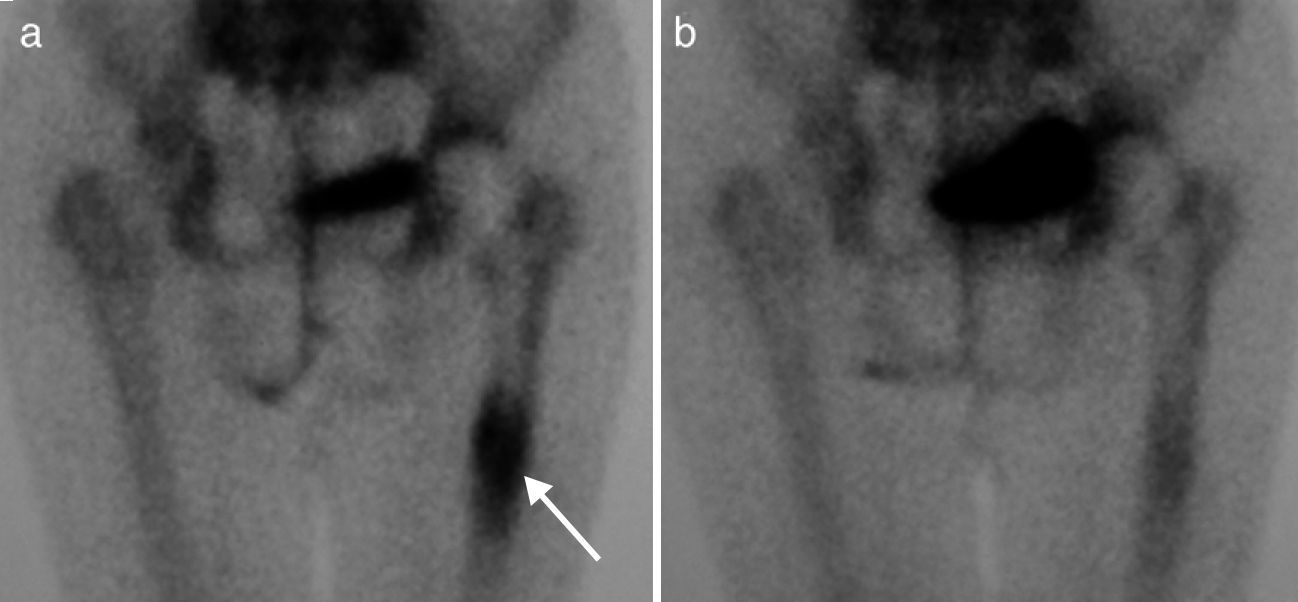
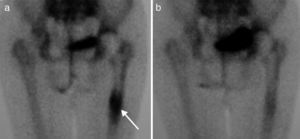
We report the case of an 83 year old woman with a history of postmenopausal osteoporosis with weekly bisphosphonate treatment and daily intake of calcium and vitamin D and a hip fracture right at 64, treated with a cemented prosthesis. She attended the clinic due to mechanical right hip pain with claudication, progressing in months. On examination we found limitation and pain on right hip rotation. We performed a hip X-ray (Fig. 1) and, suspecting aseptic displacement of the prosthesis, bone scintigraphy was performed in 3 phases showing uptake in the distal third (Fig. 2a), confirming the diagnosis. We started treatment with strontium ranelate plus calcium and vitamin D. After 2 months, the patient improved significantly and her claudication disappeared. At 6 months, the bone scan was repeated, which showed a reduction to close to normal of the increased uptake seen at baseline (Fig. 2b).
Due to the aging of the population, there is an increase of patients undergoing joint replacement surgery. Stable and lasting fixation of the prosthesis depends, among other factors, on the surgical technique used, the characteristics of the implant surface which contacts the bone and bone quantity and quality in the patient. One of the most common complications is the displacement of the prosthesis, especially in patients with osteoporosis. It is therefore expected that therapies directed at improving bone microarchitecture and increase bone mass facilitate osteointegration of the prosthesis.1
Strontium ranelate, used to prevent osteoporotic fractures,2 has been shown effective in improving prosthesis osteointegration in animals.3,4 However, to date there are no studies assessing its effects in humans for this same purpose. Thus, the case presented here provides data suggesting that strontium ranelate can be beneficial for osteointegration of a hip prosthesis. The substantial improvement in symptoms just 2 months after treatment onset with normalization of bone scan at 6 months are promising and suggest its potential application in orthopedic surgery.
Conflict of interestThe authors have no conflict of interest to declare.
Please cite this article as: León Rubio P, Baturone Castillo M. El ranelato de estroncio mejora la osteointegración de una prótesis de cadera. Reumatol Clin. 2013;9:326–327.