To adapt cross-culturally and validate the COPCORD methodology in the indigenous Wayuu population of Zulia state, Venezuela.
MethodologyA cross-sectional study was conducted on Wayuu indigenous people from the Mara and Guajira municipalities of the state of Zulia, Venezuela. The Venezuelan version of the COPCORD questionnaire was transculturally adapted and translated from Venezuelan Spanish to Wayuunaiki (Wayuu language). One hundred indigenous Wayuu, agreed to participate, they were administered the instrument, house by house, by health personnel, who were bilingual and previously trained. Positive COPCORD individuals were evaluated by rheumatologists. A descriptive analysis of variables was performed, Cronbach's alpha was measured, Spearman's correlation, screening test analysis (sensitivity, specificity, VPP and SVR +).
Results66% were women, average age 41.4 years, 20% monolingual, 21% illiterate, 69% in a couple/married, 57% with informal work. Sixty-two percent reported pain, 56% with criteria of rheumatic diseases, the most frequent were: osteoarthritis (32.3%), mechanical lower back pain (13.9%), and regional rheumatic pain syndrome (12.3%). Five dimensions of the instrument presented Cronbach's alpha> .7. The sensitivity was 100% and specificity 11.1%, VPP 14.3%, SVR + 1.13%.
ConclusionThe COPCORD is valid and useful as a screening tool for the detection of musculoskeletal complaints and rheumatic diseases in the indigenous Wayuu population.
Adaptar transculturalmente y Validar la metodología COPCORD en población indígena Wayuu del estado Zulia, Venezuela.
MetodologíaSe realizó estudio de corte transversal, en indígenas Wayuu, de los municipios Mara y Guajira del estado Zulia, Venezuela, se adaptó transculturalmente la versión venezolana del cuestionario COPCORD y se tradujo del español venezolano al wayuunaiki (idioma Wayuu). Cien indígenas Wayuu, aceptaron participar, se les administró el instrumento, casa por casa, por personal de salud, bilingüe capacitado. Los individuos COPCORD positivos fueron evaluados por reumatólogos. Se realizó análisis descriptivo de variables, se midió alfa de Cronbach, correlación de Spearman, análisis de prueba de cribado (sensibilidad, especificidad, VPP y RVS+).
ResultadosEl 66% fueron mujeres, edad promedio 41,4 años, 20% monolingües, 21% analfabetas, 69% unidos/casados, 57% con trabajo informal. El 62% reporto dolor, 56% con criterios de enfermedades reumáticas, las más frecuentes fueron: osteoartritis (32,3%), lumbalgia mecánica (13,9%) y síndrome doloroso regional reumático (12,3%). Cinco dimensiones del instrumento presentaron alfa de Cronbach >0,7. La sensibilidad fue de 100% y especificidad 11,1%, VPP 14,3%, RVS + 1,13%.
ConclusiónEl COPCORD es válido y útil como herramienta de cribado para la detección de malestares musculoesqueléticos y enfermedades reumáticas en la población indígena Wayuu.
Rheumatic diseases affect the musculoskeletal system, and express clinically with pain, stiffness, inflammation and decreased joint mobility, with potential for disability and invalidity, at high economic and social cost.1
The International League of Rheumatology Associations (ILAR), together with the World Health Organization (WHO), created the Community Oriented Programme for the Control of Rheumatic Diseases (COPCORD) at the end of 1980 with the purpose of assessing pain and disability, establishing possible risk factors, and helping to correct epidemiological information deficit, particularly in developing countries.2
COPCORD is a simple and reliable method, widely applied in countries in Asia, Africa, the Middle East, Australia, and Latin America. It comprises three stages: Stage I: community survey to obtain data from the population studied (symptom register, socio-economic information, HAQ-DI (Health Assessment Questionnaire Disability Index) and the evaluation by rheumatologists of positive COPCORD individuals). Stage II: identifies risk factors. Stage III: establishes control and prevention strategies.3
The design of COPCORD allows for standardised epidemiological records. However, there are regional variations in the prevalence of musculoskeletal pain and disorders recorded using this methodology, probably due to ethnic diversity and genetic or geographical differences. The application of this instrument in indigenous populations merits its adaptation to the socio-cultural context, since the perception of health/disease may vary according to cultural patterns, beliefs, preferences in medical care or difficulty in accessing different levels of medical care.4
Numerous COPCORD studies have been carried out in mixed-race, urban, and rural populations in Latin America.5,6 In recent years this effort has also been directed at indigenous populations, and in this regard the Latin American Study Group on Rheumatic Diseases in Indigenous Peoples (GLADERPO) has reported interesting data on musculoskeletal disorders and rheumatic diseases in many ethnic groups in Mexico, Venezuela, and Argentina.7–13
Venezuela shows diversity in the socio-cultural and linguistic expression of the 52 indigenous peoples in the country, who have high morbidity rates and health risks. Improving their conditions and guaranteeing their access to primary care requires expanding epidemiological information, understanding the indigenous worldview, and incorporating health programmes with an intercultural approach.
The Wayuu represent 61.21% of the total indigenous population of Venezuela, for whom epidemiological data on rheumatic diseases are unknown. It is particularly important that studies in this population are conducted using a reliable instrument for early diagnosis of these diseases. The objective of this work was the transcultural adaptation and validation of the COPCORD methodology in the Wayuu population.
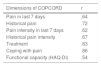
Materials and methodsDesignThe cross-cultural adaptation of the Venezuelan Spanish version of the COPCORD questionnaire and adjustment of its content during the translation and backtranslation process (Spanish/ Wayuunaiki, native language) were carried out, taking the Wayuu’s most common customs, lifestyles, and comorbidities into account. To achieve the final version, the proposals of Beaton et al.14 and the seven stages they establish were followed: Stage 1: initial translation of the instrument by two independent translators. Stage 2: translation summary, evaluation by committee of bilingual experts and administration to 5 indigenous people. Stage 3: backtranslation of the Wayuunaiki into Spanish by two bilingual translators. Stage 4: revision by a committee of experts of both backtranslations, administration of second version to 20 indigenous people. Stage 5: testing of the pre-final version. Stage 6: monitoring of the recommended stages until a final translation is obtained. Stage 7: validation of the final version (Fig. 1).
COPCORD questionnaireThe COPCORD questionnaire has several sections including: explanation of the study, demographic information, comorbidities, recent pain (last 7 days), historical pain (at some point in life), anatomical location of the pain on a dummy, pain intensity assessed by visual analogue scale (VAS) with values from 0 to 10, duration and behavioural patterns of pain, search for care, functional limitation, pain adaptation and functional capacity measured by HAQ-DI.15
Administration of the Wayuu version of COPCORDBilingual (Spanish-Wayuunaiki) health personnel, previously trained in the COPCORD methodology, applied the instrument, house by house, to 100 Wayuu indigenous people of both sexes, over 18 years of age.
Certified rheumatologists evaluated positive COPCORD individuals over a period of 7 days (recent or historical reports of pain, stiffness, or inflammation [VAS ≥ 1], not related to trauma) and made diagnoses according to international criteria. They used American College of Rheumatology (ACR) criteria for the diagnosis of osteoarthritis of the hands and knees,16,17 rheumatoid arthritis,18 systemic lupus erythematosus,19 modification of the New York criteria for the diagnosis of ankylosing spondylitis20 and the Wallace criteria for the diagnosis of gout.21 Pain without classification criteria was called musculoskeletal disorder and was recorded according to the International Classification of Diseases (WHO-ICD-10).22
PopulationThe Wayuu, an indigenous people who live on the Guajira Peninsula between Colombia and Venezuela, are the most numerous ethnic group in Venezuela. They are in the state of Zulia, grouped in small communities, distant from each other, called rancherías. Their main economic activities include herding, agriculture, fishing, trade, and textiles.23
Ethical aspectsThe provisions of the Organic Law on Indigenous Peoples and Communities of the Bolivarian Republic of Venezuela were complied with. The Ethics and Research Committee of the Hospital Central Dr Urquinaona, Maracaibo, Zulia State, approved the study. All participants signed or validated with their fingerprint their informed consent.
Statistical analysisDescriptive analysis was conducted for continuous and dichotomous or ordinal variables; continuous variables are reported in measures of central tendency and dispersion, and proportions for dichotomous or ordinal variables.
To analyse the validity of the questionnaire, internal consistency was measured with Cronbach’s α coefficient: values below .70 were considered multidimensional and those above .70 were considered one-dimensional. Reliability, reproducibility, and criterion validity were analysed with Spearman’s correlation.
We performed an analysis of the instrument’s usefulness as a screening test, evaluated sensitivity, specificity, likelihood ratio (LR), positive predictive value (PPV), areas under the curve (ROC), and 95% confidence intervals. We used SPSS 22 (Statistical Package for the Social Sciences) for Windows.
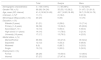
ResultsA final version of COPCORD adapted to the Wayuu cultural context was achieved without departing from the original content and was administered between March and November 2017 to 100 indigenous people from the Mara (52%) and Guajira (48%) municipalities in the state of Zulia, Venezuela. Sixty-six percent were women, the average age was 41.4 years (18−89 years), 21% were illiterate and 17% had 16 years or more of education. Twenty percent spoke only their native language, 28% were in formal employment (Table 1).
Demographic characteristics of the indigenous Wayuu population.
| Total | Guajira | Mara | |
|---|---|---|---|
| Demographic characteristics | n = 100 (100%) | n = 48 (48%) | n = 52 (52%) |
| Gender F/M, n (%) | 66 (66) /34 (34) | 35 (53) /13 (38.2) | 31 (47) / 21 (61.8) |
| Age, mean (SD; interval) | 41.4 (16.56;18−89) | 45.7 (16.83;18−89) | 36.7 (15.09;18−76) |
| Unknown, n (%)a | 11 (11) | 2 (18.2) | 9 (81.8) |
| Monolingual (Wayuunaiki), n (%) | 20 (20) | 6 (30) | 14 (70) |
| Education, n (%) | |||
| Illiterate (0 years) | 21 (21) | 6 (28.6) | 15 (71.4) |
| Primary (1−6 years) | 38 (38) | 13 (34.2) | 25 (65.8) |
| Secondary(7−10 ) | 10 (10) | 5 (50.0) | 5 (50.0) |
| High school (11 years) | 14 (14) | 11 (78.6) | 3 (21.4) |
| University (16 years) | 17 (17) | 13 (76.5) | 4 (23.5) |
| Marital status, n (%) | |||
| Married/Partner | 69 (69) | 33 (47.8) | 36 (52.2) |
| Separated | 12 (12) | 4 (33.3) | 8 (66.6) |
| Widowed | 9 (9) | 6 (66.7) | 3 (33.3) |
| Single | 10 (10) | 5 (50.0) | 5 (50.0) |
| Employment, n (%) | |||
| Formal | 28 (28) | 15 (53.6) | 13 (46.4) |
| Informal | 57 (57) | 27 (47.4) | 30 (52.6) |
F: Female; M: Male; SD: Standard Deviation.
Source: COPCORD instrument adapted to the Wayuu population.
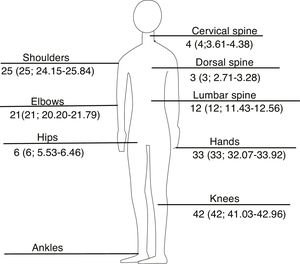
Sixty-two individuals were COPCORD positive (.62; 95% CI: .51–.71), of whom 56 (90.32%) met criteria for rheumatic diseases. The most frequent diagnoses were osteoarthritis (32.3%), other arthropathies (20%), mechanical back pain (13.9%) and appendicular regional pain syndrome (12.3%) (Table 2). The most frequent areas of pain were the knees (42%; 41.033–42.967), hands (33%; 32.078–33.922) and shoulders (25%; 24.151–25.847) (Fig. 2).
Most frequent rheumatological diagnoses.
| Diagnoses | n (%) |
|---|---|
| Osteoarthritis | 21 (32.3) |
| Other arthropathies | 13 (20.0) |
| Mechanical back pain | 9 (13.9) |
| Appendicular regional pain syndrome | 8 (12.3) |
| Polyarthritis | 5 (7.7) |
| Poly- and oligoarticular syndrome | 5 (7.7) |
Source: COPCOR instrument adapted to the Wayuu population.
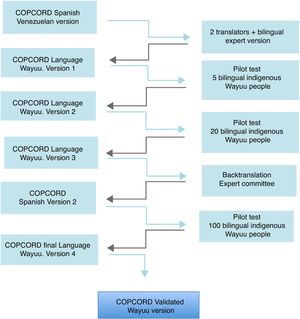
An internal consistency analysis of COPCORD found that Cronbach's alpha presented one-dimensional values from .7 for the trajectory of pain or inflammation to .9 for the characteristic of pain (Table 3).
Internal consistency of the COPCORD instrument.
| Dimensions of the COPCORD | Cronbach’s alpha | Items |
|---|---|---|
| Personal data | .2 | 11 |
| Comorbidity | .2 | 3 |
| Employment historya | .8 | 4 |
| Pain trajectory, inflammation | .7 | 10 |
| Treatment | .7 | 4 |
| Functional capacity (HAQ-DI) | .9 | 3 |
HAQ-DI: Health Assessment Questionnaire-Disability Index.
In the analysis of criterion validity, the highest correlation index was reported for the variables adaptation to pain (.86) and treatment (.83) (Table 4).
Spearman’s correlation to measure the COPCORD instrument’s criterion validity.
| Dimensions of COPCORD | r |
|---|---|
| Pain in last 7 days | .64 |
| Historical pain | .72 |
| Pain intensity in last 7 days | .62 |
| Historical pain intensity | .67 |
| Treatment | .83 |
| Coping with pain | .86 |
| Functional capacity (HAQ-DI) | .54 |
HAQ-DI: Health Assessment Questionnaire-Disability Index.
Source: COPCORD instrument adapted to the Wayuu population.
In assessing the usefulness of the questionnaire as a tool for detecting rheumatic diseases, we obtained 100% sensitivity and specificity with values from 11.1%, a PPV of 14.3, an LR of 1.1 and an area under the curve of 78% (95% CI: 71−85). The values for each of the rheumatic diseases are shown in Table 5.
Performance of the COPCORD instrument as a screening tool for musculoskeletal disorders and rheumatic diseases.
| Sensitivity (%) | Specificity (%) | PPV (%) | NPV(%) | LR+ (%) | AUC (%; IC 95%) | |
|---|---|---|---|---|---|---|
| Rheumatic diseasea | 100 | 11.1 | 14.3 | 100 | 1.13 | 78; 71−85 |
| Musculoskeletal disordersb | 100 | 13.6 | 32.1 | 100 | 1.16 | 62; 57−68 |
| Osteoarthritis | 100 | 14.6 | 37.5 | 100 | 1.17 | 54; 45−63 |
| Mechanical back pain | 100 | 11.3 | 16.1 | 100 | 1.13 | 53; 46−59 |
| Appendicular regional pain syndrome | 100 | 11.1 | 14.2 | 100 | 1.13 | 56; 49−62 |
AUC: Area under the curve; 95% CI: 95% Confidence Interval; LR: Likelihood Ratio; NPV: Negative Predictive Value; PPV: Positive Predictive Value.
Numerous COPCORD studies conducted in various regions of the world have reported a high prevalence of rheumatic diseases. The cultural adaptation of this questionnaire and its application in various ethnic groups in Latin America showed that these are highly prevalent diseases in the indigenous population (34.5%),24 and that they impact the lives of individuals in their most productive stage.
The administration of the Wayuu version of COPCORD recorded 62% of musculoskeletal pain in the indigenous people surveyed, the average age was 41.4 years, like that reported in other ethnic groups studied in Venezuela25 and Latin American1; 11% of the Wayuu do not know their age and have their own classification that groups them into child, young, old, and very old.
The homogeneity and internal consistency of the instrument was demonstrated, as well as the one-dimensionality in the trajectory of pain and functional capacity by means of Cronbach's α, with reported values between .7 and .9, like that registered by Peláez-Ballestas et al.1 in indigenous populations of Venezuela, Mexico, and Argentina, and by Guevara Pacheco et al.6 in mixed race, rural and urban populations of Cuenca, Ecuador. The criterion validity analysis showed good correlation between diagnosis of disease and different variables, with higher indices for the variables adaptation to pain (.86) and treatment (.83); functional capacity recorded an index of .54, probably due to the greater adaptability to pain that they may present.
The Wayuu version of COPCORD allows us to adequately classify the population studied. Its application reported 100% sensitivity for rheumatic diseases, higher than that reported by Pelaez-Ballestas et al.1 in the Warao, Kariña, Chaima, Mixteco, Maya-Yucateca, Raramuri and Qom peoples (from Venezuela, Mexico, and Argentina), specificity was 11.1%, and the LR was 1.13 in rheumatic diseases, and 14.6% and 1.17 in osteoarthritis.
When we compare our study with others carried out in mixed-race populations, we find some differences. Al-Awadhi et al.26 reported sensitivity of 94.38% and specificity of 96.97%. In a validation study of the COPCORD core questionnaire (CCQ), carried out in Mexico, sensitivity was 84% and specificity 61.3%,15 but in this case a level of pain >4 according to VAS was accepted. Bennett et al.27 used the adaptation of the CCQ in Brazil, Chile, and Mexico: reported sensitivity was high in the three participating countries, and the lowest specificity was reported in Chile (35.5%) for recent pain; this result could be explained by differences specific to the operational development of the work.
Osteoarthritis was the most common rheumatic disease (32.3%), coinciding with COPCORD studies conducted in indigenous and mixed-race populations in Argentina (4,0%),7 Brazil (29%),27 Cuba (22.7%),28 Ecuador (27.3%)6 Guatemala (5.58%),29 Mexico (7.26%),5 Peru (15.2%)30 and Venezuela (14.1%).12 In this study, no cases of rheumatoid arthritis were detected, similar to that recorded in aboriginal populations in Australia,2 and different to that reported in indigenous Chaima in Venezuela and Qom in Argentina, with prevalence of 2% and 2.4%.7,25 Pain most frequently affected the knee, hand and shoulder regions, coinciding with that recorded in other indigenous populations of Venezuela, Mexico and Argentina.1
With this study, it was possible to demonstrate that the Wayuu version of COPCORD performs well as a tool to detect individuals with rheumatic diseases and is easily applicable in the indigenous Wayuu population.
Conducting community studies in locations that are remote from urban centres is a challenge for researchers due to the logistical complexity of the research, which increases if they also involve culturally and linguistically different communities. Both researchers and community participants have contrasting beliefs, therefore the doctor-patient relationship must adapt to the perception of health-illness-care.
This type of study implies an ethical commitment for researchers due to the vulnerability of these populations, as well as sensitivity and respect for the culture. We believe that studies should be carried out in culturally different populations to document differential prevalence, as well as community-based health needs and solutions.
LimitationsThis study had language limitations, as a significant number of the population studied spoke only their native language, and training of bilingual interviewers was required. The move to the participating communities demanded greater logistical and financial resources.
ConclusionsThe COPCORD methodology proved a useful tool for detecting rheumatic diseases in indigenous Wayuu people and made it possible to record 62% of musculoskeletal pain and disorders in this population, which calls for more extensive population studies.
Conflict of interestsThe authors have no conflict of interests to declare.
Sociologist José Fernández, Lic. Lucas Fernández and Lawyer Edixa Montiel (Wayuunaiki-English translators), Doctor in Linguistics José Álvarez, Dr Andrys Mayor, Dr José Manuel Beleño, Nurse Esmeira Gómez, Teacher Suhail Palmar and the Latin American Group for the Study of Rheumatic Diseases in Native Peoples (GLADERPO).
Please cite this article as: Beleño-Epieyu N, Granados Y, García Mac Gregor E, Márquez D, Guerra ME, Peláez Ballesta I. Adaptación transcultural y validación de la metodología del Programa Orientado a la Comunidad para el Control de Enfermedades Reumáticas (COPCORD) en población indígena Wayuu. Venezuela. Reumatol Clin. 2021;17:82–87.