Rheumatoid arthritis (RA) is a systemic inflammatory disease, with a chronic and variable evolution, characterized by persistent and symmetrical synovitis of the peripheral joints. In recent years its natural history has changed thanks to advances in treatment, so comorbidities have become more important; in fact, increased mortality compared to the general population is primarily a result of diseases of cardiovascular origin,1 with rates up to 50% or higher.
In RA underlying atherosclerotic disease is increased2 secondary to chronic inflammation, which involves activation of T lymphocytes and macrophages, production of proinflammatory cytokines3 (gamma interferon, tumor necrosis factor, IL-1 and IL-6). It is potentiated due to classic cardiovascular risk factors (CVRF), including the metabolic syndrome, which is more prevalent probably due to less physical activity because of joint pain and moreover, dyslipidemia follows a more atherogenic4 pattern.
With all these data, we conclude that the RA is a situation with a high CVR, where cardiovascular morbidity is related to the disease activity, so its control could reduce the risk.5 Therefore, this study proposes to detect subclinical CVD by measuring the ankle-brachial index (ABI).
We performed a descriptive cross-sectional study on 60 RA patients with no history of CVD, at the University Hospital of La Princesa, Madrid, selected consecutively in the rheumatology clinic during the 6 months when the study was carried out. Sociodemographic variables, analytical data, classic CVRF, duration of RA and immunomodulatory treatment were collected. ABI was defined as abnormal if less than 0.9.6
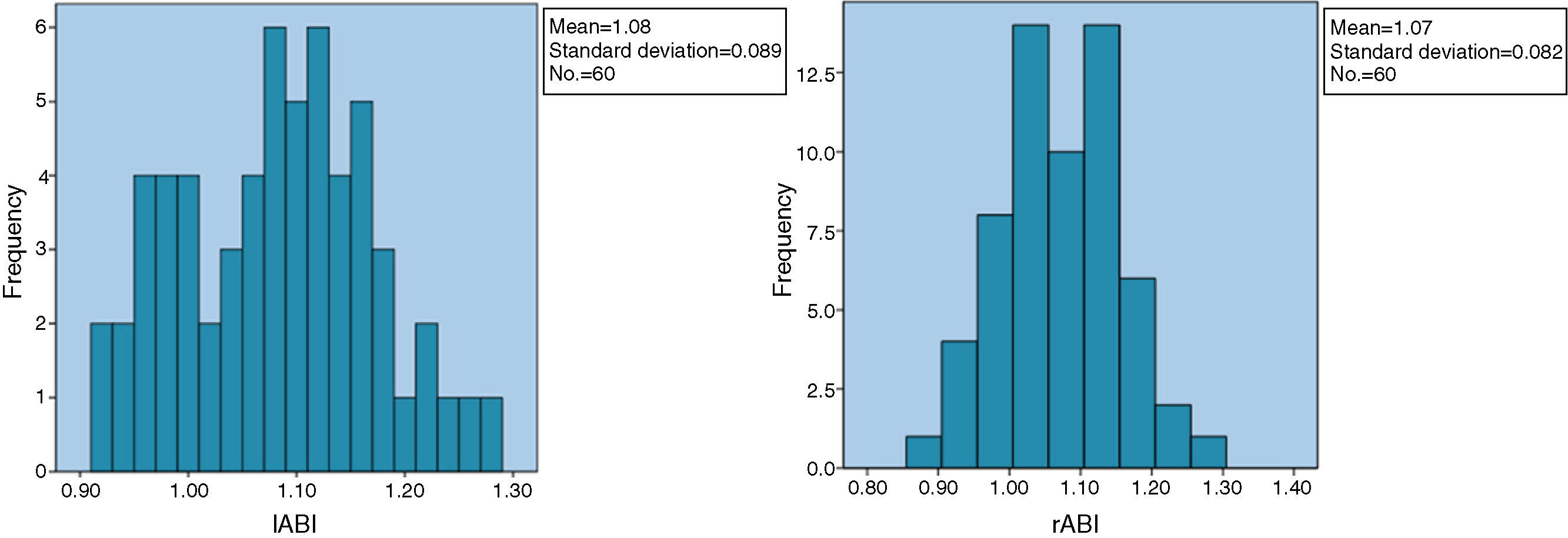
Of the 60 patients enrolled, 3 were men (5%) and 57 women (95%) with a mean age±standard deviation of 53.75 years (53.75±15.38, range 29–87). 38 had mild RA (63.3%), while 22 (36.7%) had important deformities. The time of disease progression was 9.14 years (9.14±6.505, range 0.6–40), 58 patients (96.7%) were under immunomodulatory therapy, mostly with methotrexate (75%). The result of the ABI was similar in both lower limbs: 1.074 (1.074±0.082, range 0.88–1.28) on the right and 1.077 (1.077±0.088, range 0.92–1.27) on the left, with no significant differences between them. Only one patient (1.7%) had an abnormal ABI: a woman of 87 years, with hypertension, and RA for 12 years and using corticosteroids during virtually all this time; the ABI on the other extremity was 0.92. Fig. 1 shows the ABI results.
In our sample, there is an overrepresentation of women (19:1) with respect to other RA populations (3:1). However, the profile of CVR did not differ regarding the Spanish general population.7 Only one pathological case was detected, much lower than other studies,8,9 with rates of 20%–25%, although the frequency cutoff point considered as pathological was 1, rather than the value of 0.9 currently accepted. However, in another publication with the same cutoff,10 the prevalence was 10%, although in their sample the mean age, duration of RA and, above all, the prevalence of cardiovascular risk factors (especially diabetes and dyslipidemia) were superior. Other possible factors involved could be the adequate control of the disease, since only 3.3% of patients had no specific treatment and the value of the acute phase reactants was normal.
A major limitation to the study was accessibility, as the ABI was performed after the patient visit, so many of the patients excluded were those who refused to participate, claiming physical difficulty to go and get tested, which may have been a selection bias, having lost the sickest patients.
In conclusion, based on our results we do not consider routine ABI testing justified in asymptomatic patients with RA from a cardiovascular point of view.
Please cite this article as: Marcos de Frutos C, Abad Pérez D, Suárez Fernández C. Utilidad del índice tobillo-brazo como método de cribado de enfermedad vascular subclínica en pacientes con artritis reumatoide. Reumatol Clin. 2014;10:268–269.