The cost of certain diseases may lead to catastrophic expenses and impoverishment of households without full financial support by the state and other organizations.
ObjectiveTo determine the socioeconomic impact of the rheumatoid arthritis (RA) cost in the context of catastrophic expenses and impoverishment.
Patients and methodsThis is a cohort-nested cross-sectional multicenter study on the cost of RA in Mexican households with partial, full, or private health care coverage. Catastrophic expenses referred to health expenses totaling >30% of the total household income. Impoverishment defined those households that could not afford the Mexican basic food basket (BFB).
ResultsWe included 262 patients with a mean monthly household income (US dollars) of $376 (0–18,890.63). In all, 50.8%, 35.5%, and 13.7% of the patients had partial, full, or private health care coverage, respectively. RA annual cost was $ 4653.0 per patient (65% direct cost, 35% indirect). RA cost caused catastrophic expenses in 46.9% of households, which in the logistic regression analysis were significantly associated with the type of health care coverage (OR 2.7, 95%CI 1.6–4.7) and disease duration (OR 1.024, 95%CI 1.002–1.046). Impoverishment occurred in 66.8% of households and was associated with catastrophic expenses (OR 3.6, 95%CI 1.04–14.1), high health assessment questionnaire scores (OR 4.84 95%CI 1.01–23.3), and low socioeconomic level (OR 4.66, 95%CI 1.37–15.87).
ConclusionThe cost of RA in Mexican households, particularly those lacking full health coverage leads to catastrophic expenses and impoverishment. These findings could be the same in countries with fragmented health care systems.
El costo de ciertas enfermedades puede dar lugar a gastos catastróficos y el empobrecimiento de las familias sin apoyo financiero por los organismos del Estado y otros.
ObjetivoDeterminar el impacto socioeconómico de la artritis reumatoide (AR) sobre costos en el contexto de los gastos catastróficos y el empobrecimiento.
Pacientes y métodosSe trata de una cohorte anidada en un estudio transversal y multicéntrico sobre el costo de la AR en los hogares mexicanos con cobertura parcial, completa o privado de salud. Los gastos catastróficos se definieron como aquellos que ocupaban > 30% del ingreso total del hogar. Empobrecimiento se definió como los hogares que no podían pagar la canasta básica de alimentos de México (CBA).
ResultadosSe incluyeron 262 pacientes con un ingreso familiar promedio mensual (dólares americanos) de $ 376 (0-18,890.63). En total, el 50,8%, 35,5% y 13,7% de los pacientes tenían cobertura médica parcial, completa o privado, respectivamente. El costo anual de la AR fue de $ 5,534.8 por paciente (65% los costos directos, el 35% indirecto).La AR generó gastos catastróficos en el 46,9% de los hogares, que en el análisis de regresión logística se asociaron significativamente con el tipo de cobertura de salud (OR 2,7, IC 95% 1.6 a 4.7) y la duración de la enfermedad (OR 1,024, IC del 95% 1.002-1,046). El empobrecimiento se produjo en el 66,8% de los hogares y se asoció con gastos catastróficos (OR 3,6, IC 95% 1.04 a 14.1), los altos puntajes del cuestionario de Evaluación de Salud (OR 4,84 IC 95%: 1,01 a 23,3), y el nivel socioeconómico bajo (OR 4.66, IC 95%: 1.37-15.87).
ConclusiónEl costo de la AR en los hogares mexicanos, en particular los que no tienen cobertura de salud completa lleva a los gastos catastróficos y el empobrecimiento. Estos hallazgos podrían ser los mismo en los países con sistemas de salud fragmentados.
Rheumatoid arthritis (RA) is a chronic inflammatory rheumatic disease affecting 0.5–1.0% of the population in some developed countries1 and 1.6% in the Mexican population.2 Short and long-term consequences of RA include chronic pain, impaired functioning,3 significant comorbidity, and reduced life expectancy.4 The cost of RA in some European countries has been estimated in €45.3 billion and in the United States of America (USA) in €41.6 billion.5 Interestingly, the economic burden caused by the disease in the population is important6–16 and paradoxically is high in countries with low gross domestic product (GDP).17 Nevertheless, there is a paucity of information from developing countries, particularly those in which the health care system is fragmented and diverse.
In México, the state covers ∼47% of the population with full and ∼49% with partial health care services by means of institutions of social security and the public health care system. Affiliates to the former are provided with all health care services and resources, including medications, whereas patients attending the latter rely on out-of-pocket expenses (OPEs) to cover most of the cost of their medical care.18–21 In the year 2000, 52% of the cost of health in México – which represented 5.8% of the GDP, corresponded to OPEs; public finances covered 46% and health care insurance companies 2%.19,20 It is estimated that 25% of RA disease direct cost in México corresponds to OPEs.21
OPEs are linked to catastrophic expenses and household impoverishment,18–22 yet the information on its effect in rheumatic diseases is scarce. It is remarkable that as consequence of RA, 2.4–19.2% of the household income is expended as OPEs in the USA.23 Impoverishment ranges from 12.3% to 51.3% households and relates to low family income, severe disease, and poor health insurance coverage.23 The USA and Mexican health care systems are alike at some extent. Both systems are fragmented in various types of coverage, but a variable proportion of individuals, usually those with the lowest income have no health coverage at all and rely on OPEs to cover medical costs. OPEs and their consequences – catastrophic expenses and impoverishment – may negatively influence patient's compliance, therapeutic adherence, and indeed RA outcome. Since the advent of biologic disease-modifying anti-rheumatic drugs (DMARDs) as part of the treatment of RA, the cost of the disease has notably increased.5 While developed nations may increment the budget fraction of GDP to cover the cost of RA,17 the situation in developing countries is critical. Neither health care dedicated GDP budget nor OPEs are enough to cover the cost of the disease.
In this context, we have investigated the burden of RA in households, particularly catastrophic expenses and impoverishment level across the Mexican health care system.18–22 In the best scenario, the results of this study would influence local policies to take measures to provide the whole population with RA with full health care. In addition, they may also facilitate the recognition and understanding of the consequences of RA in countries with complex health care systems and limited resources for the medical care of patients with such disease. In this sense, we approached the consequences of RA in a deeper form, far beyond that the solely description of OPEs we made previously.21
Subjects and methodsThis is a cross-sectional, multicenter cost-of-illness study with a prevalence-based, cost-estimated with the person-based approach of the baseline data of a cohort of patients with RA. OPEs data from the original cohort, including ankylosing spondylitis and gout have been already reported.21 The RA24 cohort consisted of consecutive outpatients with disease onset >18 years of age attending 11 institutional and private centers in five major cities. The Institutional Review Board at each center approved the study's protocol and patients agreed their participation in the study by signing an informed consent. The centers and patients that participated in the study were proportionally representative of each of the different health care systems in México.21 Information was collected from 2003 to 2005.
In brief, the Mexican health care system consists of several vertically integrated providers covering all different segments of the population.19 This study considered the three most important health care systems in the country:
- (1)
The full health care coverage system, which embraces institutions of social security that provide health care services, maternity leave, work disability, and retirement plans to wage-earners from the formal sector, their beneficiaries, and dependents. This system is financed by the federal government as well as by contributions from employees and their employers. The amount allocated to these institutions per family is almost two-thirds higher than that allocated by the public sector. The type and scope of services provided by institutions of social security depend on the availability of the resources. Around one-half of the Mexican population (55 million inhabitants in 2004) is covered by this system.
- (2)
The public health care system, which depends on the Ministry of Health, provides partial health care coverage to the population that is not covered by institutions of social security. It is a decentralized system financed and administered by the federation and governments of the states. Despite the fact that people have to pay for this type of care, costs are significantly lower than those of private health care services. Unfortunately, medications, paid sick days, disability, retirement plans, or copayments are not included among the benefits of such health system.
- (3)
The private health care system, a non-regulated sector in which users must pay directly for the services provided or less frequently through private insurance companies – usually very costly. Only 3% of this system includes collective plans, for which funds come from the employees having the possibility of deducting the cost of premium price as a taxable income.18,22
Demographic variables included age, sex, education level, and marital condition. Patient's work status included the following categories: unemployed, self-employed, and formally employed, disabled, retired, student, and housewife. We determined the total household income, housing characteristics, and whether the patient and its family owned, hired, or temporarily inhabited the property where they lived. We investigated the characteristics of medical care, including private insurance coverage, network support, and medical and non-medical direct costs in the last six months.25 Clinical variables included disease duration (interval between onset of symptoms and RA diagnosis), tender and swollen joint counts, erythrocyte sedimentation rate, and the disease activity score-28 (DAS-28).26 We also evaluated patient's well-being status, functioning, and health related quality of life with the Mexican validated versions of the Health Assessment Questionnaire-Disability Index (HAQ-DI)27 and the short-form (SF-36) questionnaire.28 Finally, we also assessed coping29 and co-morbidity.
OPEs were calculated through a micro-costing analysis of health care related patient's expenses. Cost components of healthcare and related resources, production losses, and intangible burdens were identified. Thus, we estimated the direct medical costs (physician consultations, hospitalization, medication, alternative therapies as well as laboratory and auxiliary tests), the direct non-medical costs (transportation and meals related to medical care), and the indirect costs (work disability, home care, loss of income at home) as consequence of RA and its comorbidities within the last six months. The patient, economically supporting relatives, health care institutions, and drug stores (pharmacies) provided the information for this analysis. Indirect costs were always obtained from the patient and his relatives. With information provided by patients and households having partial health care coverage or private medical care, and pharmacies as well as data from health institutions taking care of patients with full health care coverage, we calculated RA direct costs. Because we did not measure production losses as consequence of housework (unpaid productive work), we inferred housewives earned one minimum wage. Costs were converted from Mexican pesos into US Dollars for December 2005 and expressed throughout the paper as that (1 US Dollar=10.64 Mexican pesos; non-adjusted for purchasing power parities).30
Catastrophic expenses referred to health expenses totaling >30% of the family income and their calculation was made according to Torres and Knaul.31 Thresholds at 40%, 50%, and 60% were calculated as well. The poverty line was established according to the Basic Food Basket (BFB) threshold in México32–33 and the Organ for Economic Co-operation and Development (OECD) definition.22 The BFB definition of impoverishment was the household inability to cover the BFB average cost (approximately $536.2).32,33 The OECD definition of poor people referred to household income 60% below the national average (approximately $139.8).22 In addition, we calculated the household socio-economic status (SES) by using the following variables: head's of the family education level, dwelling characteristics, home overcrowding, and water sewer services.34 SES data were presented as a global score ranging from 0 to 12 where low scores corresponded to low SES.
Statistical analysisSocio-demographic, economic, and patient's clinical characteristics in each type of health care system were compared by means of descriptive statistics. Differences across the three different types of health care systems were tested with one and two-way analyses of variance (ANOVA) for continuous variables and chi-square or Kruskal–Wallis tests for ordinal, nominal, or categorical variables. We performed univariate and multivariate analyses and checked out the colinearity of independent variables. In the linear regression analysis, catastrophic expenses, total OPEs, and poverty level were considered dependent variables whereas the demographic, clinical, and socioeconomic features were regarded as independent. We also built some logistic regression models in which the presence of catastrophic expenses was regarded as the dependent variable and socio-demographic, clinical, and economic features were considered independent.
ResultsThe study included 262 patients (89.3% females) with a mean (standard deviation) age of 42.7 (13.6) years and median (range) disease duration of 17 (3–72) months (Table 1). The median household income was $376 (0–18,890.63) per month; 74.9% of the people earned ≤$244.0. Twenty-seven (10.3%) patients were off-medications, 170 (64.9%) were on non-steroidal antinflammatory drugs (NSAIDs), 71 (27.1%) on glucocorticoids, 65 (24.8%) on DMARDs monotherapy, 170 (64.9%) on DMARDs combinations, and only 17 (6.5%) on biologic therapy. Remarkably, 145 (55.3%) of the patients did not take all medications prescribed by their physicians because they could not afford their cost (85%) or because they faced institutional shortage (15%).
Demographic, economic, and clinical characteristics of patients with rheumatoid arthritis (n=262) according to the different types of health care coverage.a
| Variable | Partial coverage (n=133) | Full coverage (n=93) | Private coverage (n=36) | Pb |
| Females, n (%) | 123 (92.5) | 84 (90.3) | 27 (75) | 0.01 |
| Age, years | 42.9 (12.6) | 45.2 (14) | 46.14 (17) | 0.3 |
| Disease duration, years | 22.23 (17) | 23.19 (18) | 19.69 (15) | 0.6 |
| DAS28 | 3.1 (1.8) | 3.3 (1.8) | 3.5 (1.9) | 0.5 |
| HAQ-DI | 0.95 (0.79) | 1.04 (0.88) | 1.30 (0.89) | 0.09 |
| SF36 physical component score | 48.8 (22) | 49.7 (23) | 42.8 (24) | 0.3 |
| SF36 mental component score | 52.7 (20) | 58.5 (20) | 55.5 (20) | 0.11 |
| On DMARDs, n (%) | 120 (90.2) | 79 (84.9) | 32 (88.9) | 0.48 |
| On glucocorticoids n (%) | 39 (29.3) | 20 (21.5) | 12 (33.3) | 0.28 |
| Educational level, years | 8.2 (3.7) | 9.4 (3.7) | 11.5 (4.2) | 0.000 |
| Household socio-economic status | 7.79 (2.36) | 8.97 (1.99) | 9.83 (1.81) | 0.000 |
| Paid job, n (%) | 45 (34) | 40 (43) | 16 (44) | 0.3 |
| Sick leave, last year, n (%) | 22 (17) | 30 (32) | 17 (47) | 0.001 |
| Pay for all medications, n (%) | 55 (41) | 39 (42) | 19 (53) | 0.52 |
| Expenses in complementary therapiesc | 49.39 (187) | 94.21 (281) | 239.30 (697) | 0.001 |
| Private medical insurance coverage, n (%) | 1 (0.8) | 4 (4.3) | 14 (38.9) | 0.000 |
DAS28: disease activity score; HAQ-DI: health Assessment Questionnaire-Disability Index; DMARDs: disease-modifying anti-rheumatic drugs.
In all, 50.8% of the patients had partial and 35.5% full health care coverage whereas 13.7% relied on private medical care (Table 1). There was a trend of less severe and less active disease in the former group and the contrary on the latter, but regarding educational and economic variables the group of patients with partial health coverage was certainly below the two other groups.
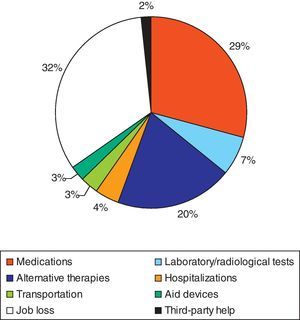
Cost analysisThe mean annual direct and indirect estimated costs for RA were $3,599±6,621 and $1,409±4,099, respectively (Fig. 1). Indirect costs corresponded mostly to job loss or to third-party help. Direct medical and non-medical costs differed across the health care systems (Table 2). The monthly median drug cost in social security institutions (full coverage system) was $28.2 (range 0.43–3719.9). The median OPEs for medications corresponded to $76.23 (range 0.47–1466.8). The median total institutional drug prescription (institutional and full coverage) cost per month was $55.1 (range 0.3–719.9). The mean total annual estimated cost per RA patient was $5534.8. Of these, 65% corresponded to direct and 35% to indirect costs (Fig. 1).
Cost analysis, out-of-pocket-expenses, catastrophic expenses, and impoverishment across health care systems in household with rheumatoid arthritis.a
| Partial coverage (n=133) | Full coverage (n=93) | Private coverage (n=36) | p | All patients (n=262) | |
| Annual directmedical and non medical cost | |||||
| Mean (SD) | 2,775 (3,801) | 3,787 (8,040) | 6,521(10,047) | 0.007 | 3,599(6,621) |
| Median (range) | 1,756 (12-19,254) | 744 (11-58,827) | 2,516 (32-51,873) | 1,515 (11-58,827) | |
| Annual indirect medical cost | |||||
| Mean (SD) | 393(1,372) | 1,860 (4,226) | 4,296 (7,970) | 0.001 | 1,409 (4,099) |
| Median (range) | 0 (0-10,150) | 0 (0-23,684) | 0 (0-33,835) | 0 (0-33,835) | |
| Annual total cost | |||||
| Mean (SD) | 3,152(4,044) | 5,553 (9,105) | 8,797(12,645) | 0.017 | 4,653(7,578) |
| Median (range) | 1,794 (12-19,234) | 1,515 (22-58,827) | 5,051(90-52,519) | 1,950(12-58,827) | |
| Household incomepermonth Mean (SD) | 316 (240) | 648 (451) | 1,848 (3617) | 0.000 | 644.4 (1453) |
| OPEs | |||||
| OPEs per month, mean (SD) | 231.22 (317) | 315.6 (670) | 543 (837) | 0.017 | 299.9 (551) |
| OPEs, % of household income | 73% | 49% | 29% | 0.002 | 65% |
| >30%of household income dedicated to RA,n (%) | 86 (64.7) | 20 (21.5) | 17 (47.2) | 0.000 | 123 (46.9) |
| Impoverished households | |||||
| BFB, n (%) | 118 (88.7) | 44 (47.3) | 13 (36.1) | 0.000 | 175 (66.8) |
| OECD, n (%) | 25 (18.8) | 3 (3.2) | 3 (8.3) | 0.001 | 31 (11.8) |
SD: standard deviation; OPEs: out-of-pocket-expenses; BFB: basic food basket; OECD: Organization for Economic Cooperation and Development.
The median household income was $376 (0–18,890.63) per month (Table 2) with an annual estimation of $4513 (0–226,688). In 123 (46.9%) patients, OPEs represented more than 30% of the household income. Thus, 64.7% with partial and 21.5% of patients with full health care coverage as well as 47.2% in the private health care system had catastrophic expenses as consequence of RA. According to SES,34 65% of households with catastrophic expenses were classified as extremely impoverished. Regardless of cut-off points, the proportion of households with catastrophic expenses and impoverishment was much higher in households with partial coverage than in those with full health care coverage (see Table 2). According to BFB definition of impoverishment,32,33 175 (66.8%) of the households, particularly those with partial coverage were impoverished. For the OECD,22 only 11.8% of the households would be considered poor (Table 2).
Association of OPEs and catastrophic expenses with demographic and clinical variablesThe variables that predicted catastrophic expenses in the logistic regression analysis were partial health care coverage (OR 2.7, 95%CI 1.6–4.7; p=0.000) and long disease duration (OR 1.024, 95%CI 1.002–1.046; p=0.031). Increased number of family members (>4) (OR 0.37, 95%CI 0.17–0.81; p=0.012) and household income (>$400) (OR 0.29, 95%CI 0.11–0.80; p=0.016) protected against catastrophic expenses. Interestingly, there were no variables significantly associated with impoverishment in the logistic regression models that considered BFB. In contrast, catastrophic expenses (OR 3.6, 95%CI 1.04–14.1; p=0.043); high HAQ score (OR 4.84, 95%CI 1.01–23.33; p=0.049) and low SES (OR 4.66, 95%CI 1.37–15.85; p=0.014) predicted impoverishment as defined by the OECD in our population.
DiscussionAs seen from the perspective of catastrophic expenses and impoverishment, the burden of RA in Mexican households found in this study was of great magnitude. Nearly 50% of households assigned >30% of their monthly income to cover the direct and indirect costs of the disease; moreover, for 37.4% of them, the proportion was over >50%. On the other hand, two-thirds of households were in a state of impoverishment according to BFB definition. The proportion of households reporting catastrophic expenses and falling below the level of impoverishment was higher among those with partial or private coverage than in those with full health care coverage. One possible interpretation of these findings could be that a high percentage of households would not be able to face RA as a health problem and in fact would fall below the impoverishment level as consequence of the disease.
Catastrophic expenses relate to OPEs, type of health coverage, family income, physical functioning, number of family members, and average age of the family. The factors that determined OPEs and catastrophic expenses as consequence of RA were low family income, lack of employment and health insurance, and low educational level; additional related factors were the number and composition of people living in patient's home and characteristics of the place of residence.18,20 Regardless of any disease in the family, the 2002 National Performance Assessment Survey (ENED)20 found catastrophic expenses in 3.89% (IC95% 3.61–4.19) of households, particularly in those with pregnant women, persons aged >60 years, or disabled individuals. Each of these situations led to impoverishment in 77%, 42%, and 52%, respectively.20 Finally, the risk of impoverishment was high among those already impoverished living in rural areas lacking health care insurance.18,20,31 At first glance, the factors leading to catastrophic expenses and impoverishment in RA differ from those in the general population. However, the characteristics of the two groups, RA and general population make comparisons unfair.
Remarkably, there is no information on catastrophic expenses generated by rheumatic diseases despite the fact that direct and indirect costs, including some referring to OPEs expenses have been the subject of numerous studies.4,23 We previously reported that OPEs represented 15% of household income and 26.1% ($610±302.2 per year) of the total cost of RA.21 Mean OPEs per year as consequence of RA in the USA was $1798±$3314.23 While 43.6% of USA patients had problems in paying their medical bills, this obligation represented a serious problem for 9.0% of the population with RA. According to the Health and Human Services, 51.3% of such population falls below the poverty line.23 In our study, 88.7% of householders with partial health coverage fall below the impoverishment level. Despite gross economical differences, the cost of RA in México and USA leads to high OPEs and impoverishment of the population that lacks full medical care coverage or insurance. In other countries, particularly those in the European Community, the cost of the disease is mostly covered by the state. In such circumstance, there is no way that any household would have catastrophic expenses as consequence of any disease.
The annual total cost per patient with RA in this study (including direct and indirect costs) was $4653.16. Medications represented 29% of the total cost, which is in the 8–26% range reported in other studies.35–40 Remarkably, unemployment was high among RA patients (61.5%), as well as among the members of their family in the age years of economic potential (44.4%). Unemployment rate in our country is approximately 4%, but despite the National Institute of Statistics and Geography (INEGI) officially states that 95.97% of the economically active population has a paid job, 66% of the jobs are informal and therefore do not generate social benefits. Around 60% of the population earns between 1 and 3 minimum wages and 64% have no access to health services.
Based on the prevalence of RA in our country (0.7–2.8% out of 107,029,000 inhabitants),2 the estimated annual cost of the disease could be in the range of $44,099 million to $176,397.6 million. Considering that in 2005, health care expenses represented 6.5% ($615,869.2 million) of GDP, the annual cost of RA in México would represent 7.2–28.6% of the total health care expenses per year. Despite the fact that the Mexican government has allocated some financial resources for a group of nine diseases causing leading to catastrophic expenses,41 none of the rheumatic diseases including RA are considered in such group.
The limitations of the study include some selection bias to more severe cases, which may be expected among patients attending specialized departments. However, most patients had less than five years of symptoms and severity might be mostly resulted from active disease and not from severe structural changes at the time of the study. In addition, we included patients attending private practice, in which disease severity may be lower. Interestingly, the proportion of patients included in the study corresponded very well to the proportion of individuals in each segment of the health care system in the country, which suggest representativeness of our sample. There was a general under-representation of biologic agents in our sample: only 2% of all patients were on biologic therapy. The use of biologic agents has grown year per year, but access to this type of therapy is mostly limited to that segment of the population with complete full coverage or private medical insurance and not by those with partial medical coverage or no coverage at all. While those with full medical coverage do not incur in any cost to get them, those in private practice and those with private insurances usually have catastrophic expenses.
In conclusion, we have shown that the cost of RA has an important socioeconomic impact in Mexican households as seen through the magnitude of catastrophic expenses and impoverishment resulting from OPEs. The households lacking full medical coverage were those particularly affected by the cost of the disease. In this sense, it is expected that the impact of RA could be approximately the same in countries with fragmented health care systems. After all, an important segment of the population and specifically of patients with RA will not be able to comply with long-term therapeutic indications and indeed access to new costly medications.
Financial supportThis work is supported by a research grant from the National Council of Science and Technology (CONACYT), Project No. 69765.
Conflicts of interestThe authors have no conflicts of interest to declare.
REUMAIMPACT Group: Aceves FJ, Álvarez-Hernández E, Bernard-Medina AG, Boonen A, Burgos-Vargas R, Carlos F, Casasola-Vargas J, Espinoza-Villalpando J, Esquivel J, Flores D, Garza M, Goycochea-Robles MV, Hernández-Garduño A, Peláez-Ballestas I, Ramos-Remus C, Rodríguez J, Shumsky C, Skinner-Taylor C, Teran-Estrada L, Vázquez-Mellado J, and Ventura-Ríos L.