Sjögren's syndrome (SS) is a systemic autoimmune disease characterized by the infiltration of lymphocytes into exocrine glands, resulting in the typical sicca symptoms. Unlike adults, primary SS is a very rare condition in childhood, and the risk of malignancy in juvenile SS (JSS) has not been defined.
We report the detection of extranodal marginal zone B-cell lymphoma (EMZL) occurring in two children with SS. Fine needle aspiration of the salivary glands (SG) showed nonspecific findings that led to delayed diagnosis of SS. The diagnosis of B-cell lymphoma associated with JSS was based on morphologic and immunohistochemical staining done during the biopsy.
To highlight awareness of EMZL as a timely and appropriate update of an unusual complication in children with SS.
El síndrome de Sjögren (SS) es una enfermedad sistémica autoinmune caracterizada por la infiltración de linfocitos en glándulas exocrinas, provocando el típico síndrome seco. A diferencia de los adultos, el SS es una afección rara en niños, y el riesgo de malignización no ha sido descrito.
Describimos la detección de linfoma B de la zona marginal extranodal de tejido linfoide asociado a mucosa (linfoma MALT) en 2 niños con SS. La aspiración con aguja fina de las glándulas salivares (SG) mostró hallazgos inespecíficos que retrasaron el diagnóstico de SS. El diagnóstico de linfoma B asociado a SS juvenil se realizó con base en los hallazgos morfológicos e inmunohistoquímicos detectados en biopsia.
Hay que tomar conciencia de que un linfoma B puede acontecer en el curso de un SS como una complicación inesperada en niños, principalmente para realizar una derivación correcta a oncología.
Sjögren's syndrome (SS) is a systemic autoimmune disease characterized by the infiltration of lymphocytes in exocrine glands.1 SS is a rare condition in childhood and ocular and oral symptoms are uncommon.2,3 The risk of lymphoma development during the course of SS has been described in adults, but it is extremely rare in childhood.1 We report the association of lymphoma to SS in two children, as an unexpected complication.
Case reportsCase 1A teenager followed since the age of 14 years for intermittent swelling of the knee with negative image and laboratory investigations. She developed SS at the age of 18 year showing intermittent swelling of parotid glands, positive RF, antinuclear antibodies (ANA) and anti-SSA antibodies, elevated erythrocyte sedimentation rate (ESR, 25mm/1h), but normal serum level of cryoglobulins, IgG4 and complement. The Schirmer test and serologic testing for virus were negative. The minor SG biopsy showed focal lymphocytic sialadenitis but the histopathologic diagnosis did not meet SS-criteria. Her follow-up showed the detection of a nodule on the hard palate with the diagnosis of B-cell lymphoma based on morphologic and immunohistochemical staining (CD20+ B cells) from nodule biopsy. Gastrointestinal endoscopy showed chronic gastritis (Helicobacter pylori negative). The computerized tomography (CT) of neck, chest, abdomen, and pelvis, showed no additional evidence of disease. Recently a new episode of right parotitis along with a biopsied cervical lymph node confirmed persistent lymphoma after 6 months of rituximab.
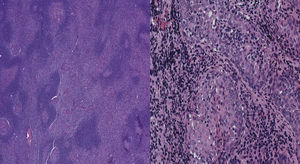
Case 2A 16-year-old boy presented with intermittent painless cervical lymphadenopathy and bilateral parotid swelling for more than 5 years. Neck CT demonstrated enlargement of the parotids. A fine needle aspiration showed a benign lymphoid tissue with no evidence of malignancy. Laboratory data showed an increased ESR (122mm/h). Histopathology analysis showed infiltration of the salivary gland by a lymphocytic proliferation forming confluent nodular masses and follicular hyperplasia of the attached lymph nodes, indicative of a lymphoid malignancy (Fig. 1). Immunohistochemical stains demonstrated sheets of CD20+ B cells that were negative for CD5, CD43, and cyclin-D1, confirming B-cell clonal proliferation (Fig. 2). CD10 and BCL-6 stains highlighted germinal centers which were negative for BCL-2. A Ki-67 stain showed numerous positive cells within and between germinal centers (20–30% cells). Parotidectomy and radiotherapy was performed. Serologic testing revealed only a remote infection by CMV and EBV. Immunological tests showed positive RF, ANA, anti-SSA and anti-SSB antibodies. Despite only vague sicca symptoms, ophthalmology exam revealed corneal and conjunctival erosions, and the diagnosis of SS was made. Hydroxychloroquine and rituximab were started. There was no evidence of tumor recurrence after >14 months follow-up.
In childhood, recurrent parotid swelling is the most common hallmark of SS, usually proceeding to sicca symptoms as in our patients.2 Diagnostic criteria are similar to those proposed in adults3; however, it showed low sensitivity and histological findings of the minor SG criteria (>1 focus of 50 lymphocytes/4mm2) are often negative in children.4 It explains delayed diagnosis in the case 1, despite exclusion of infectious diseases at onset. The sensitivity increases by using a lesser score in childhood.5
The occurrence of lymphoma in SS is extremely rare in childhood. EMZL is a low-grade lymphoma that usually occurs in the setting of a benign myoepithelial sialadenitis (MESA) and biopsy confirms the diagnosis. Clonal expansion to EMZL is believed to be triggered by chronic immune stimulation in the context of a preexisting inflammatory response from autoimmune diseases or chronic infections, amyloidosis, some translocations and common variable immunodeficiency.6–9 Differences in Rituximab response might be a higher pretreatment number of CD20+ B cells/mm2 parotid gland parenchyma.10
ConclusionSS requires child-specific criteria to role out lymphoma as unusual complication in children, particularly for timely and appropriate referral.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Confidentiality of dataThe authors declare that they have followed the protocols of their work centre on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflict of interestNone.