Schwannomas, also known as neurilemmomas or Schwann cell tumors, are benign tumors originating from Schwann cells of the peripheral nerve sheath, occurring more frequently along the brachial plexus and spinal nerves.1–4 Despite being the most common tumors of the peripheral nerve sheath, they are rarely encountered and diagnosis is often delayed.2,4 These entities can mimic rheumatologic conditions such as synovial cysts, bursitis or ganglions.
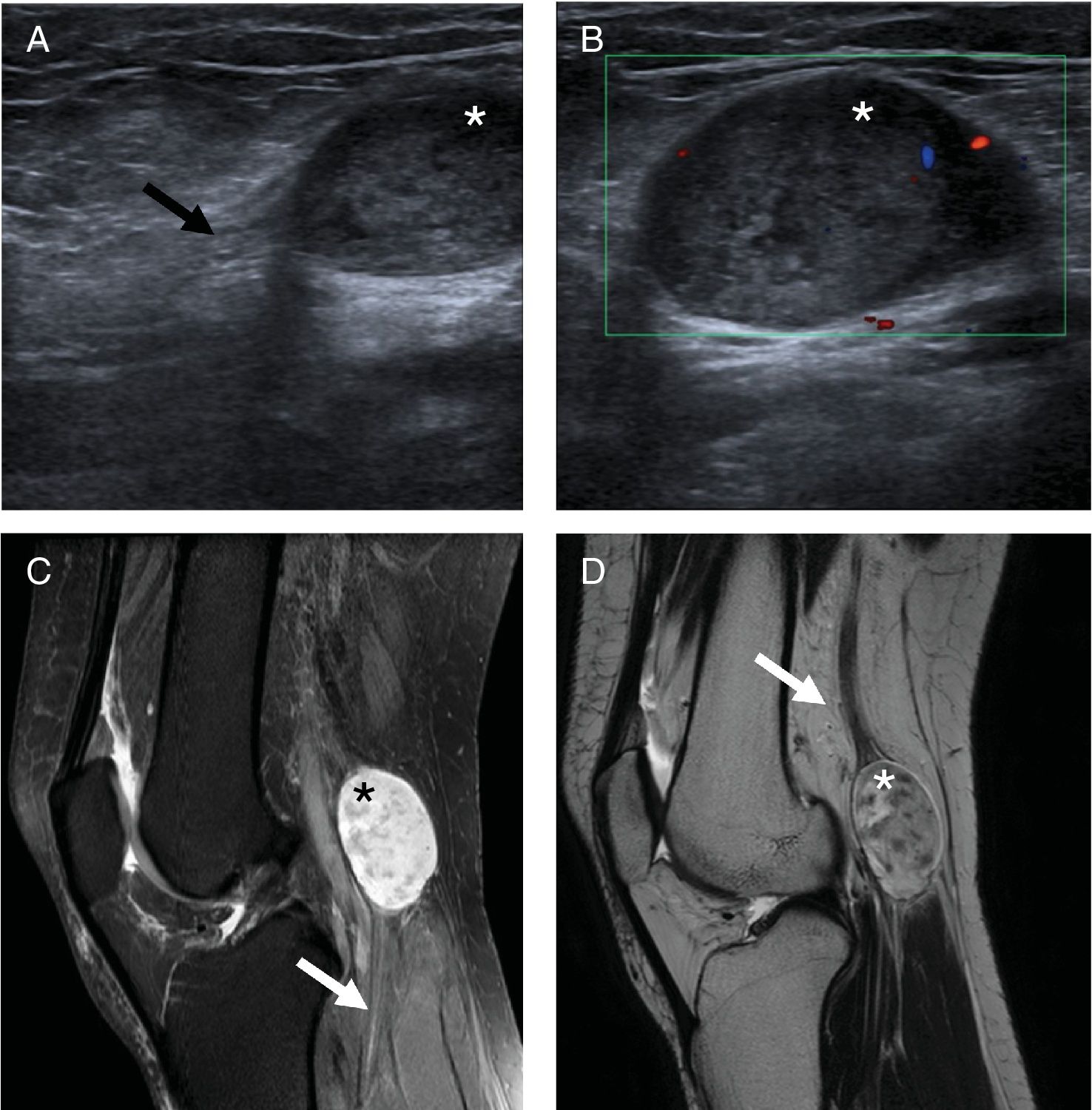
A 36-year-old healthy woman (Fig. 1) presented with a five-year history of a slowly enlarging mass in the popliteal region, with no previous history of trauma. A mobile and solid mass was palpable at the popliteal region evocative of a Baker's cyst, although the Foucher's sign was not present on examination. The patient was referred for ultrasound-guided aspiration and corticosteroid infiltration. However, ultrasound (US) documented a 29.9×25.5mm heterogeneous solid mass in the popliteal region, originating from the tibial nerve. Magnetic resonance imaging (MRI) showed a homogeneous low intensity in T1-weighted images and heterogeneous high intensity in T2-weighted images, suggestive of a tibial nerve schwannoma.
Ultrasound (A, B) and MRI (C, D) images of the knee depicting a well-defined solid mass (*) localized in the popliteal region, originating from the tibial nerve (arrows), with a heterogeneous structure with low intensity MRI-signal on T1 sequences and high intensity on DP SPAIR (C) and T2 sequences (D).
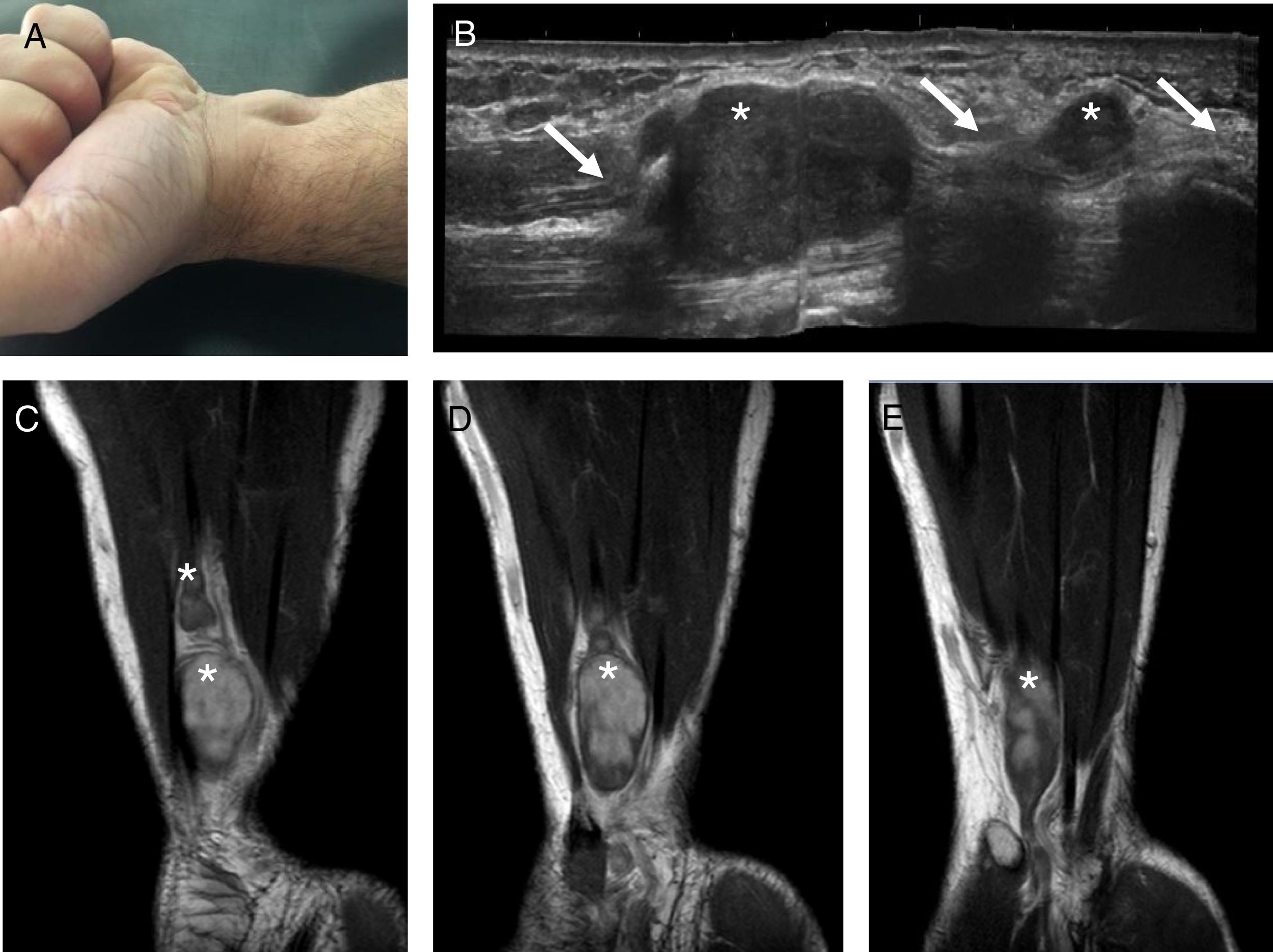
A 47-year-old healthy male (Fig. 2) presented with a one-year history of an enlarging mass on the distal part of the anterior aspect of the forearm and wrist, with no associated trauma or inflammatory signs. The clinical diagnosis was of a synovial cyst and the patient was referred for US-guided aspiration. US identified well-defined masses (the biggest with 26×11mm) originating from the cubital nerve. The diagnosis of cubital nerve schwannoma was confirmed by MRI, which documented 5 nodular masses originating from the cubital nerve.
Both patients were referred to but refused surgical excision of the tumors.
These cases highlight the importance of considering schwannomas in the evaluation of patients with nodules suggestive of synovial cysts, both on physical examination and when performing US or US-guided techniques. In both cases, US was crucial for the correct diagnosis these entities.
Conflict of interestsThe authors declare no conflict of interest.