The aim of the present study was to describe the ultrasound (US) findings in patients with rheumatoid arthritis (RA) in clinical remission, and to evaluate the ability of power Doppler (PD) US to reclassify disease activity in these patients.
Material and methodsWe included consecutive patients with RA according to 2010 American College of Rheumatology/European League Against Rheumatism criteria, who were in clinical remission by the Disease Activity Score (DAS28<2.6). Twenty joints of both hands were assessed by US. PD signal was evaluated on a semi-quantitative scale from 0 to 3. Three different US-modified DAS28 (US-DAS28) were constructed, replacing the clinical swollen joint count by the PD US joint count using PD score ≥1, ≥2 or ≥3, respectively.
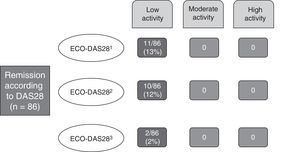
ResultsEighty-six patients were included. Twenty-three (26.7%) patients had at least one joint with abnormal US-positive PD signal. Thirteen percent of patients were reclassified to low disease activity by applying the US-DAS28 when joints were considered active with a PD signal ≥1; 12%, when a PD signal ≥2 was considered, and 2% of the patients were reclassified when a PD score of 3 was considered. No patients were reclassified to a level of moderate or high activity applying US-DAS28.
ConclusionsAlthough around a quarter of patients with RA in clinical remission showed PD US features indicating residual activity, only a small percentage were reclassified to a state of low activity and none to a level of moderate or high activity, applying the proposed US-DAS28.
Describir los hallazgos ecográficos en pacientes con artritis reumatoide (AR) en remisión clínica y evaluar la capacidad de la ecografía con Doppler de poder (DP) para reclasificar la actividad de la enfermedad en este grupo de pacientes.
Material y métodosSe incluyeron pacientes consecutivos con diagnóstico de AR (criterios ACR/EULAR 2010) en remisión clínica por DAS28 (<2,6). Se evaluaron mediante ecografía 20 articulaciones de ambas manos. La señal DP fue evaluada mediante una escala semicuantitativa de 0 a 3. Se construyeron 3 índices clínico-ecográficos que denominamos ECO-DAS28 1, 2 y 3, donde el recuento de articulaciones tumefactas evaluadas clínicamente fue reemplazado por el recuento de articulaciones con señal DP positiva grado ≥1, ≥2 o 3, respectivamente.
ResultadosSe incluyeron 86 pacientes, de los cuales 23 (26,7%) tuvieron al menos una articulación con señal DP positiva. Un 13% de los pacientes fueron reclasificados hacia baja actividad de la enfermedad aplicando el ECO-DAS28 cuando se consideraron activas las articulaciones con señal DP grado ≥1, el 12% cuando se consideró actividad una señal DP≥2 y el 2% de los pacientes cuando se consideró la señal DP igual a 3. Ningún paciente se reclasificó a un nivel de moderada o alta actividad.
ConclusionesA pesar de encontrar actividad inflamatoria residual por ecografía en aproximadamente un cuarto de los pacientes con AR en remisión clínica, solo un bajo porcentaje fue reclasificado a un estado de baja actividad de la enfermedad y ninguno a un nivel de moderada o alta, aplicando los ECO-DAS28 propuestos.
In recent decades, musculoskeletal ultrasound has become a highly useful tool in the evaluation and management of patients with distinct rheumatic diseases, especially those with a diagnosis of rheumatoid arthritis (RA).1,2
Ultrasound constitutes an ancillary tool in physical examination and, as this method is highly sensitive in the detection of inflammatory processes, it provides greater information on the degree of joint involvement,3–5 even in patients in clinical remission. Synovitis detected by ultrasound, rather than by a clinical test or in asymptomatic patients with a diagnosis of RA, regardless of the disease activity score, is referred to as “subclinical synovitis”. Ultrasound has been shown to be useful in the detection of subclinical inflammatory changes in the joints.3,6–9 However, it is not yet clear whether these findings should lead to a modification of the therapeutic management.10–12
A number of studies have demonstrated the importance of ultrasound as an independent predictor of radiographic progression and the development of bone erosions affecting joints.7,9,13–15 The presence of the power Doppler (PD) signal would always have a role in the prediction of relapse in RA patients who are in clinical remission.14,16–18
In the near future, the “treat-to-target” strategy guided by ultrasound could be a valid alternative for improving the treatment and prognosis of patients with RA.19–22
The purpose of the present study was to describe the ultrasound findings in RA patients in clinical remission and evaluate the capability of PD ultrasound for reclassifying the level of the activity of RA measured by the Disease Activity Score in 28 joints (DAS28) in this group of patients.
Material and MethodsPatientsWe included 86 consecutive patients from the outpatient clinical practice of the rheumatology department of Hospital Italiano de Buenos Aires, Argentina, who met the 2010 American College of Rheumatology/European League Against Rheumatism (ACR/EULAR) criteria23 for the diagnosis of RA and who were in clinical remission in accordance with the criteria of their treating physicians and had a DAS28<2.6.24
During the first visit to the rheumatology department, the clinical and demographic data of the patients were recorded, after which they underwent an ultrasound evaluation of both hands.
Clinical ExaminationThis was carried out in every case by experienced rheumatologists. The tender and swollen joint counts were determined,28 and the visual analog scale (VAS) was employed to establish the disease activity as assessed by the patient. The DAS28 was calculated utilizing the erythrocyte sedimentation rate.24
Ultrasound EvaluationThis was performed in every case by the same rheumatologist, who had extensive experience in the technique—and who was blinded to the clinical data of the patient—on the same day as the clinical evaluation. This was carried out with a MyLab®70 ultrasound system (Esaote) equipped with a 6–18MHz multifrequency linear transducer. The ultrasound technique was done in accordance with the EULAR recommendations.25 Bilateral evaluation was performed in the following joints of the hands and carpi (a total of 20): carpus, first to fifth metacarpophalangeal joints and second to fifth proximal interphalangeal joints. The carpus and metacarpophalangeal joints were evaluated using a dorsal approach and the proximal interphalangeal joints employing a palmar approach. The carpus was considered to be a single unit, which could affect the radiocarpal and/or intercarpal recess. We evaluated the presence of joint capsular distension (JCD) on gray-scale images, either due to the presence of fluid and/or synovial hypertrophy, in accordance with the definitions of the OMERACT group.26
The degree of abnormal intra-articular vascularization was determined by means of the PD technique, utilizing a semiquantitative scale from 0 to 3 (score of 0: absence of PD signal; score of 1: presence of a single signal; score of 2: presence of 1 or more confluent signals that occupy less than 50% of the intra-articular area; score of 3: signal occupying more than 50% of the intra-articular area). The configuration of PD parameters agreed with the recommendation of experts.4,27
We constructed 3 indices of clinical-ultrasonographic activity that we refer to as ECO-DAS28 (DAS28 modified by ultrasound: ECO-DAS281, ECO-DAS282, ECO-DAS283). In the original formula of DAS28, we replaced the clinical swollen joint count with the ultrasound results of the intra-articular PD signal. In ECO-DAS281, we considered to be swollen any joint with a PD signal≥1, in ECO-DAS282, any joint with a PD signal≥2 and in ECO-DAS283, any joint with a PD signal grade 3. In the case of the 8 joints not assessed by ultrasound that are included in the DAS28 (shoulders, elbows, interphalangeal joints of the thumbs and knees), we took into account the data from the clinical evaluation.
The study was performed in accordance with the guidelines of the Declaration of Helsinki and the protocol was approved by the institutional ethics committee of research protocols for application. All of the patients gave their informed consent prior to inclusion in the study.
Statistical AnalysisWe utilized the mean and standard deviation (SD) to express the continuous variables, and number (n) and percentage for the categorical variables. The calculation of the ECO-DAS28 was done with the same mathematical formula employed for DAS28.24 For the correlations between the clinical and ultrasonographic activity indices, we utilized the Spearman test.
ResultsWe included a total of 86 patients, 65 (75%) of whom were women; the mean age (SD) was 58 years14 and the mean disease duration (SD) was 7 (7.9) years. The demographic and clinical characteristics of the patients are shown in Table 1.
Clinical and Demographic Characteristics of the Patients.
| Characteristics | n=86 |
|---|---|
| Women, n (%) | 65 (75) |
| Age, mean (SD) | 58 (14) |
| Disease duration, mean (SD) | 7 (7.9) |
| Treatment with DMARD, n (%) | 71 (82.5) |
| Treatment with biological therapy, n (%) | 25 (29) |
| Positive RF, n (%) | 55 (67) |
| Patients with at least 1 SJ, n (%) | 7 (8) |
| Patients with at least 1 TJ, n (%) | 10 (9) |
| DAS28, mean (SD) | 2.08 (0.39) |
| Patients in whom PD signal was detected, n (%) | 23 (26.7) |
| ECO-DAS281, mean (SD) | 2.15 (0.45) |
| ECO-DAS282, mean (SD) | 2.13 (0.45) |
| ECO-DAS283, mean (SD) | 2.07 (0.39) |
DAS28, Disease Activity Score in 28 joints; DMARD, disease-modifying antirheumatic drug; ECO-DAS28, DAS28 modified by ultrasound; n, number; PD, power Doppler; RF, rheumatoid factor; SD, standard deviation; SJ, swollen joints; TJ, tender joints.
In the clinical evaluation, only 7 patients had swollen joints: 6 of them with involvement of only 1 joint and the remaining patient had 2 inflamed joints. The mean (SD) of DAS28 was 2.08 (0.39).
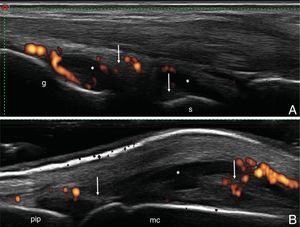
Twenty-three patients (26.7%) had at least 1 joint with a positive PD signal. Of a total of 1720 joints evaluated by ultrasound, 36 (2%) showed an abnormal increase in vascularization in studies done using PD. The PD signal most frequently found in these patients was grade 1, occurring in 70% of the cases (25 joints) (Fig. 1).
Applying ECO-DAS281, with respect to the level of disease activity, we reclassified 11/86 (13%) of the patients, in addition to 10/86 (12%) with ECO-DAS282 and 2/86 (2%) with ECO-DAS283, respectively. In every case, the patients were reclassified toward a level of low disease activity and none of them toward moderate or high activity, in accordance with the new DAS28 value modified by ultrasound (ECO-DAS28) (Fig. 2).
We found an excellent correlation between DAS28 and the diverse ECO-DAS28 proposed (Spearman's rho for ECO-DAS281: 0.90; for ECO-DAS282: 0.91 and for ECO-DAS283: 0.95, respectively; P<.001) (Fig. 3).
(A) Carpus. Dorsal longitudinal plane. Capsular distension in the radiocarpal and intercarpal joints recesses, both with synovial fluid (*) and areas of synovial proliferation (arrow), with increased vascularization by power Doppler (grade 2). (B) Metacarpophalangeal joint. Dorsal longitudinal plane. Joint capsular distension with areas of synovial fluid (*) and areas of synovial proliferation (arrow), with increased vascularization by power Doppler (grade 2). l, large; mc, metacarpophalangeal joint; pip, proximal interphalangeal joint; r, radiocarpal; s, semilunar.
The present study proposes a combined clinical-ultrasonographic index for the evaluation of disease activity by DAS28 in patients with RA. Our objective was to evaluate the disease activity by DAS28, replacing the clinical evaluation of swollen joints with their ultrasound evaluation. In this study, we randomly selected only the joints of the hands and carpi, for the purpose of reducing the time and costs of the ultrasound examination.
The percentage of patients (26.7%) in whom we detected residual inflammatory activity, confirmed by the presence of a PD signal in the joint, was somewhat lower than that reported in earlier works. A meta-analysis by Nguyen et al. demonstrated the presence of subclinical synovitis with a positive PD signal in 44% of RA patients in clinical remission.17 Brown et al. showed, irrespective of the clinical criteria applied to define remission, that active inflammation was present by imaging techniques.3 In all, 73% of the patients in clinical remission had synovial hypertrophy in gray-scale images, and 43% had an increased intra-articular PD signal. The patients included in our study had few joints with positive PD signal and, in the great majority, they were grade 1. Our prevalence of nearly 30% is slightly lower than that reported in those articles, and this could be due to differences in the selection of the patients to be studied, to the different proficiency in the clinical evaluation for the detection of synovitis in distinct joints and to differences in the number and selection of the joints included in these studies.
Reclassification of the disease activity, utilizing the ECO-DAS28 indices, was observed in a small percentage of patients and, in every case, it was from a state of clinical remission toward a level of low disease activity and in no instance toward a level of moderate or high activity.
The present work has certain limitations that should be mentioned. In the first place, not all of the 28 joints included in the DAS28 underwent ultrasound evaluation. Thus, the presence of subclinical activity may have been omitted in certain joints. However, several ultrasound scoring systems involving a reduced number of joints have been found to have an excellent correlation with others that include a larger number of joints. Most of those scoring systems include the carpus and the small joints of both hands, which were examined in our study.28–30 These simplified systems have been validated in patients with active RA for the monitoring of their therapeutic response, although they have not been utilized in routine practice in patients in clinical remission. Naredo et al. compared different reduced ultrasound scoring systems in patients with RA in clinical remission.7 On evaluating a 44-joint count, they detected the presence of synovial hypertrophy in 87.8% of the patients with a DAS28<2.6 and in 81.8% with the Simplified Disease Activity Index (SDAI)<3.3. The PD signal was detected in 46.3% of the patients with a DAS28<2.6 and in 36.4% with the SDAI<3.3. These authors demonstrated that ultrasound evaluation in the carpus, second to fifth metacarpophalangeal joints, ankle, and second to fifth metatarsophalangeal joints was highly sensitive for detecting synovitis by gray-scale and by PD signal, compared with the ultrasound evaluation of 44 joints. Secondly, the cross-sectional design of the present study does not enable us to establish whether this reclassification of the patients, even with low frequency and toward a state of low disease activity, could be associated with future relapses or progression of the radiographic damage.13,14,16,31 Finally, although the ultrasound examination was carried out by a rheumatologist with extensive experience in the technique, the lack of an evaluation of intra- and interobserver agreement concerning the ultrasound findings could reduce the internal validity of the study.
Our study demonstrated that the joint inflammatory process, assessed by PD ultrasound in hands and carpi, was not useful for reclassifying patients in remission to a state of higher activity. The great majority of the patients remained in the same level of activity, indicating that, in these patients, ultrasound did not change the parameter most widely used in real-world practice for making therapeutic decisions, according to the treat-to-target recommendations.
In conclusion, the present report demonstrated residual activity detected by PD ultrasound in approximately a fourth of the patients with RA in clinical remission. This enabled the reclassification of the disease activity in a low percentage of these individuals, in every case toward a state of low disease activity. We consider that it would be very useful in this group of patients, to perform a prospective comparison of the utility of a multimodal index based on clinical-ultrasonographic monitoring with findings from an approach that focused on clinical monitoring. This may help to determine whether there are advantages to the use of ultrasound in the follow-up of patients with RA in clinical remission.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
FundingThe present report was financed by the Rheumatology Section of the Medical Clinic Department and Radiology Department of Hospital Italiano de Buenos Aires, Argentina.
Conflicts of InterestThe authors declare they have no conflicts of interest with respect to the present study.
Please cite this article as: Vergara F, Ruta S, Rosa J, Marín J, García-Mónaco R, Soriano ER. Valor de la ecografía con Doppler de poder en pacientes con artritis reumatoide en remisión clínica: ¿reclasificación de la actividad de la enfermedad? Reumatol Clin. 2018;14:202–206.