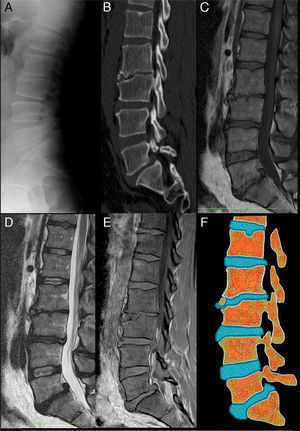
The patient was a 39-year-old farmer who had nothing remarkable in his clinical history. He presented with self-limiting, chronic, mechanical low back pain, without radiation, fever or systemic symptoms. Physical examination revealed only pain on palpation of the lumbar spinous processes and limited anterior dorsiflexion. Laboratory values, including serological findings and protein profile, were normal. A radiograph of the lumbar spine (Fig. 1A) showed an irregular sclerotic lesion in the epiphysis of lumbar 3 (L3). Lumbar computed tomography (Fig. 1B) showed irregularity, crush fracture and fragmentation preceding L3. Magnetic resonance imaging of the lumbar spine (Fig. 1C–E) revealed a limbus vertebra (LV) at L3, degenerative disc disease at L2–L4 and L5–sacral 1 (S1) and disc herniation at L3–L4 and L5–S1.
Limbus vertebra: (A) lateral radiograph of lumbar spine. The image shows the irregularity of the superior and anterior corners of the vertebral body at lumbar 3 (L3). The L2–L3 intervertebral space is narrowed. There are small anterior osteophytic formations at L2 and L4. The density of the vertebral bodies is conserved; (B) computed tomography with sagittal multiplanar reconstruction, in which the irregularity of the anterosuperior margin of L3 vertebral body can be seen in greater detail. Sclerosis can be observed both in the recessed vertebral endplates and around the osseous fragments separated from the rest of the bone. Listhesis can also be detected at L3–sacral 1 (S1) and Schmorl's node in the superior endplate at L1; (C) magnetic resonance imaging (MRI) of sagittal spin-echo T1-weighted (SET1) sequences. The intensity of the vertebral bodies is conserved and the osseous fragment separated from the L3 body has the same signal intensity has the rest of the bone; (D) MRI of sagittal spin-echo T2-weighted sequences. The findings complement what can be observed in the SET1 sequence. There is a decrease in height and signal of intervertebral discs at L2–L3, L3–L4 and L5–S1 in relation to dehydration in the setting of a degenerative disc disease. There is also a posterior central disc herniation at L5–S1, that migrated cranially, accompanied by listhesis; (E) MRI sagittal SET1 sequences in-phase and out-of-phase. In these sequences, the signal of the disc cartilage is high and bright. It can be seen how it is introduced between the osseous fragment and the foremost region of the superior L3 endplate; (F) drawing representing the changes observed in the images to the left. It can be seen that the L2–L3 intervertebral disc is introduced through the anterior surface of the L3 vertebral body. A Schmorl node can also be seen in the superior endplate of L1 and a protrusion of the L5–S1 disc, with a posterior central disc herniation, accompanied by listhesis at L5–S1.
The diagnosis was LV at L3 and listhesis at L5 with spondylolysis. The patient improved with conservative treatment (anti-inflammatory agents and muscle relaxants). Surgery was ruled out.
Limbus vertebra is a radiological finding. Its prevalence is unknown and its significance is uncertain. It is a bone defect that affects the vertebral body margin, which is the origin of this a triangular fragment with sclerotic borders (Fig. 1F). It is produced in the form of an intraosseous herniation of the nucleus pulposus through the vertebral ring apophysis, prior to the complete fusion of the vertebral body. Its pathogenesis is related to that of Schmorl's nodes and Scheuermann disease. The most common localization is the lumbar spine and it involves the anterosuperior corner, followed by the anteroinferior region. Posterior LV is less frequent, but has a more marked clinical and functional impact because the osseous fragments can move, thus narrowing the spinal canal.1,2
In our case, the radiographic image could lead to a diagnosis of fracture, inflammation, infection or tumor, making additional imaging studies necessary.
The question as to whether LV is a variant of normality is controversial. Although there is little available literature, the cases described refer to patients who complain of back pain, not healthy individuals. There appears to be a pathological significance associated with low back pain. Clinical and epidemiological research on this entity should be embarked on under a new approach.
Ethical DisclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflicts of InterestThe authors declare they have no conflicts of interest.
Please cite this article as: Carrasco Cubero C, Coelho Achega DG, Férnández Gil MÁ, Álvarez Vega JL. Lumbalgia mecánica como forma de presentación de vértebra limbus anterior. 2017;13:176–177.